Patient and radiographer assessment of slump sitting flexion compared to conventional standing forward bending flexion
Introduction
Segmental instability of the spine in the sagittal plane is a poorly-defined entity, due to the lack of standardisation in performing lumbar flexion and extension X-rays (1-4), and the absence of consensus diagnostic criteria (5-9). Many surgeons thus plan their surgery based on what they perceive to be segmental instability (10-13), when deciding between neural decompression alone and decompression with fusion.
The authors of this paper believe that current widely-practised methods of performing flexion-extension X-rays are suboptimal and may lead to an under-diagnosis of this condition. Patients who are unable to stand, have difficulties balancing themselves in forward flexion, who have tight hamstrings or lower limb abnormalities may be particularly at risk. In a previous study comparing slump-sitting and conventional standing forward bending methods, the former proved to be much better in stressing the lumbar spine both globally and in each individual lumbar vertebral segment (1,14). It increases the diagnosis rate of sagittal spinal instability up to 40% depending on the diagnostic criteria used (1). The increased sensitivity of this method in detecting lumbar spine instability hence serves as a good starting point for future studies aimed at establishing diagnostic criteria for segmental instability to achieve a more universal definition. This would subsequently allow us to further stratify patients according to the degree of instability and identify those who would truly benefit from fusion surgery.
In addition to its diagnostic utility, several other factors need to be considered before a radiography posture can be accepted as the ‘gold standard’. It should also be safe (15), precise (16), easily reproducible (17) for the radiographers as well as comfortably achievable by the patient (15). This study aims to explore the qualitative aspects the slump sitting method of obtaining flexion-extension radiographs compared to the conventional standing forward bending method from both the radiographer and the patient perspective. We hypothesised that in addition to being diagnostically superior, the slump sitting method would be favoured by both radiographers and patients.
Methods
This study was performed concurrently with our previous study comparing the diagnostic ability of both methods—the recruitment criteria and study methodology have been previously described (1). In that study, 60 consecutive patients were recruited and randomly assigned into two groups. The first group were those who had flexion X-rays taken using the new (slump sitting) method first, followed by the conventional (standing forward bend) method; while the second group were those who had X-rays taken using the conventional method first, followed by the new method. Flexion angles were compared between both groups for the entire lumbar spine and for each segmental levels. Vertebral translation were also compared for each segmental levels.
In this study, we distributed questionnaires to all the same patients undergoing both methods of flexion-extension X-rays, as well as the radiographers obtaining them. The National Domain-Specific Ethics Committee approval was obtained prior to study commencement, and written informed consent was taken for all subjects. There was no funding required for this study, and there were no potential conflicts of interests.
A pilot of 10 patients was used to develop the questionnaire tool prior to the commencement of the study. Aspects of positioning assessed by the questionnaire include the safety, reliability and technical challenges for the radiographers, as well as comfort for the patients. Qualitative feedback was also obtained using the questionnaires.
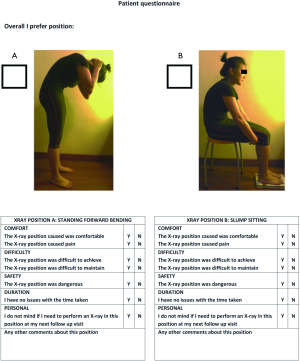
In the patient questionnaire, pictorial representations of the postures were included in the questionnaire leaflets for ease of reference. Dichotomous questions were used to assess each posture separately, and then patients were asked to pick their favoured posture. A copy of this questionnaire is shown in Figure S1.
For the radiographer questionnaire, responses were obtained in the form of a Likert-type scale from 1 to 5. Additional information including the number of attempts required to obtain satisfactory radiographs and the amount of time taken to complete the study were also collected as a proxy measure of reliability and convenience. A copy of this questionnaire is shown in Figure S2.
All questionnaires were self-administered. Radiographer questionnaires were in English and patient questionnaires were in both English and Mandarin. Ten patients spoke only Chinese dialects and two patients spoke only Malay, requiring translations by a clinic assistant. All questionnaires were distributed after obtaining all required X-rays. Both the patients’ and the radiographers’ questionnaires were collected by a study administrator for storage until the end of the study when the data was collated. A total of eight radiographers provided feedback for all 60 patients involved in the study.
Of the 60 patients who participated in the study, only 52 returned completed questionnaires initially. Eight who did not complete the questionnaires due to logistical errors were revisited and completed via telephone interview. Data from all questionnaires were included in the final analysis.
Statistical analysis
All collected data was tabulated using Microsoft Excel 2013 (version 15.0) and analysed using International Business Machines (IBM) Statistical Package for the Social Sciences (SPSS version 23.0).
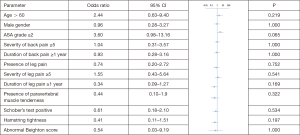
Baseline characteristics of subjects in both groups were compared using Chi-squared tests for binomial data and unpaired t-tests for continuous parametric data to identify any significant differences that may have occurred due to chance during block randomization step (Table 1). Parameters evaluated include the patients’ age, gender, American Society for Anaesthesiologist (ASA) grade, presence and severity of back or leg pain, duration of each pain, presence of paravertebral muscle tenderness, Schober’s test, hamstring tightness and Beighton’s ligament laxity score. These parameters were analysed as they can affect the patients’ choice of X-ray method.
Full table
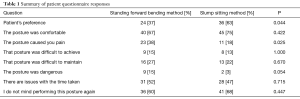
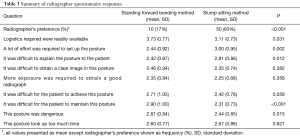
The questionnaire answers provided by the patients were tabulated as paired binary data. Using the null hypothesis that there are no significant differences between the two methods, the paired binary data for each question was evaluated using a McNemar test (Table 2). Next, the questionnaire answers provided by the radiographers were tabulated as ordinal values from a scale of 1 to 5. These were evaluated using the Sign test for ordinal values with repeated measures (Table 3).
Full table
Full table
Lastly, the odds ratio of each baseline characteristic for preferring the slump sitting method compared to the standing forward bending method was determined (Figure 1) in an attempt to identify patients who preferred one posture over the other. Multivariate linear regression modelling was then performed using preference for the slump sitting method as a positive outcome.
Results
Of the 60 patients who participated in the study, 28 were male and 32 female. The mean age was 56.5 years (range, 44–79 years). There were no significant differences in baseline characteristics between the two groups, regardless which method of imaging was performed first. Details of patient characteristics and lumbar spine alignment parameters can be found in the previous study (1).
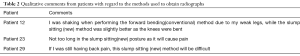
For this study, the results from the patient questionnaire is summarised in Table 1. Twenty-four preferred the conventional method while 36 preferred the new method (P=0.044). There were no significant differences between both methods in terms of subject’s comfort, difficulty in achieving and maintaining postures during X-rays, time taken, and preference for future radiographs from the patients’ perspective. The standing forward bending method however, was shown to more frequently cause pain than the slump sitting method (P=0.025). There was also a trend towards significance in patients finding the conventional method more dangerous than the new method (P=0.054). All comments obtained from the free text box of the questionnaire is presented in Table 2.
With regard to the radiographers responses (Table 3), 10 preferred the conventional method while 50 preferred the new method (P<0.001). There were no significant differences between both methods in terms of difficulty in obtaining clear images, amount of exposure required, and duration. The conventional method was logistically easier to perform. On average, the new slump sitting method required more effort and was more difficult to explain to patient. The new method however was felt by radiographers to be significantly less difficult to maintain and less dangerous.
There were no identifiable factors which predicted patient preference towards either posture (Figure 1). Patients with an ASA grade ≥2 had an odds ratio of 3.60 to prefer the new slump sitting method as a desired outcome—this however did not reach statistical significance. There was also no significant correlation between the radiographers’ experience and the duration required to obtain X-rays or the number of X-rays taken (data not shown).
Discussion
The slump sitting posture flexes the lumbar spine more than the conventional standing forward bending posture (1,14). This stresses the lumbar spine into more flexion and aids in the diagnosis of sagittal lumbar instability, which as mentioned previously may affect surgical decision making; fusion may be indicated as a result in patients for whom isolated decompression have been previously preferred (10-12). In order for this new flexion method to be more widely implemented, the improved diagnostic yield should not come at the expense of patient safety and comfort, nor unnecessarily burden the duty radiographers (15-17).
Our study showed that the radiographers felt that the slump sitting posture is safer compared to the standing forward bending posture (P=0.015). Overall more patients felt that the standing forward bending posture was dangerous compared to the slump sitting posture, although this difference did not reach statistical significance (P=0.054). The slump sitting posture could theoretically reduce the risk of falls and related injuries (18). Patients sitting on the chair have a lower centre of gravity and don’t have to support their own weight; this would be especially useful in patients with leg weakness or those unsteady on their feet. Furthermore, the enhanced safety of this posture allows patients to push themselves into maximum possible flexion without worry—the radiographs obtained are thus more likely to reflect a true stress view of the spine (19). Similarly, significantly fewer patients reported pain during slump sitting compared to standing forward bending (P=0.025), which makes the patients less apprehensive when flexing. This appears to occur in spite of the increased stress created applied across the lumbar spine. While respecting selected spinal conditions may predispose to patients experiencing back pain during flexion or extension, this was not the main aim of the study and was hence not evaluated. Multivariate analysis showed there was a tendency for patients with ASA ≥2 to prefer the slump sitting posture, although again this did not reach statistical significance. This may be secondary to the greater comfort appreciated by patients with multiple co-morbidities when doing the slump sitting method (19,20).
From the radiographers point of view, the slump sitting method was perceived to be more easily achieved (P=0.058) and maintained (P<0.001). Patients themselves did not report any more difficulty holding their spines flexed in the slump sitting posture compared to the forward bending posture. With respect to the time taken to obtain the radiographs, there was no real or perceived difference between both methods from both the radiographers and patients’ perspective. This is important as the imaging process is potentially time consuming and may interfere with the efficiency of the clinical workflow (21,22). From a technical viewpoint, both methods were also equivalent in terms of the perceived ease of obtaining images and the amount of radiation exposure required.
The slump sitting method is not without its limitations. Many radiographers felt that the slump sitting method was more logistically demanding (P=0.031), more difficult to explain to the patient (P=0.012), and required more effort to perform (P=0.002). These technical challenges may be related to the relative novelty of the positioning method in our institution, and could potentially be overcome via procedure standardization and practice (17,23,24). As the process of explaining and performing flexion X-rays in the slump sitting posture becomes more streamlined with repetition we believe the perception of these challenges will diminish (17). The slump sitting method inherently requires more logistics—we do not however feel that the additional chair required for the slump sitting method is prohibitive. Even though our study employed both visual aids (25) and verbal instructions (24,25) from radiographers when instructing patients to assume these X-ray postures, providing patients with an information leaflet prior to the imaging process may also ease some of the technical challenges faced by the radiographers (25).
This study was performed in a tertiary hospital with a dedicated spine division, supported by a large team of radiographers who help obtain the radiographs for all the patients. Our radiographers varied in terms of experience and training, but a multi-variable analysis performed did not reveal any association between the number of X-ray attempts, the overall imaging time and years of experience of the radiographers (23). This reflects the fact that while imaging in the slump sitting posture may have been perceived to be challenging, it could be reliably and effectively performed regardless of radiographer’s experience and training (26).
The slump sitting posture has already been shown to improve our ability to diagnose lumbar instability based on current guidelines. This study shows that it at the very least equivalent and in some aspects superior to the conventional standing forward bending method based on patient and radiographer feedback. It is hence our recommendation that it should be adopted as the standardised method for performing lumbar flexion X-rays, and subsequently be used to develop diagnostic criteria for spinal instability.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The National Domain-Specific Ethics Committee approval was obtained prior to study commencement, and written informed consent was taken for all subjects.
References
- Hey HW, Lau ET, Lim JL, et al. Slump sitting X-ray of the lumbar spine is superior to the conventional flexion view in assessing lumbar spine instability. Spine J 2017;17:360-8. [Crossref] [PubMed]
- Bontrager KL, Lampignano J. Textbook of Radiographic Positioning and Related Anatomy-E-Book. Elsevier Health Sciences, 2013 Aug 7.
- Moore A, Alsop C. Clark's Positioning in Radiography 12Ed. Hodder Education, 2005.
- Frank E, Long B, Smith B. Merrill’s atlas of radiographic positioning and procedures: Volume 3. Mosby, 2007.
- Dupuis PR, Yong-Hing K, Cassidy JD, et al. Radiologic diagnosis of degenerative lumbar spinal instability. Spine (Phila Pa 1976) 1985;10:262-76. [Crossref] [PubMed]
- Pope MH, Panjabi M. Biomechanical definitions of spinal instability. Spine (Phila Pa 1976) 1985;10:255-6. [Crossref] [PubMed]
- White AA, Panjabi MM. Clinical biomechanics of the spine. Philadelphia: Lippincott, 1990.
- Hammouri QM, Haims AH, Simpson AK, et al. The utility of dynamic flexion-extension radiographs in the initial evaluation of the degenerative lumbar spine. Spine (Phila Pa 1976) 2007;32:2361-4. [Crossref] [PubMed]
- Dvorak J, Panjabi MM, Novotny JE, et al. Clinical validation of functional flexion-extension roentgenograms of the lumbar spine. Spine (Phila Pa 1976) 1991;16:943-50. [Crossref] [PubMed]
- Frymoyer JW, Selby DK. Segmental instability. Rationale for treatment. Spine (Phila Pa 1976) 1985;10:280-6. [Crossref] [PubMed]
- Pearson AM, Lurie JD, Blood EA, et al. Spine patient outcomes research trial: radiographic predictors of clinical outcomes after operative or nonoperative treatment of degenerative spondylolisthesis. Spine (Phila Pa 1976) 2008;33:2759-66. [Crossref] [PubMed]
- Sengupta DK, Herkowitz HN. Degenerative spondylolisthesis: review of current trends and controversies. Spine (Phila Pa 1976) 2005;30:S71-81. [Crossref] [PubMed]
- American Academy of Orthopaedic Surgeons. Spinal Fusion Surgery [Internet]. American Academy of Orthopaedic Surgeons [cited 2015 July 18]. Available online: http://www.aaos.org/govern/federal/issues/HumanaSpinalFusionSurgery.pdf
- Hey HW, Choong DA, Lau ETC, et al. Slump sitting X-ray of the lumbar spine is better than conventional flexion view. Poster presented at: The Combined Congress of 12th Hong Kong International Orthopaedic Forum (HKIOF), The 10th Combined Congress of the Asia Pacific Spine Society (APSS), and The Asia Pacific Pediatric Orthopaedic Society (APPOS); 2015 Jun 5-7; Hong Kong, China.
- Falls in Radiology. Establishing a Unit-Specific Prevention Program. Pa Patient Saf Advis 2011;8:12-7.
- Frobin W, Brinckmann P, Leivseth G, et al. Precision measurement of segmental motion from flexion—extension radiographs of the lumbar spine. Clin Biomech (Bristol, Avon) 1996;11:457-65. [Crossref] [PubMed]
- Maruyama T, Yamamoto H. Study of positioning techniques for skull radiography. Poster presented at: Instrumentation and measurement technology conference; 2006 Apr 24-27; Sorrento, Italy.
- Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting. J Gen Intern Med 2004;19:732-9. [Crossref] [PubMed]
- Geisser ME, Haig AJ, Wallbom AS, et al. Pain-related fear, lumbar flexion, and dynamic EMG among persons with chronic musculoskeletal low back pain. Clin J Pain 2004;20:61-9. [Crossref] [PubMed]
- O’Sullivan PB, Grahamslaw KM, Kendell M, et al. The effect of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine (Phila Pa 1976) 2002;27:1238-44. [Crossref] [PubMed]
- Reiner B, Siegel E, Carrino JA. Workflow optimization: current trends and future directions. J Digit Imaging 2002;15:141-52. [Crossref] [PubMed]
- Andriole KP. Productivity and cost assessment of computed radiography, digital radiography, and screen-film for outpatient chest examinations. J Digit Imaging 2002;15:161-9. [Crossref] [PubMed]
- Williams PL, Berry JE. What is competence? A new model for diagnostic radiographers: Part 1. Radiography 1999;5:221-35. [Crossref]
- Patak L, Wilson-Stronks A, Costello J, et al. Improving patient-provider communication: a call to action. J Nurs Adm 2009;39:372. [Crossref] [PubMed]
- Houts PS, Doak CC, Doak LG, et al. The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence. Patient Educ Couns 2006;61:173-90. [Crossref] [PubMed]
- U.S. Office of Personnel Management. Position Classification Standard for Diagnostic Radiologic Technologist Series, GS-0647 [Internet]. U.S. Office of Personnel Management [cited 2015 Oct 4]. Available online: https://www.opm.gov/policy-data-oversight/classification-qualifications/classifying-general-schedule-positions/standards/0600/gs0647.pdf