
An observation of massive lumbar disc prolapse
Introduction
Lumbar disc herniations (LDH) are common findings, but despite this, most do not cause clinical symptoms. A study of asymptomatic individuals with no lumbar-related symptoms, revealed that 30% demonstrated major abnormality on magnetic resonance imaging (MRI) (1). The natural history of these lesions is to spontaneously resorb which is correlated to the clinical outcome (2,3). Indeed, the predominant treatment modality is accepted to be non-operative in the form of analgesia, physiotherapy and guided-injections (4-6). However, there is little literature regarding the non-operative treatment of the massive LDH, which has been defined as one which occupies at least 50% of the spinal canal on axial MRI scans (7). These lesions raise the fear that they may lead to cauda equina syndrome if left alone and therefore are more likely to be treated surgically.
Following on from the work of Cribb et al. (7), we present an observational study from the same institution of 17 patients diagnosed with massive LDH who chose not to have surgery.
Methods
Our institution is a tertiary referral centre that accepts referrals predominantly from the West Midlands and North Wales regions in the United Kingdom. To be included in this observational study, patients had to have a ‘massive’ LDH on their initial MRI scan (Figure 1); have no symptoms of cauda equina syndrome; and had to opt for non-operative management. We reviewed 17 consecutive patients between January 2014 and August 2017 with confirmed ‘massive’ LDH who chose not to have surgery. These patients initially presented with back pain and radiculopathy and were referred to the general spinal clinic electively by their general practitioner (14 patients) or a musculoskeletal triage service (3 patients), who organized their initial MRI scan.
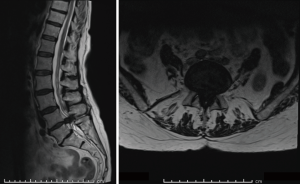
There were 6 female patients and 11 male patients with a mean age of 42 (27 to 75). All patients already had MRI scans performed on presentation to the spine clinic. The herniations were classified as previously described by Fardon (8). A disc herniation was a protrusion, if in any plane on an axial MRI, the greatest distance between the edge of the disc material beyond the disc space was less than the distance between the edges of the base in the same plane. An extrusion was where the greatest distance between the edge of the disc material beyond the disc space was greater than the distance between the edges of the base in the same plane. A sequestration was one where the offending disc material had completely lost continuity with the parent disc.
The patients were examined for symptoms of cauda equina syndrome and their diagnosis was explained to them. They were counselled extensively on the management options including the benefits and complications and risks of surgery. These patients were managed non-operatively because, either their symptoms were improving or minimal, or they wanted to pursue transforaminal epidural steroid injections. Patients were educated on the symptoms of cauda equina syndrome and were advised to seek urgent medical attention should they develop these symptoms. Patients were followed-up appropriately depending upon their history and examination findings.
Results
Eight of the disc herniations were classed as extrusions and nine were sequestrations, there were no protrusions. Three of the herniations were at L3–4, six at L4–5 and eight at L5–S1.
Patients were followed up for an average time of 209 days (0 to 1,005 days). Two patients were discharged at their first clinic appointment as their symptoms had almost completely resolved. Three patients went on to have transforaminal epidural steroid injections, with two of these making a significant improvement. The remaining patient had persisting radicular symptoms, but with no features of cauda equina syndrome, and was therefore listed for surgery electively. However, this patient was subsequently deemed unfit for surgery and this was therefore cancelled. Upon follow-up, this patient’s pain had improved significantly.
Of these 17 patients, all except one patient had back pain and leg pain. Seven of these patients stated that their back pain was the main problem over the leg pain. One patient complained of leg pain only. Only three patients had weakness in the corresponding myotome and this was measured to be grade four, according to the Medical Research Council (MRC) scale, in all of these patients. Seven patients were found to have altered sensation in the corresponding dermatome on testing with light touch. Nine patients had a positive straight leg raise test, with a positive test indicated by exacerbation of their leg pain.
One patient developed impending cauda equina syndrome after initial presentation and a repeat MRI scan revealed progression of the disc herniation. She went on to have urgent discectomy 84 days after her initial presentation to the spinal clinic with no post-operative complications.
All remaining patients had no complications and had complete or significant resolution of their pain and were safely managed with observation alone.
Discussion
The natural history of LDH is to spontaneously resorb, although not fully understood, it is postulated to occur with an inflammatory reaction (9) mediated by macrophages (10). The nucleus pulposus is normally a site of immunological privilege whilst surrounded by the annulus fibrosus, until a herniation exposes it to the immune system which initiates the inflammatory reaction (11). The macrophages have an essential role in regression of the herniation through a process of phagocytosis and the rim enhancement seen on contrast MRI is thought to represent neovascularization (12). Previous studies have shown that larger disc herniations do decrease in size and to a greater extent than smaller herniations (3,13).
Of our 17 cases of massive LDH, 8 were at L5–S1 (47%) and 6 were at L4–5 (35%). The capaciousness of the spinal canal at these levels and the relatively fewer nerve roots is likely to account for the fact that massive LDH at these levels is less likely to cause compression resulting in cauda equina syndrome. Indeed, a meta-analysis of 322 patients (14) with cauda equina secondary to LDH showed that only 16% were at L4–5 and 22% were at L5–S1. Most of the herniations were at L1–2 (27%) of which there were none in our series.
A systematic review by Jacobs et al. showed that although early surgery for sciatica provided short-term relief of leg pain, there was no significant difference between the clinical outcomes following surgery or non-operative management at 1 and 2 years (15). They also emphasize the weak evidence in the literature due to the limited number of studies.
However, there are few studies which look at the non-operative management of massive LDH as their impressive appearance on MRI raise the fear that they may lead to cauda equina syndrome. The first study from our institution (7), reported on 15 patients with massive LDH who were managed non-operatively. Repeat MRI on average two years later, revealed resolution of the LDH in 14 patients; one patient went on to have surgery for persistent pain and no patients developed cauda equina syndrome. Similarly, Benson et al. reported on 37 patients with non-operatively managed LDH with an 83% success rate as measured by resolution of symptoms. Four patients required discectomy for persistent or recurrent pain (16). Whilst none of their patients developed cauda equina syndrome, one of our 17 patients developed impending cauda equina syndrome and therefore this highlights the need to educate and fully inform patients of this potential complication when reviewing them.
As an alternative to surgery, transforaminal epidural steroid injections have also been used to treat massive LDH with a good success rate (17). Indeed, three of our patients chose this management option with two reporting an improvement in their symptoms.
Furthermore, spinal surgery is associated with significant complications: the incidence of dural tears is reported to be up to 16% (18) depending upon the complexity; the incidence of postoperative infection following spinal surgery is reported to be up to 4.4% (19); and Fandiño et al. reported reoperation rates of 7% due to recurrent or persistent symptoms (20). Also, it appears that surgery on large discs causing cauda equina syndrome is associated with a higher complication rate with intra-operative complications occurring in 11.56% of cases and inadvertent durotomy in 9.5% of cases (21).
There is varying opinion in the literature with regards to the correlation between the size of the LDH and clinical symptoms. Some studies have found a strong correlation between the resorption of the LDH and improvement of symptoms (3,22), whilst others have found no correlation between the two (3,15). Compression, therefore, is unlikely to be the only cause of symptoms and inflammation is likely to have a role in the causation (23). This raises the possibility that LDH and indeed massive LDH are likely to be underdiagnosed, with many asymptomatic individuals never requiring any investigation or treatment.
We realize the limitation in our study with the small sample size and the variability of follow-up period. However, the incidence of patients with symptomatic massive LDH but without cauda equina syndrome is probably low. Additionally, as our institution is the regional spinal referral centre for several hospitals covering a large catchment area, any patients requiring further spinal assessment or surgery are referred to us. This provides us with not only a large demographic, but also reasonable confidence that patients are followed-up effectively and comprehensively.
A further limitation is that not all patients had repeat MRI to look for resorption of the herniation and how this correlated to clinical symptoms. The reason for this was that patients were fully educated on red-flag signs and investigations were only performed for developing or persistent symptoms. Furthermore, it is already well documented how the massive LDH progresses with time in repeat imaging (7).
Out of our series of 17 patients only 1 developed impending cauda equina syndrome, and once operated on emergently, this patient made a full recovery. Unless patients develop progression of the LDH or a recurrent prolapse, patients are highly unlikely to develop cauda equina syndrome after they are initially reviewed.
Conclusions
We conclude that the massive LDH can be safely managed non-operatively providing patients are examined for cauda equina syndrome and are fully educated on the need to represent urgently should red-flag symptoms develop.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained from local institutional review boards (No. CARMS-00331).
References
- Baker ADL. Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatic Subjects. A Prospective Investigation. In: Banaszkiewicz PA, Kader DF. editors. Classic Papers in Orthopaedics, London: Springer London, 2014:245-7.
- Takada E, Takahashi M, Shimada K. Natural history of lumbar disc hernia with radicular leg pain: Spontaneous MRI changes of the herniated mass and correlation with clinical outcome. J Orthop Surg (Hong Kong) 2001;9:1-7. [Crossref] [PubMed]
- Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine (Phila Pa 1976) 1990;15:683-6. [Crossref] [PubMed]
- Mathews JA, Mills SB, Jenkins VM, et al. Back pain and sciatica: controlled trials of manipulation, traction, sclerosant and epidural injections. Br J Rheumatol 1987;26:416-23. [Crossref] [PubMed]
- Derby R, Kine G, Saal JA, et al. Response to steroid and duration of radicular pain as predictors of surgical outcome. Spine (Phila Pa 1976) 1992;17:S176-83. [Crossref] [PubMed]
- Riew KD, Yin Y, Gilula L, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am 2000;82-A:1589-93. [Crossref] [PubMed]
- Cribb GL, Jaffray DC, Cassar-Pullicino VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br 2007;89:782-4. [Crossref] [PubMed]
- Fardon DF, Milette PC. Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 2001;26:E93-113. [Crossref] [PubMed]
- Virri J, Grönblad M, Seitsalo S, et al. Comparison of the prevalence of inflammatory cells in subtypes of disc herniations and associations with straight leg raising. Spine (Phila Pa 1976) 2001;26:2311-5. [Crossref] [PubMed]
- Rothoerl R, Woertgen C, Holzschuh M, et al. Macrophage tissue infiltration, clinical symptoms, and signs in patients with lumbar disc herniation. A clinicopathological study on 179 patients. Acta Neurochir (Wien) 1998;140:1245-8. [Crossref] [PubMed]
- Tohmura T. Fate of epidurally sequestrated disc; MRI and an immuno-histological study of herniated nucleus pulposus of the lumbar spine. Clin Orthop Surg 1994;29:413-21.
- Doita M, Kanatani T, Harada T, et al. Immunohistologic study of the ruptured intervertebral disc of the lumbar spine. Spine (Phila Pa 1976) 1996;21:235-41. [Crossref] [PubMed]
- Bozzao A, Gallucci M, Masciocchi C, et al. Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology 1992;185:135-41. [Crossref] [PubMed]
- Ahn UM, Ahn NU, Buchowski JM, et al. Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine (Phila Pa 1976) 2000;25:1515-22. [Crossref] [PubMed]
- Jacobs WC, van Tulder M, Arts M, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J 2011;20:513-22. [Crossref] [PubMed]
- Benson RT, Tavares SP, Robertson SC, et al. Conservatively treated massive prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl 2010;92:147-53. [Crossref] [PubMed]
- Hong SJ, Kim DY, Kim H, et al. Resorption of Massive Lumbar Disc Herniation on MRI Treated with Epidural Steroid Injection: A Retrospective Study of 28 Cases. Pain Physician 2016;19:381-8. [PubMed]
- Khan MH, Rihn J, Steele G, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 2006;31:2609-13. [Crossref] [PubMed]
- Fang A, Hu SS, Endres N, et al. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 2005;30:1460-5. [Crossref] [PubMed]
- Fandiño J, Botana C, Viladrich A, et al. Reoperation after lumbar disc surgery: results in 130 cases. Acta Neurochir (Wien) 1993;122:102-4. [Crossref] [PubMed]
- Venkatesan M, Nasto L, Haddad S, et al. Cauda equina syndrome: a single centre review of 147 operated cases. Spine J 2017;17:S6. [Crossref]
- Bush K, Cowan N, Katz DE, et al. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow-up. Spine (Phila Pa 1976) 1992;17:1205-12. [Crossref] [PubMed]
- Siddall PJ, Cousins MJ. Spinal pain mechanisms. Spine (Phila Pa 1976) 1997;22:98-104. [Crossref] [PubMed]


