Decreasing radiation dose with FluoroLESS Standalone Anterior Cervical Fusion
Introduction
Orthopedic surgery has advanced with the use of instrumentation and implants. Radiation dose continues to be a concern especially in the field of spine surgery, where anterior and posterior instrumentation is frequently utilized to treat multiple pathologies. The advent of minimally invasive procedures has especially increased the use of intraoperative imaging, where instrumentation is inserted percutaneously without the direct anatomic visualization compared to open procedures.
Ionizing radiation has been classified as a carcinogen by the World Health Organization (1). Radiation types within the “ionizing radiation” range have enough energy to remove electrons from atoms (1). The use of fluoroscopic localization is performed routinely for surgical spine procedures with the advent of minimally invasive surgical techniques. There have been increasing concerns about overall radiation exposure to patients as well as physicians. Several studies have demonstrated a higher incidence of cancer in physicians and other healthcare workers whose work involves the use of fluoroscopic imaging. These implications are often neglected by the health care team for the benefit of treating patients (2-7). The use of protective equipment and measuring radiation dosage are means of trying to decrease total dosage over exposure time (8). Surgeons are likely to exceed their lifetime radiation dose limit in the initial 10 years of practice (9).
The incidence of chronic neck pain related to degenerative disc disease affects up to two-thirds of the population over their lifetime (10). The literature has demonstrated the treatment option of ACDF for cervical disc herniation and spondylosis (11-16). Standalone cervical fixation devices have shown good outcomes both in the hospital and outpatient setting with the potential to decrease fluoroscopic use and total exposure time to patients and surgeons (17). The authors aim to assess radiation dose in standalone cervical fusion versus anterior cervical plate (ACP) fusion. Thereby demonstrating the feasibility of decreasing radiation dosage in patients who had cervical spine surgery to achieve FluoroLESS ACDF.
Methods
This retrospective review of prospectively collected data of 97 patients was performed with standalone ACDF (S-ACDF) in 48 consecutive patients, Group 1 (A-CIFT Solofuse-P®, SpineFrontier Inc. Malden, MA, USA) in the outpatient setting with comparison control group of ACDF with an ACP in 49 patients, Group 2 (Arena-C®, SpineFrontier Inc. Malden, MA, USA) in the outpatient setting; fusion was reinforced with an ACP (Invue®, SpineFrontier Inc., Malden, MA, USA). We received IRB approval as part of a cohort of patients who had anterior cervical surgery. This was a single surgeon study in the outpatient setting and patients had informed consent prior to proceeding to surgery. Indications for surgery included: failed conservative management for at least six weeks. Patients with symptomatic cervical spondylosis, stenosing herniated discs, degenerative disc disease with instability and facet arthritis, tropism or facetogenic pain were also included. An exclusion criterion for outpatient surgery used at this institute (18). We recommended the discontinuation of narcotics at least two weeks before surgery if the patient had a history of narcotic use for greater than 6 months (19). All patients with chronic medical conditions were sent for clearance to their family practitioner and/or cardiologist where applicable.
Fluoroscopy was performed for positioning, identification of level, placement of the implant, each screw, final AP and lateral images for the first 20 patients in Group 1. We noted after this that screw placement would be intact with the stop allowing good placement of the implant.
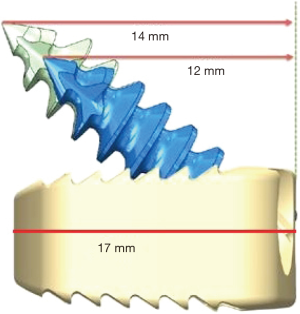
The implant design with a length of 17 mm, the width of 13 mm and angle of 40o (Figure 1) allowed for the approximation of screw length to be placed safely based on average cervical vertebral height (20). This is confirmed by cosine rule of cosine (Ѳ) = adj/hyp allowing us to confidently place screw without fluoroscopy confirmation for each screw.
Surgical technique
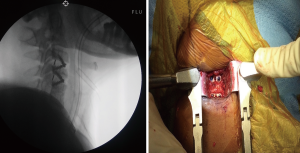
On the day of the procedure, informed consent was signed and operative procedure verified. Patient was placed under general anesthesia, and sterile preparation performed. A midline transverse incision base on modification of the standard Smith-Robinson operative technique then made (21,22). Surgical dissection, exposure, and discectomy performed at the desired operative level have been previously detailed in a study by Chin et al for cervical fusion (22). Confirmation of level is performed fluoroscopically with an 18G bent spinal needle as well as with retractors and Casper pin in place. Pituitary ronguers, curette and burr drill used to perform discectomy removing the affected disc and opening foraminal space, the posterior longitudinal ligament was retained in situ (23,24). The PEEK caged was prepacked with demineralized bone matrix (DBM0 pure to aid fusion. Placement of the standalone cervical PEEK cage performed with aid of a stop and two screws then placed under direct visualization. Hemostasis achieved using bipolar forceps, a Penrose drain was placed above the implant, brought through the incision and secured with a sterile safety pin. This allows for wound drainage to prevent the development of a postoperative hematoma in all patients. In Group 2 the surgical approach was similar with DBM prepacked within the PEEK cage and ACP placed for supplemental fixation. Hemostasis achieved using bipolar forceps, a Penrose drain was placed above the implant, brought through the incision and secured with a sterile safety pin. This allows for wound drainage to prevent the development of a postoperative hematoma in all patients. The closure was performed in layers and a Penrose drain was left in-situ. Confirmation of placement of implants by fluoroscopic was performed at the end of procedure for lateral and AP views (Figure 2).
Radiographic equipment
This study was performed using a Fluoroscopic X-ray system (Zen-7000) fluoroscopy machine. Total filtration of the X-ray beam was 3.7 mm Al. The machine was placed on auto exposure with the ability to manually change the pre-programmed exposure factors if needed. The machine also had the option to capture the last fluoroscopic image.
Discharge and follow up
Our institute used an outpatient protocol which was previously published with instructions discussed with all patients and caregivers (18,22,25). Potential complications were discussed with the patient prior to and after discharge and follow up based on published protocol (18,22).
Statistical analysis
SPSS v22 (IBM Corporation, New York, USA) used to perform analysis of continuous and categorical data. Respectively we used an independent sample student t-test and a chi-squared analysis. Significant data is determined if the P value <0.05.
Results
Forty-eight patients in Group 1 (S-ACDF), 71% were female with the group’s mean age being 47.8±1.6 years and a mean BMI 29.7±1.0 kg/m2. Of the 49 patients in Group 2 (ACDF-ACP), 87% were female with the group’s mean age being 48.7±1.4 years and a mean BMI 29.7±1.1 kg/m2. No statistical significance was demonstrated between demographics of groups. Preoperative and postoperative outcomes did not show any statistical significance (17).
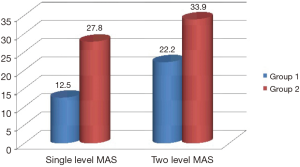
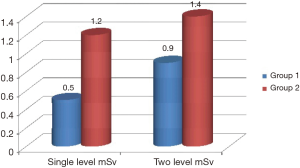
Radiation dose was obtained from fluoroscopy machine for each patient and calculated using the formula of mA X time = mAs and D = g × kV × mAs/d2 mean radiation dose in group 1 of 17.9±6.6 mAs and 0.8±0.3 mSv was significantly less compared to group 2 which was 29.8±5.4 and 1.3±0.2 mSv, P<0.001. The average radiation dose for single-level fusion in Group 1 was 12.5±3.5 mAs and 0.5±0.1 mSv this is compared to average radiation dose in Group 2 of 27.8±3.9 mAs and 1.2±0.2 mSv, P=0.001. The average radiation dose for two level fusion in Group 1 was 22.2±5.1 mAs and 0.9±0.2 mSv this is compared to average radiation dose in Group 2 of 33.9±6.0 and 1.4±0.3 mSv, P=0.001. Figures 3 and 4 illustrate the MAS and radiation dose, respectively.
Discussion
The authors aimed to assess the effective radiation dose for patients who received stand-alone anterior cervical fusion in the outpatient setting. Our study showed a statistically significant decrease in the total radiation dose to the patient. Outcome scores were also comparable demonstrating the feasibility of performing outpatient S-ACDF. We did not access total radiation dose to a physician but can inference there would be a decrease when doing standalone fusions compared to fusion with anterior plates.
Radiation exposure is of concern over the lifetime of patients and surgeons. It is pertinent for healthcare personnel to reduce this exposure in the way procedures are ordered and performed especially in the specialty of spine surgery. Pedicle screw insertion is of major concern and has been the focus of reduction due to the radiation does to both patients and medical staff (26-32).
In a randomized control study by Nayar et al. (31), they demonstrated that with the use of ultra-low radiation imaging (ULRI) there was no compromise of the accuracy of placement of pedicle screws with a reduction in radiation dose to patients and surgeons.
Studies have also demonstrated that the use of computer navigation decreases overall radiation dose. In a small prospective randomized study by Villard et al. demonstrated that radiation dose for the patient was higher with the freehand technique, 1,884.8 cGy·cm (non-navigated) versus 887 cGy·cm (navigated), without reaching a statistically significant level (26). A more recent study, however, suggested that no benefits using the computer-guided system (28). The fact remains that accuracy of screw placement and decreasing radiation dose are the most important determinants during pedicle screw placement.
In reviewing the literature there were limited studies looking specifically at radiation exposure during anterior cervical discectomy and fusion (ACDF) as this procedure already has a low radiation dose exposure per procedure (33-35). This shows that more study is required has the cumulative dose can still have been dramatic effects have there are increasing trends in ACDF being performed in the outpatient settings (36). In a study by Metaxas, they demonstrated a low cumulative dose range of 0.96 mGy (range, 0.04−6.58 mGy) and ED between 0.001 and 0.097 mSv (average 0.015 mSv) (33). This study, however, has some limitations with the use of Caldose software which has no modality to estimate dose to the cervical spine. The results of our study when compared would be the total radiation dose from fluoroscopy machine compared to a calculated absorbed dose.
The authors of this manuscript recognize the limitations of this study. The patients recruited for this study were mostly female and both groups had an average BMI of about 30. Performing a similar study with a completely randomized and large population size would provide greater evidence to support the results of this study and how applicable they are too different patient populations. There may have also been limitations in the way that the radiation dosage was calculated for each group since the amount of radiation produced per X-ray radiograph may have a slight variation. Since the radiation dosage was calculated the same for each group, the results were likely not affected by this limitation, however using a more accurate method of measuring radiation via fluoroscopy may provide a better idea of the difference in magnitude of radiation produced by each of the surgical procedures discussed in this study. Lastly, the clinical relevance of the findings mentioned in this study can be better understood if a longitudinal study was performed over decades with a large sample size to identify if there was a difference in the number of malignancies reported between patients that received either surgical procedure. Although the results mentioned in this study may provide a potential benefit for both surgeons and patients, further studies should be performed to verify these findings and their clinical impacts.
Conclusions
In the outpatient setting, S-ACDF has shown a statistically significant intergroup difference in overall radiation dose, as well as single and two-level fusions (P<0.001). We conclude that S-ACDF can decrease overall radiation exposure to patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: KR Chin is a shareholder in and receives other benefits from SpineFrontier Inc. The other authors have no conflicts of interest to declare.
Ethical Statement: IRB approval was granted for patients involved in study as part of a cohort of patients who had anterior cervical surgery. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Hardell L. World Health Organization, radiofrequency radiation and health - a hard nut to crack Int J Oncol 2017;51:405-13. (Review). [Crossref] [PubMed]
- Yoshinaga S, Mabuchi K, Sigurdson AJ, et al. Cancer risks among radiologists and radiologic technologists: review of epidemiologic studies. Radiology 2004;233:313-21. [Crossref] [PubMed]
- Mastrangelo G, Fedeli U, Fadda E, et al. Increased cancer risk among surgeons in an orthopaedic hospital. Occupational medicine (Oxford, England) 2005;55:498-500. [Crossref] [PubMed]
- Venneri L, Rossi F, Botto N, et al. Cancer risk from professional exposure in staff working in cardiac catheterization laboratory: insights from the National Research Council's Biological Effects of Ionizing Radiation VII Report. Am Heart J 2009;157:118-24. [Crossref] [PubMed]
- Hoffman DA, Lonstein JE, Morin MM, et al. Breast cancer in women with scoliosis exposed to multiple diagnostic x rays. J Natl Cancer Inst 1989;81:1307-12. [Crossref] [PubMed]
- Chou LB, Chandran S, Harris AH, et al. Increased breast cancer prevalence among female orthopedic surgeons. J Womens Health (Larchmt) 2012;21:683-9. [Crossref] [PubMed]
- Mroz TE, Abdullah KG, Steinmetz MP, et al. Radiation exposure to the surgeon during percutaneous pedicle screw placement. J Spinal Disord Tech 2011;24:264-7. [Crossref] [PubMed]
- Mechlenburg I, Daugaard H, Soballe K. Radiation exposure to the orthopaedic surgeon during periacetabular osteotomy. Int Orthop 2009;33:1747-51. [Crossref] [PubMed]
- Ul Haque M, Shufflebarger HL, O'Brien M, et al. Radiation exposure during pedicle screw placement in adolescent idiopathic scoliosis: is fluoroscopy safe? Spine (Phila Pa 1976) 2006;31:2516-20. [PubMed]
- Todd AG. Cervical spine: degenerative conditions. Curr Rev Musculoskelet Med 2011;4:168-74. [Crossref] [PubMed]
- Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607-24. [Crossref] [PubMed]
- Ipsen BJ, Kim DH, Jenis LG, et al. Effect of plate position on clinical outcome after anterior cervical spine surgery. Spine J 2007;7:637-42. [Crossref] [PubMed]
- Scherping SC Jr. Anterior cervical discectomy and fusion: role of anterior plate fixation in degenerative cervical disorders. Semin Spine Surg 2004;16:35-41. [Crossref]
- Goldberg G, Hilibrand A. Anterior cervical discectomy and fusion. Oper Tech Orthop 2003;13:188-94. [Crossref]
- Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 1953;10:154-68. [Crossref] [PubMed]
- Bailey RW, Badgley CE. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am 1960;42-A:565-94. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Mustafa LM, et al. Sentinel sign in standalone anterior cervical fusion: Outcomes and fusion rate. J Orthop 2018;15:935-9. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Eligibility of Outpatient Spine Surgery Candidates in a Single Private Practice. Clin Spine Surg 2017;30:E1352-E8. [Crossref] [PubMed]
- Lawrence JT, London N, Bohlman HH, et al. Preoperative narcotic use as a predictor of clinical outcome: results following anterior cervical arthrodesis. Spine (Phila Pa 1976) 2008;33:2074-8. [Crossref] [PubMed]
- Gilad I, Nissan M. Sagittal evaluation of elemental geometrical dimensions of human vertebrae. J Anat 1985;143:115-20. [PubMed]
- Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull John Hopkins Hosp 1955;96:223-4.
- Chin KR, Pencle FJR, Seale JA, et al. Clinical Outcomes of Outpatient Cervical Total Disc Replacement Compared With Outpatient Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:E567-E74. [Crossref] [PubMed]
- Chin KR, Ghiselli G, Cumming V, et al. Postoperative magnetic resonance imaging assessment for potential compressive effects of retained posterior longitudinal ligament after anterior cervical fusions: a cross-sectional study. Spine (Phila Pa 1976) 2013;38:253-6. [Crossref] [PubMed]
- Avila MJ, Skoch J, Sattarov K, et al. Posterior longitudinal ligament resection or preservation in anterior cervical decompression surgery. J Clin Neurosci 2015;22:1088-90. [Crossref] [PubMed]
- Marshall SI, Chung F. Discharge criteria and complications after ambulatory surgery. Anesth Analg 1999;88:508-17. [Crossref] [PubMed]
- Villard J, Ryang YM, Demetriades AK, et al. Radiation exposure to the surgeon and the patient during posterior lumbar spinal instrumentation: a prospective randomized comparison of navigated versus non-navigated freehand techniques. Spine (Phila Pa 1976) 2014;39:1004-9. [Crossref] [PubMed]
- Dabaghi Richerand A, Christodoulou E, Li Y, et al. Comparison of Effective Dose of Radiation During Pedicle Screw Placement Using Intraoperative Computed Tomography Navigation Versus Fluoroscopy in Children With Spinal Deformities. J Pediatr Orthop 2016;36:530-3. [Crossref] [PubMed]
- Urbanski W, Jurasz W, Wolanczyk M, et al. Increased Radiation but No Benefits in Pedicle Screw Accuracy With Navigation versus a Freehand Technique in Scoliosis Surgery. Clin Orthop Relat Res 2018;476:1020-7. [Crossref] [PubMed]
- Fan Y, Peng Du J, Liu JJ, et al. Radiological and clinical differences among three assisted technologies in pedicle screw fixation of adult degenerative scoliosis. Sci Rep 2018;8:890. [Crossref] [PubMed]
- Fomekong E, Pierrard J, Raftopoulos C. Comparative Cohort Study of Percutaneous Pedicle Screw Implantation without Versus with Navigation in Patients Undergoing Surgery for Degenerative Lumbar Disc Disease. World Neurosurg 2018;111:e410-e417. [Crossref] [PubMed]
- Nayar G, Blizzard DJ, Wang TY, et al. Pedicle screw placement accuracy using ultra-low radiation imaging with image enhancement versus conventional fluoroscopy in minimally invasive transforaminal lumbar interbody fusion: an internally randomized controlled trial. J Neurosurg Spine 2018;28:186-93. [Crossref] [PubMed]
- Kraus M, von dem Berge S, Perl M, et al. Accuracy of screw placement and radiation dose in navigated dorsal instrumentation of the cervical spine: a prospective cohort study. Int J Med Robot 2014;10:223-9. [Crossref] [PubMed]
- Metaxas VI, Messaris GA, Gatzounis GD, et al. Patient Dose in Fluoroscopically Guided Cervical Discectomy and Fusion. Radiat Prot Dosimetry 2017;174:575-82. [PubMed]
- Bohl DD, Hustedt JW, Blizzard DJ, et al. Routine imaging for anterior cervical decompression and fusion procedures: a survey study establishing current practice patterns. Orthopedics 2012;35:e1068-72. [Crossref] [PubMed]
- Mulconrey DS. Fluoroscopic Radiation Exposure in Spinal Surgery: In Vivo Evaluation for Operating Room Personnel. Clin Spine Surg 2016;29:E331-5. [Crossref] [PubMed]
- Pencle FJR, Rosas S, Britton NT, et al. Trends in Inpatient versus Outpatient Anterior Cervical Discectomy and Fusion in the United States of America: An Epidemiologic and Economic Analysis. West Indian Med J 2017.66.