Robotic versus freehand S2 alar iliac fixation: in-depth technical considerations
Introduction
Rigid internal fixation is necessary for successful reduction, stabilization and eventual fusion in spinal deformity surgery. The often-excessive stress across the lumbosacral junction creates a difficult situation for the deformity surgeon in terms of obtaining stable fixation. The use of bilateral S1 tri-cortical screws alone may lead to loss of fixation, pseudarthrosis, and other poor outcomes (1,2). Sacropelvic fixation, particularly in the form of S2 alar-iliac (S2AI) screws decreases the amount of strain on the S1 screws and may help to prevent these complications. These screws can be utilized in osteoporotic patients with long constructs, patients with significant pelvic obliquity, those with unstable sacral fractures, three column lumbar osteotomies, reduction of high grade spondylolisthesis, and extensive lumbosacral tumor resection (3-5).
S2AI screws have a different starting point and corridor than traditional iliac screws. The starting point for the S2AI screw is 1mm inferior and lateral to the S1 dorsal foramen. The screw is angulated 40° inferiorly and 40° laterally from a line connecting the PSIS and unlike iliac bolts, crosses the sacroiliac (SI) joint (6,7). The traditional S2AI technique, as described by Drs. Sponseller and Kebaish et al., was fluoroscopically guided to prevent damage to surrounding structures in the sciatic notch and pelvis. Recently, Shillingford et al. have described the method for freehand placement of these screws without fluoroscopic guidance (8).
Floor and bone-mounted robotic systems with surgical arms have been developed in order to increase the precision of S2AI screw placement and to provide the surgeon with the ability to plan the trajectory of the screw pre-operatively and intra-operatively through use of computed tomography (CT) imaging. Robotic assisted S2AI technique was shown to be safe and effective with over 95% accuracy and without complication due to robotic assisted spinopelvic fixation (9). Herein, we report the first study in the literature to compare the technical aspects of robotic and freehand S2AI screw insertion.
Robotic S2AI surgical technique
Preoperative surgical plan
- Obtain thin cut (1 mm) CT scan of patient for preoperative planning;
- Using proprietary software, plan S2AI screw start points, trajectories, diameters and lengths.
Selection of appropriate bone mount platform
Note: four options are provided for affixing the bone mount bridge (BMB) to the patient’s bony anatomy: clamp, dual clamp, Schanz screw, or link bridge. Our preferred technique involves the insertion of a Schanz screw into the iliac crest. When fixed to the iliac crest, the Schanz Screw platform provides operational reach from vertebrae L3 through S2 via a posterior incision.
- Make a stab incision over the iliac crest at the desired site;
- Load the Schanz screw into the power drill and drill the screw into the iliac crest at the desired site;
- Place the Schanz screw ball adapter onto the Schanz screw and lock it into position using the universal screwdriver.
Selecting the BMB and affixing to the bony anatomy
Note: the BMB connects the Schanz screw to the base of robotic arm. The bridges are available in four positioning angles: 0, 15, 30 and 45 degrees. The surgeon must select the most appropriate angle for the patient’s anatomy.
- Hold BMB in position ready to mount onto the draped surgical arm;
- Align bridge locating pins and screws with the grooves and screw holes located on the surgical arm;
- Fasten two screws into place using the supplied screwdriver until the BMB locks into place;
- Adjust BMB to the required angle to match the patient’s anatomy and then attach the BMB to the Schanz screw;
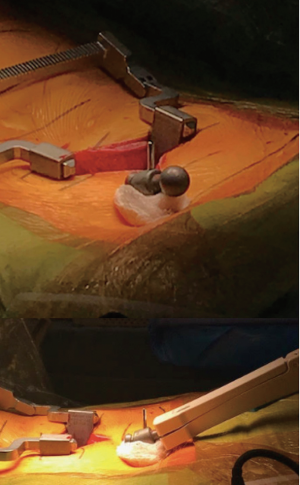
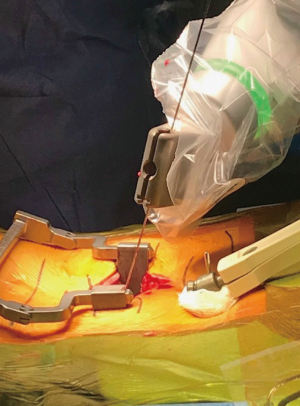
- Prior to commencing operation, adjust the BMB to the corresponding angle of the patient’s anatomy and then attach the BMB to the Schanz screw (Figure 1);
- After unlocking the shoulder joints, bring the BMB toward the platform and approximate the end of the BMB to the ball, advance the BMB to receive the ball, and tighten the screw at the tip of the BMB.
Registration of the robotic guidance with fluoroscopic images
Note: the robotic surgical guidance platform requires the surgeon to capture a number of AP and oblique images with the surgical arm in position. In the following steps, while each of the images is being acquired by the robotic software, it is monitoring the position of the surgical arm and basing its calculations on that position.
- Mount the 3D marker on top of the target extender and screw it in position with the 3D marker screw (Figure 2);
- Insert the other end of the target extender into the arm guide;
- Slide the target extender over the base of the arm guide taking care to align the notch at the end of the target extender with the locating pin on the arm guide;
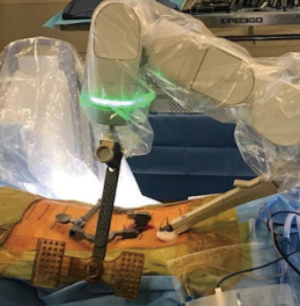
- Slide the target extender screw (Figure 3) into the top of the arm guide, then screw it in completely. It is an important distinction to understand that the arm guide connects the target extender to the tip of the robotic arm, while the BMB connects the Schanz screw to the base of the robotic arm.
- Lock the target extender into position with the target extender screw;
- Acquire the AP and oblique fluoroscopic image. Ensure the entire region of interest and 3D marker pattern are visible in the image;
- When the desired image is displayed in the acquisition window, tap to capture button to capture and save the image.
Activating the surgical arm and commencing instrumentation
Note: prior to moving the surgical arm to the preoperatively planned screw trajectories, a list of suggested optimal configurations for reaching the trajectory is available, and the surgeon has the option to run an animated simulation of movement of the surgical arm. Once the trajectory is confirmed, the target extender is detached from the arm guide. After computer verification, a message will appear on the surgical monitor stating that the robot is ready for drilling and instrumentation.
- Make an incision with a number 11 scalpel blade by inserting the scalpel through the arm guide and puncturing the skin/muscle fascia;
- Take the blunt trocar and insert it into the cannula of the indicated length, then slide the indicated cannula through the arm guide (Figure 4);
- Push and rotate the blunt trocar toward the bony anatomy clearing a path through the muscles for the cannula—gently tap the bony anatomy with the blunt trocar. It is very important to note that if the blunt skives off of the bony surface, then the docking surface is inclined and needs to be flattened;
- Slide the cannula over the blunt trocar until the engraved line is seen near the top of the trocar;
- Remove the blunt trocar and leave the cannula in position;
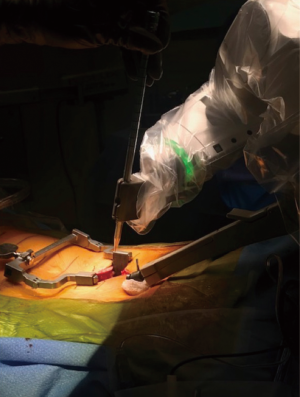
- Take the drill guide with the same color code as the cannula and insert it into the cannula (Figure 5);
- With the mallet, gently tap the top of the drill guide. Check that the drill guide is well docked by applying gentle torque to its head;
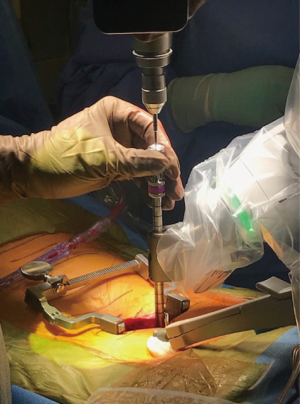
- Take the appropriate (long/short, 3 or 2.4 mm) drill bit and secure it within the high-speed drill;
- Without drilling, insert the drill bit into the drill guide until it contacts bone;
- While holding the high-speed drill with one hand and the drill guide with the other, begin rotation of the drill bit to maximum speed and insert the drill bit into the bone with moderate force;
- Remove the drill bit and insert the reduction tube through the drill guide;
- Insert a K-wire into the reduction tube by gently tapping the wire and ensuring its purchase in bone;
- Remove the drill guide, cannula, and reduction tube, while leaving the K-wire in place;
- Gently pull the K-wire through the slit on the robotic arm (Figure 6), allowing it to proceed in its movement to the next trajectory and leaving the K-wire seated in bone;
- Repeat from step 1 until all required trajectories for the segment are drilled and a K-wire is placed in each one;
- After K-wire placement, tapping proceeds in typical fashion. A cannulated tap is inserted over the K-wire;
- On removal of the tap, downward pressure is placed on the K-wire to prevent inadvertent removal;
- A cannulated screw is placed over the K-wire into the tapped and predetermined trajectory.
Freehand S2AI surgical technique
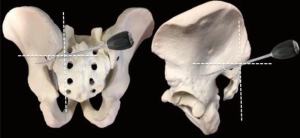
Note: the S2AI screw is most commonly inserted from the contralateral side of the patient. Freehand screw placement begins with subperiosteal dissection of the S2AI starting point and the posterior superior iliac spine (PSIS). The entry point is located just lateral to the midpoint of the S1 and S2 foramen, and mediolaterally, it should be in line with the S1 screw (Figure 7, cross-section of dotted lines).
- Use a high-speed burr to establish a 5 mm deep cortical breach at the screw entry point;
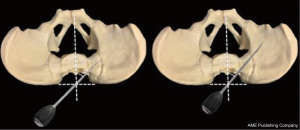
- A curved blunt-tipped gearshift is advanced toward the SI joint with the curved tip directed posteriorly (dorsally) to avoid anterior perforation;
- Direct the probe towards the anterior inferior iliac spine (AIIS) by aiming perpendicular to the sacral laminar slope and cephalad to the inferior tip of the PSIS, thus avoiding the sciatic notch inferiorly (Figure 7);
- Remove the gearshift when the hard, cortical surface of the SI joint has been reached, typically at a depth of about 50 mm;
- Palpate the tract with a flexible ball-tipped pedicle sounding probe to confirm an intraosseous trajectory for the screw with the presence of a floor and four intact bony walls (anterior, posterior, superior and inferior);
- Reinsert the gearshift to the original depth;
- Rotate the curved tip to point anteriorly (ventrally) as the gearshift is advanced through the SI joint (Figure 8);
- Advance the gearshift toward the AIIS in a smooth consistent manner to a depth of about 70–90 mm;
- Remove the gearshift and again confirm intraosseous placement with the ball-tipped pedicle sounding probe;
- Use a hemostat clamp to document screw length on the ball-tipped probe;
- Under-tap the S2AI trajectory 1–2 mm less than desired screw diameter;
- Once again, confirm the intraosseous path and screw length;
- The screw is then inserted (typically with a powered drill) in the direction of the established S2AI path.
Discussion
There are a number of reasons for the increased use of S2AI screws for spinopelvic fixation in spinal deformity and complex lumbar degenerative surgery. Because the screws cross three cortical surfaces, including the SI joint, they are afforded increased biomechanical stability compared to traditional methods of iliac fixation. After the screw crosses the SI joint, it comes into close proximity to the dense area just superior to the greater sciatic notch anchoring the screw in high quality bone. Additionally, due to their entry point and trajectories, these screws align well with proximal instrumentation and do not require extensive dissection or offset connectors (10).
The corridor for S2AI screws, although ideal in terms of fixation and screw prominence, is in close proximity to several important neurological and vascular structures. Inferiorly lies the sciatic foramen, while posteriorly and postero-superiorly lies the superior gluteal vessels and nerves (11-13). Anterior structures in the pelvis include the bowel, nerve roots (L5 and S1), sympathetic chain ganglia, and common iliac vessels (14). Therefore, accurate and efficient placement of S2AI screws is necessary to avoid inadvertent injury to these associated neurovascular structures.
In a propensity matched analysis of robotic versus freehand S2AI screws, Shillingford et al. reported overall accuracy rates of 97.8% and 94.9%, respectively. In both groups, there were no inferior screw violations, which would potentially place the sciatic nerve and superior gluteal neurovascular bundle at risk. There was an overall 5% rate of posterior cortical violation and 2% incidence of anterior cortex violation (8). Similarly, Hu and Lieberman reported no breaches or complications in a series of 35 robotically placed S2AI screws (15).
The S2AI technique allows for rigid and low-profile spinopelvic fixation in spinal deformity and complex lumbar degenerative surgery. Both freehand and robotic-guided S2AI screw placement prove to be safe and reliable techniques for achieving spinopelvic fixation. We describe a step-by-step protocol of achieving safe and effective spinopelvic fixation with both robotic and freehand techniques (16).
Acknowledgements
None.
Footnote
Conflicts of Interest: JL Laratta, MD—Research funding: Orthopaedic Science Research Foundation, Norton Healthcare; Consulting: Evolution Spine; Review Board: Spine, Global Spine Journal. JL Gum, MD—Consultant: Medtronic, Dupuy, Alphatec, Stryker, Acuity, K2M, Nuvasive, Pacmed (1/15); Royalties: Acuity; Honorarium: MiMedx (11/14), Pacira Pharmaceuticals; Advisory/Editorial Board: American Journal of Orthopedics; Grants: Fischer Owen Fund—Travel Funds (12/31/16); Journal Reviewer: The Spine Journal, American Journal of Orthopedics; Research Support: Integra, Intellirod Spine Inc., Pfizer, International Spine Study Group Foundation—Funds to institution only, NuVasive—Database support only; Norton Healthcare: Research Funding. LG Lenke, MD—Board Membership OREF and GSO: Unpaid position; Personal Fees: Consultancy—Dupuy Synthes Spine, K2M, Medtronic—monies donated to a charitable foundation; Personal Fees: Expert Testimony—Fox Rothschild, LLP; Grants: AO Spine; Scoliosis Research Society; DePuy Synthes Spine; Setting Scoliosis Straight Foundation; EOS—monies paid to institution; Royalties: Medtronic; Quality Medical Publishing; Travel accommodations/meeting expenses: AO Spine; Broadwater, Seattle Science Foundation; Scoliosis Research Society; The Spinal Research Foundation—Reimbursement for airfare/hotel only; Fellowship Grant: AO Spine North America—institutional support for fellowship; Grant: Philanthropic Research funding—Fox Family Foundation; Evans Family. RA Lehman, MD—Grant: PRORP (Department of Defense Peer Reviewed Orthopaedic Research Program—paid directly to organization; Personal Fees/Financial Support: Dupuy Synthes Spine—Honoraria for Speakers Bureau, Travel paid for any speaking arrangements; Stryker—Honoraria for Speakers Bureau, Travel paid for any speaking arrangements; Medtronic—Consulting fees, Honoraria for Speakers Bureau, Travel paid for any speaking arrangements. The other authors have no conflicts of interest to declare.
References
- Edwards CC 2nd, Bridwell KH, Patel A, et al. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976) 2004;29:1996-2005. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976) 2006;31:2329-36. [Crossref] [PubMed]
- Perra JH. Techniques of instrumentation in long fusions to the sacrum. Orthop Clin North Am 1994;25:287-99. [PubMed]
- Rosner MK, Ondra SL. Sacropelvic fixation in adult deformity. Semin Spine Surg 2004;16:107-13. [Crossref]
- Bridwell KH, Lewis SJ, Rinella A, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am 2004;86-A Suppl 1:44-50. [Crossref] [PubMed]
- Chang TL, Sponseller PD, Kebaish KM, et al. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976) 2009;34:436-40. [Crossref] [PubMed]
- O'Brien JR, Yu WD, Bhatnagar R, et al. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976) 2009;34:E439-42. [Crossref] [PubMed]
- Shillingford JN, Laratta JL, Tan LA, et al. The Free-Hand Technique for S2-Alar-Iliac Screw Placement: A Safe and Effective Method for Sacropelvic Fixation in Adult Spinal Deformity. J Bone Joint Surg Am 2018;100:334-42. [Crossref] [PubMed]
- Laratta JL, Shillingford JN, Lombardi JM, et al. Accuracy of S2 Alar-Iliac Screw Placement Under Robotic Guidance. Spine Deform 2018;6:130-6. [Crossref] [PubMed]
- Stevens DB, Beard C. Segmental spinal instrumentation for neuromuscular spinal deformity. Clin Orthop Relat Res 1989.164-8. [PubMed]
- Altman DT, Jones CB, Routt ML Jr. Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma 1999;13:220-7. [Crossref] [PubMed]
- Marmor M, Lynch T, Matityahu A. Superior gluteal artery injury during iliosacral screw placement due to aberrant anatomy. Orthopedics 2010;33:117-20. [Crossref] [PubMed]
- Collinge C, Coons D, Aschenbrenner J. Risks to the superior gluteal neurovascular bundle during percutaneous iliosacral screw insertion: an anatomical cadaver study. J Orthop Trauma 2005;19:96-101. [Crossref] [PubMed]
- Esses SI, Botsford DJ, Huler RJ, et al. Surgical anatomy of the sacrum. A guide for rational screw fixation. Spine (Phila Pa 1976) 1991;16:S283-8. [Crossref] [PubMed]
- Hu X, Lieberman IH. Robotic-guided sacro-pelvic fixation using S2 alar-iliac screws: feasibility and accuracy. Eur Spine J 2017;26:720-5. [Crossref] [PubMed]
- Mazor Robotics Technical Guide, Mazor Robotics Ltd.; Caesarea, Israel.