Spinal tumour: primary cervical extradural meningioma at an unusual location
Introduction
The vast majority of meningiomas arise in intracranial, intraspinal or orbital locations. Amongst the intraspinal location, meningiomas account for 25% to 46% of primary spinal neoplasms, while the incidence of spinal meningiomas is 7.5% to 12.7% of all meningiomas (1). In the spine, most meningiomas occur in the thoracic region located intradural extramedullary. However, a purely extradural position at cervical spine as reported in this paper is quite exceptional and to the best of our knowledge, only 9 cases have been reported in the literature so far (2). This case report highlights the fact that, although extremely rare, the possibility of an extradural mass being a meningioma does exist. The case is discussed in this paper for its exceptional location. The origin, clinical course, radiological features, pathological findings, and surgical treatment are discussed based on a review of the literature.
Case presentation
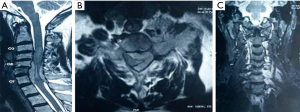
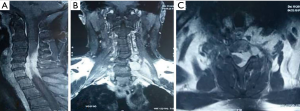
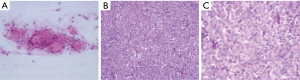
A 50-year-old male presented with complaints of weakness in both upper limbs for the last six months followed by gradual numbness in both upper limbs for the last 5 months. On examination, the patient had muscle weakness in both the upper limbs (motor strength of 3/5). There was no other neurologic deficit. The magnetic resonance imaging (MRI) of the cervical spine and cervicothoracic junction revealed marrow signal abnormality involving the C6–C7 vertebral bodies along with the posterior elements showing hypointense signal on T1-weighted (T1W) images and hyperintense signal on T2-weighted/short tau inversion recovery sequence (T2W/STIR) images. An associated soft tissue mass was seen in the left intraspinal extradural compartment extending from C5 to C7 levels, encircling and compressing the thecal sac and cervical cord, which was already displaced rightwards with intramedullary cord hyperintensity, suggesting significant cord edema. The mass had widened the left C5–6, C6–7 neural foramina with extension into the left paraspinal soft tissues (Figure 1). Post-gadolinium images revealed intense homogenous contrast enhancement in the intraspinal and extra spinal soft tissue components (Figure 2). Based on the radiological findings, differential diagnoses of Pott’s spine, round cell tumor and neurogenic tumor were considered. Based on the clinicoradiological correlation, the patient underwent a C3–C6 laminectomy with a provisional diagnosis of neurofibroma, exposing an entirely extradural mass adherent to the dura and ligamentum flavum. It was a grayish white, non-suckable and moderately vascular mass. Near total excision was done. The per-operative specimen sent to the histopathology laboratory was subjected to squash smear preparation. Hematoxylin and eosin (HE) and Toluidine blue (TB) stained squash smears showed a meningothelial tumor (Figure 3A). Based on the above findings a diagnosis of meningioma was suggested on per-operative squash smears. The latter specimen, received in formalin for paraffin sections, showed sheets of meningothelial cells having ovoid nuclei with stippled chromatin and eosinophilic cytoplasm (Figure 3B,C). Histopathological diagnosis of meningothelial meningioma (World Health Organization (WHO) Grade I) was made. The patient showed marked improvement in the motor symptoms with almost full recovery in the postoperative course. The 1-year follow-up has showed considerable sustained improvement in the patient status.
Discussion
Meningiomas are mostly benign slow growing tumours arising in intracranial, intraspinal or orbital locations, intraventricular and epidural localizations are uncommon. Intraspinal meningiomas have a predilection to localize in the thoracic region located intradural extramedullary, being most likely derived from the meningothelial cells of the arachnoid layer. Nevertheless, they are rarely found in an extradural location, an anomaly that may be explained by the following hypotheses: (I) by proliferation of ectopic arachnoidal cells around the periradicular nerve root sleeves; or (II) by the displacement of the primitive embryonic remnants of the arachnoid mater and villi along the periradicular dura; or (III) by the migration of islands of arachnoid tissue into the extradural space (3,4).
These are generally slow growing tumours manifesting in the fourth to fifth decade, with a predilection for women. They rarely cause clinical symptoms at an earlier age (5). The symptomatology of meningiomas includes neurological signs and symptoms due to compression of adjacent structures; the specific deficits depend on tumour location. Spinal meningiomas present with pain, motor and sensory changes with sphincter disturbances.
Concerning neuroimaging, MRI is recommended for the diagnosis of spinal meningiomas. In extradural spinal lesions, the differentials included are: metastatic lesions, schwannoma, neurofibroma, chordomas, synovial cyst, infectious etiology and meningioma. MRI of spinal meningiomas on T1W images exhibit signal intensity similar to that of spinal cord and does not show significant increased signal intensity on T2W images. However, contrast enhancement is immediate and homogeneous (5). Radiological features revealing lack of foraminal extension suggests a diagnosis of meningioma over schwannoma or neurofibromas. The latter two tumours demonstrate high signal intensity on T2W images, cystic changes with homogeneous enhancement (6). Chordoma is isotense to marrow on a T1W image while synovial cyst is contiguous to the joint, is spherical and measures approximately 1–2 cm (7).
Histopathology of spinal meningiomas usually exhibits meningothelial, fibroblastic, transitional and psammomatous patterns. In most of the case reports, meningothelial and psammomatous variants have been described (Table 1).
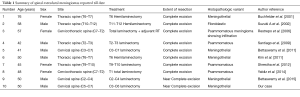
Full table
Meningioma is a surgically-treated disease. Concerning the management, the best therapeutic approach for these tumours is the total removal of the tumour with wide margins, whereas adjuvant therapy after resection of atypical (WHO grade II) or malignant (WHO grade III) meningiomas should be considered. The major prognostic factors regarding WHO grade II and grade III meningiomas are estimates of recurrence and overall survival (8). The major clinical factor in recurrence is the extent of resection which is invariably influenced by tumour site, extent of invasion and attachment to vital intracranial/intraspinal structures. In terms of histopathology, some variants are more likely to recur. The most useful morphological predictor of recurrence is the overall WHO grade. Benign meningiomas have recurrence rates of approximately 7–25%, atypical meningiomas show recurrence rates of 29–52% and anaplastic meningiomas recur in 50–94% of cases (9). Meningiomas with malignant histological features are associated with shorter survival times; approximately 2–5 years depending largely on the extent of resection (10).
Conclusions
Extradural meningiomas are very rare lesions. To the best of our knowledge, only nine cases have been reported to date. Although simple to diagnose on histopathology, meningiomas at unusual sites can pose a preoperative radiologic dilemma, as the radiologic findings overlap with more common extradural spinal masses like peripheral nerve sheath tumors or metastatic lesions. Surgery is the only effective treatment, and its goal should be the radical resection of the lesion to avoid recurrence. When radical resection of tumor poses a risk, however, subtotal resection can be a wise option.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ben Nsir A, Boughamoura M, Mahmoudi H, et al. Uncommon progression of an extradural spinal meningioma. Case Rep Surg 2014;2014:630876. [Crossref] [PubMed]
- Bettaswamy G, Ambesh P, Das KK, et al. Extradural spinal meningioma: Revisiting a rare entity. J Craniovertebr Junction Spine 2016;7:65-8. [Crossref] [PubMed]
- Zevgaridis D, Thomé C. Purely epidural spinal meningioma mimicking metastatic tumor: case report and review of the literature. Spine (Phila Pa 1976) 2002;27:E403-5. [Crossref] [PubMed]
- Tuli J, Drzymalski DM, Lidov H, et al. Extradural en plaque spinal meningioma with intraneural invasion. World Neurosurg 2012;77:202.e5-13. [Crossref] [PubMed]
- Gambardella G, Toscano S, Staropoli C. Epidural spinal meningioma: role of magnetic resonance in differential diagnosis. Acta Neurochir (Wien) 1990;107:70-3. [Crossref] [PubMed]
- El Khamary SM, Alorainy IA. Case 100: spinal epidural meningioma. Radiology 2006;241:614-7. [Crossref] [PubMed]
- Ross J, Brant-Zawadzki M, Chen M, et al. Meningioma. In: Diagnostic Imaging: Spine. 1st ed. Salt Lake City, UT: Amirsys; 2004:IV1-78-IV1-81.
- Jääskeläinen J. Seemingly complete removal of histologically benign intracranial meningioma: late recurrence rate and factors predicting recurrence in 657 patients. A multivariate analysis. Surg Neurol 1986;26:461-9. [Crossref] [PubMed]
- Marciscano AE, Stemmer-Rachamimov AO, Niemierko A, et al. Benign meningiomas (WHO grade I) with atypical histological features: correlation of histopathological features with clinical outcomes. J Neurosurg 2016;124:106-14. [Crossref] [PubMed]
- Aizer AA, Bi WL, Kandola MS, et al. Extent of resection and overall survival for patients with atypical and malignant meningiomas. Cancer 2015;121:4376-81. [Crossref] [PubMed]


