
“One and a half” minimally invasive transforaminal lumbar interbody fusion: single level transforaminal lumbar interbody fusion with adjacent segment unilateral laminotomy for bilateral decompression for spondylolisthesis with bisegmental stenosis
Introduction
Degenerative lumbar spondylolisthesis is often associated with lumbar multilevel spinal stenosis (MSS) of the adjacent segments.
Traditionally, this condition is treated with open decompression followed by a multilevel fusion (1,2). However, it has been hypothesized that a single level fusion of the unstable segment followed by a stand-alone decompression (i.e., laminectomy) without fusion of the adjacent segment may be a successful and less invasive treatment option (3).
Over the past two decades, minimally invasive surgery (MIS) has gained popularity due to several advantages (e.g., less muscle trauma, decreased blood loss and reduced hospitalization times). Pioneered by Foley and Smith in 1997, tubular discectomy has become a well-established procedure (4-6). Subsequently, this approach has been adapted to different procedures in spinal surgery, including decompression of the spinal canal (6). More recently, due to constantly evolving technologies, fusion procedures are also carried out in a minimally invasive fashion, such as the 3D navigated lumbar transforaminal lumbar interbody fusion (TLIF) (7).
Multilevel fusion is known to have a negative impact on the adjacent spinal segments by increasing the biomechanical stress thus leading to degeneration of the adjacent segments (8-10). On the other hand, a decompression without fusion when performed adjacent to a fused level may be associated with instability and failure (11-13). In order to assess the biomechanical stability of a simultaneously performed single level MIS-TLIF and decompression without fusion of the adjacent stenotic segment, our group recently performed a biomechanical cadaver study (14). The findings of this particular study suggest that, if done in a minimally invasive fashion, a unilateral laminotomy for bilateral decompression (ULBD) of the adjacent segment causes significantly less motion than a traditional open laminectomy. Our biomechanical study revealed that if decompressing a segment adjacent to a simultaneously performed fusion, it is crucial to preserve both facet joints in order to maintain stability. The findings of this study suggested that a mono-segmental MIS-TLIF combined with an adjacent MIS-tubular decompression is superior to a mono-segmental MIS-TLIF with adjacent level open laminectomy (14).
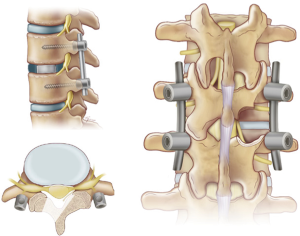
More recently, we translated this approach into clinical practice. The present article provides a technical description about how to perform a 3D navigated MIS-TLIF combined with a tubular ULBD of the adjacent segment (Figure 1).
Surgical technique
The procedure is performed under general anesthesia with the patient in prone position. As previously described by our group, intraoperative navigation is utilized with the iliac crest reference array placed opposite of the side from which the TLIF will be approached (7). An intraoperative CT is obtained prior to skin incision. The “one and a half” technique can be broken up into its components, as will be described below. The following technical description for MIS-TLIF plus ULBD of the adjacent segment explains the technique using 3D-CT-navigation. However, the same technique can be easily applied using intraoperative fluoroscopy instead of a 3D navigation system.
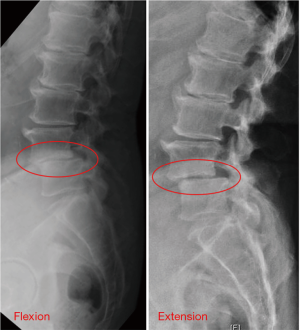
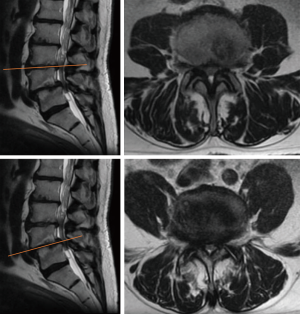
For better visualization, this technical note is accompanied by pre- and intraoperative images of a case of degenerative spondylolisthesis at L4/5 and adjacent stenosis of the spinal canal at L3/4 (Figures 2-5).
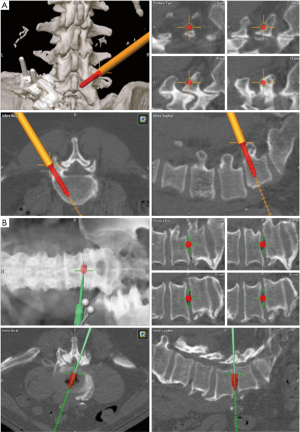

Pedicle screw placement
Using the navigation probe, the skin incisions for the pedicle screw insertion are marked on the patient’s skin bilaterally. On the side opposite the TLIF approach, a linear incision is made connecting the marked starting points for the pedicle screws. Soft tissue dissection is performed until the fascia is identified. The navigation probe is then used to reidentify the pedicle screw trajectories and a linear incision is made in the fascia in line with the pedicle screw trajectories. The navigation probe is then passed through the musculature to palpate the transverse processes to ensure accuracy (Figure 4), after which the pedicle screws can be safely placed. On the side the TLIF is to be performed, a linear skin incision is made approximately 1cm medial to the marked entry points for the pedicle screws. This medialization of the skin incision allows one to make a lateral fascial incision for the pedicle screws and a medial fascial incision for the TLIF through one skin incision. The pedicle screws are then placed in the same manner as described above.
TLIF
Through the same incision used to place the pedicle screws, the navigation probe is used to identify the ideal trajectory for the TLIF approach at the level of the fascia. The ideal docking point is over the inferior edge of the cephalad lamina and facet joint with a medial angle to allow midline cage insertion. Once this trajectory has been identified, a 2.5 cm linear incision is made in the fascia; this incision should be separate and medial to the previously created fascial incisions for the pedicle screws. The first dilator is then passed through the lumbar musculature to dock on lateral lamina and facet joint. Serial dilation is then performed and a 21 mm tubular retractor is placed and secured with the rigid table arm. The navigation probe is then used to confirm adequate tubular retractor placement. At this point, the operative microscope is brought in and the bony anatomy is exposed using extended monopolar and bipolar electrocautery. The inferior edge of the lamina and lateral pars of the cephalad level should be exposed, as well as the facet joint. The inferior articulating process (IAP) is then disconnected using a drill, Kerrison rongeurs, and/or an osteotome to expose the superior articulating process (SAP). Bone from the facetectomy is morselized and used later as autograft. A laminotomy is performed as needed to visualize the thecal sac and to allow for medialization of the dura. The SAP is then drilled away until flush with the superior edge of the caudal pedicle. At this point, the disc space should be visible. The navigated probe is used to confirm the location of the disc space and trajectory for later cage insertion. An annulotomy is performed and the disc is removed using shavers and curettes. The endplates are prepared thoroughly to facilitate bony fusion. It is critical to adequately prepare the endplates as MIS TLIF relies primarily on the interbody for fusion. The morselized autograft is packed into the disc space. A navigated TLIF cage filled with biologic is then inserted into the disc space (Figure 4).
Laminectomy
The navigation probe is used to identify the target level and trajectory for the ULBD opposite the side from which the TLIF was performed. The ideal target is the medial lamina and base of the spinous process overlying the target disc space at the site of spinal stenosis to be treated. Once the ideal trajectory has been identified, a 2.5 cm linear skin incision is made; this incision should be cephalad and medial to the previously created pedicle screw incision. The remaining steps have been previously described in a 10-step technique (6).
Rod insertion and closure
Once the pedicle screws and interbody cage are in place and the laminectomy has been completed, an intraoperative CT is obtained to confirm adequate hardware placement (Figure 5). Rods are inserted through the pedicle screw towers and locked in place. The tubular retractors are removed slowly and any soft tissue bleeding is addressed using coagulation and hemostatic agents. The fascia and skin are closed in standard fashion.
Discussion
The surgical management of mono-segmental instability with adjacent level spinal stenosis remains a controversial topic. Although minimally invasive techniques have grown increasingly popular in spinal surgery in the past two decades, many surgeons still recommend total laminectomy and fusion in those particular cases (12,13,15). Lone-standing open laminectomy seems to increase the risk of postoperative instability due to violation of the interspinous ligament complex which provides additional stability by limiting flexion and axial rotation (16). Therefore, resection of the spinous processes and the attached ligamentous complex may accelerate the segmental instability.
Our previously published data demonstrated that even in patients with mild preoperative spondylolisthesis and stenosis an MIS-decompression does not lead to an increase in instability necessitating secondary fusion (17). Since a segment adjacent to a spinal fusion has to endure additional biomechanical stress (18-22) it is more susceptible to instability after decompression. When performing a laminectomy, a previously published biomechanical cadaveric study demonstrated that, as expected, the least biomechanical instability occurs if both facet joints remain untouched (14); however, even with MIS laminectomy a portion of the ipsilateral medial facet joint is commonly resected (6). This goes along with the findings of Hamasaki et al. who demonstrated that bilateral medial facetectomy significantly decreases the segmental stiffness thus promoting instability (23). Thus, when performing the MIS laminectomy at the level not to be fused, one must take care to minimize the necessary violation of the ipsilateral medial facet joint.
Performing the decompression approach contralateral to the TLIF approach balances the tissue trauma (24). Mayer et al. described this as the so called “slalom technique” for multilevel lumbar decompression. The alternation of the approach side leads to more balanced muscle trauma than the conventional unilateral approach combined with the tissue preserving properties of a minimally invasive approach.
Limitations
As described above, this technique is limited to certain spinal pathologies. It is not recommended to perform this technique in cases of bisegmental instability. Therefore, it is critical to assess the patient’s stability with flexion/extension X-ray in the segment meant to undergo ULBD only with our described technique. Furthermore, this approach has the same limitations as the conventional MIS-TLIF. These limitations involve high grade spondylolisthesis, epidural scarring or severe osteoporosis (25).
Conclusions
This technical note provides a description of a motion preserving, minimally invasive technique to treat mono-segmental instability with adjacent segment spinal stenosis. Of note, this does not apply to situations where we treat adjacent segment instability and stenosis after a previously performed fusion. In this case, we prefer a decompression and fusion of the adjacent segment. The presently described “one and a half” technique is meant to stabilize the unstable segment while decompressing and maintaining the motion of the adjacent segment without causing significant instability. However, when performing the adjacent segment decompression, great care should be taken to minimize the violation of both facet joints in order to preserve the most stability. More long-term data is needed to prove the superiority of this approach over a two- or multi-level fusion.
Acknowledgements
None.
Footnote
Conflicts of Interest: R Härtl is a consultant for DePuy-Synthes, Ulrich and Brainlab and receives royalties from Zimmer. The other authors have no conflicts of interest to declare.
References
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 2007;356:2257-70. [Crossref] [PubMed]
- Herkowitz HN, Kurz L. Degenerative lumbar spondylolisthesis with spinal stenosis. J Bone Joint Surg Am 1991;73:802-8. [Crossref] [PubMed]
- Smorgick Y, Park DK, Baker KC, et al. Single versus multilevel fusion, for single level degenerative spondylolisthesis and multilevel lumbar stenosis. Four-year results of the spine patient outcomes research trial. Spine 2013;38:797. [Crossref] [PubMed]
- Oppenheimer JH, DeCastro I, McDonnell DE. Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurg Focus 2009;27:E9. [Crossref] [PubMed]
- Foley KT, Smith MM, Rampersaud YR. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 1999;7:e5. [Crossref] [PubMed]
- Boukebir MA, Berlin CD, Navarro-Ramirez R, et al. Ten-step minimally invasive spine lumbar decompression and dural repair through tubular retractors. Operative Neurosurgery 2017;13:232-45. [PubMed]
- Lian X, Navarro-Ramirez R, Berlin C, et al. Total 3D Airo® Navigation for Minimally Invasive Transforaminal Lumbar Interbody Fusion. Biomed Res Int 2016;2016:5027340. [Crossref] [PubMed]
- Strube P, Tohtz S, Hoff E, et al. Dynamic stabilization adjacent to single-level fusion: part I. Biomechanical effects on lumbar spinal motion. Eur Spine J 2010;19:2171-80. [Crossref] [PubMed]
- Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 2002;27:2431-4. [Crossref] [PubMed]
- Aiki H, Ohwada O, Kobayashi H, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci 2005;10:490-5. [Crossref] [PubMed]
- Cardoso MJ, Dmitriev AE, Helgeson M, et al. Does superior-segment facet violation or laminectomy destabilize the adjacent level in lumbar transpedicular fixation?: an in vitro human cadaveric assessment. Spine 2008;33:2868-73. [Crossref] [PubMed]
- Postacchini F, Cinotti G. Bone regrowth after surgical decompression for lumbar spinal stenosis. J Bone Joint Surg Br 1992;74:862-9. [Crossref] [PubMed]
- Hopp E, Tsou PM. Postdecompression lumbar instability. Clin Orthop Relat Res 1988.143-51. [PubMed]
- Grunert P, Reyes PM, Newcomb AG, et al. Biomechanical Evaluation of Lumbar Decompression Adjacent to Instrumented Segments. Neurosurgery 2016;79:895-904. [Crossref] [PubMed]
- Guigui P, Barre E, Benoist M, et al. Radiologic and computed tomography image evaluation of bone regrowth after wide surgical decompression for lumbar stenosis. Spine 1999;24:281-8. [Crossref] [PubMed]
- Sharma M, Langrana NA, Rodriguez J. Role of ligaments and facets in lumbar spinal stability. Spine 1995;20:887-900. [Crossref] [PubMed]
- Alimi M, Hofstetter CP, Pyo SY, et al. Minimally invasive laminectomy for lumbar spinal stenosis in patients with and without preoperative spondylolisthesis: clinical outcome and reoperation rates. J Neurosurg Spine 2015;22:339-52. [Crossref] [PubMed]
- Hsu KY, Zucherman J, White A. The long-term effect of lumbar spine fusion: deterioration of adjacent motion segments. Lumbar fusion and stabilization. Springer, 1993:54-64.
- Chow DH, Luk KD, Evans JH, et al. Effects of short anterior lumbar interbody fusion on biomechanics of neighboring unfused segments. Spine 1996;21:549-55. [Crossref] [PubMed]
- Nagata H, Schendel MJ, Transfeldt EE, et al. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine 1993;18:2471-9. [Crossref] [PubMed]
- Chen CS, Cheng CK, Liu CL, et al. Stress analysis of the disc adjacent to interbody fusion in lumbar spine. Med Eng Phys 2001;23:483-91. [Crossref] [PubMed]
- Ren C, Song Y, Liu L, et al. Adjacent segment degeneration and disease after lumbar fusion compared with motion-preserving procedures: a meta-analysis. Eur J Orthop Surg Traumatol 2014;24:S245-53. [Crossref] [PubMed]
- Hamasaki T, Tanaka N, Kim J, et al. Biomechanical assessment of minimally invasive decompression for lumbar spinal canal stenosis: a cadaver study. J Spinal Disord Tech 2009;22:486-91. [PubMed]
- Mayer HM, Heider F. "Slalom": Microsurgical Cross-Over Decompression for Multilevel Degenerative Lumbar Stenosis. Biomed Res Int 2016;2016:9074257. [Crossref] [PubMed]
- Pimenta L, Tohmeh A, Jones D, et al. Rational decision making in a wide scenario of different minimally invasive lumbar interbody fusion approaches and devices. J Spine Surg 2018;4:142-55. [Crossref] [PubMed]


