Corpectomy and expandable cage replacement versus third generation percutaneous augmentation system in case of vertebra plana: rationale and recommendations
Introduction
Each year, there are approximately 5 million of new vertebral fractures worldwide (1). Due to the increase in life expectancy, the incidence of osteoporosis vertebral fractures (OVFs) is becoming increasingly high. In Italy, the incidence of OVF is very high, resulting in a substantial increase in health care costs (2). OVF prevalence in Italy was estimated to be about 61,000 in the 2008, with a 6.3% increase over 7 years (3). Although the incidence is approximately 189.0 events/100,000 inhabitants, this value doubles for the population between 75 and 95 years (3).
These fractures usually affect the thoracolumbar junction and the lumbar spine. In the first, it is due to the mechanical characteristics of the transition zone and in the second it is the consequence of the sagittally oriented facet joints and of the absence of the costovertebral joints. In more than 70% of cases, type A compression fractures occur, in particular-A1-wedge fractures (according to Magerl/AO-spine classification). The compression fractures promote a progressive increase of the kyphosis deformity, resulting in an anterior weight shift and an anterior column overload, with promotion of the vertebral collapse and other OVFs (domino effect) (4). Therefore, the fracture reduction and the vertebral height recovery are the only treatments that can be considered curative (4).
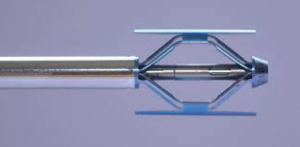
Among the mini-invasive techniques, vertebroplasty and balloon kyphoplasty proved to be effective to manage the OVFs, especially in the medically compromised patients. Both the approaches are reported to confer great pain relief, but unfortunately they have been proven to have many application limits and therefore they are not always achievable. In the 12% of the cases, several complications might occur, requiring more invasive surgical approaches (5). Although they could be very dangerous, they might represent the one and only chance to obtain the restoration of the anterior and middle column, in order to achieve the mechanical stability. The aim of this work is to evaluate the role of third generation percutaneous vertebral augmentation systems (Spine Jack®) (Figure 1) as alternative to the corpectomies and expandable cages replacement (X-Core® Adjustable VBR System) (Figure 2) in the treatment of vertebra plana (VP) as complication of the OVF.
Methods
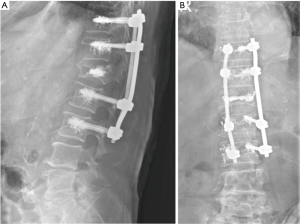
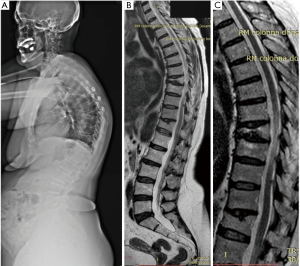
Spine Jack® is a new device for mechanical kyphoplasty (MK). It is a titanium implant designed to restore the height of the vertebral body in OVF, primary or secondary bone tumors, or traumatic fractures (A1, A2, A3.1 and type B in selected cases, according to AO classification) (6). The X-Core® adjustable VBR System is a vertebral body replacement device, indicated for use in the thoracolumbar spine (T1 to L5) to replace a diseased or damaged vertebral body caused by tumor or fracture, to restore height of a collapsed vertebral body and to achieve decompression of the spinal cord. It is an expandable titanium cage. Due to the wide footprint, the cage rests on the ring apophysis, enhancing biomechanical support. The cage was expanded in order to reduce partially the local kyphosis using the superior and inferior vertebral endplates as points of fixation. It is intended to be used with supplemental internal spinal fixation systems (7). Since February 2016, 9 patients (2 men and 7 women; mean age 81 years) affected with VP due to OVF were subjected to surgical treatment. The thoracic spine was involved in 3 cases and the lumbar spine in 6 cases. In 8 patients the thoracolumbar junction was implicated. Among the 9 patients, 7 were treated by Spine Jack®. A corpectomy was performed only in two cases (thoracic level) through the X-Core® adjustable VBR System. Preoperative radiographic exams, computed tomography (CT), and magnetic resonance imaging (MRI) were performed in all cases. Clinical outcome measures included preoperative and postoperative Oswestry Disability Index (ODI), Visual Analog Scale pain score (VAS), neurologic examination, complications, estimated blood loss, and operating time. Postoperative radiographic evaluations were made at 1, 6, and 12 months. All patients were informed about the study procedures and they signed an informed consent form. Ethical approval was obtained from the ethics clearance committee of the hospital health administration. Statistical analyses were performed independently by a nonclinical investigator assistant. The data were analyzed using standard statistical software. The results were considered statistically significant if the P value was ≤0.05 for continuous variables.
Results
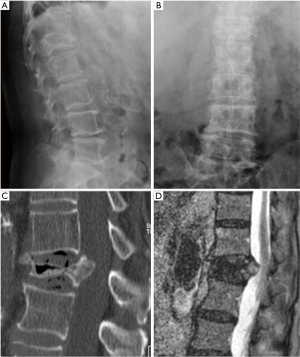
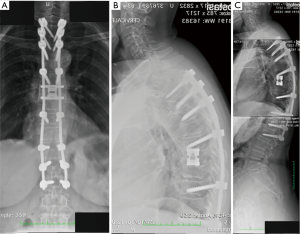
All the nine patients were in theory suitable for corpectomy and expandable titanium cage implant (7). But this approach was performed only in two of them. In fact, in 7 patients, a reconstruction of the anterior and medial spinal column was accomplished by third generation percutaneous vertebral augmentation systems (MK). In all the cases however a posterior fixation with rod and screws was always performed. The choice between one technique and the other one was made according to the signal in short tau inversion recovery (STIR) in the MRI sequences: in case of hyperintense signal to the level of the collapsed vertebra (VP), we decided for the percutaneous vertebral augmentation (Figures 3,4) (8). In absence or in case of very low STIR hyperintense signal, we chose for the standard corpectomy (Figures 5,6). Indeed, the presence of positive signal in the VP is in fact indicative of the reducibility of the vertebral soma. Moreover, in the cases of spinal canal compression the applicability of the third generation MK alone, without any posterior decompression, must not be excluded: it must be inferior to 1/3 and 2/3 respectively in case of fractures level above and below the spinal cord and any clinical signs of radicular compressions must not be identified. Otherwise, a direct posterior spinal cord decompression must be performed. Furthermore it is mandatory to evaluate the state of the anterior longitudinal ligament (ALL). In case of ossification of ALL at the level of the VP, MK has to be avoided, because a satisfactory correction of the vertebral height and a substantial management of the regional deformity might not be achieved. Mean follow-up was 18 months (range, 12–28 months). None of the patients experienced neurologic deterioration neither they showed a progression of local or regional deformity. No infections, dural tears, or spinal cord injuries occurred. No revision surgery was performed. In case of corpectomy the main blood loss and the mean surgical time were inevitably greater (9).
Discussion
VP is due to different pathological conditions, including eosinophilic granuloma, giant cell tumor, malignant tumor and especially trauma. All these pathologies can lead to the vertebral collapse (10). The radiological diagnosis of VP is based on different and limited criteria: the fall of the vertebral body, a normal adjacent intervertebral discs, an increased height of the intervertebral space by at least one third and an increased density of the collapsed vertebra (10). More easily, the VP can be identifiable as vertebrae that collapsed more than 75% of their original height (9). The vertebral body plays a significant role in the biomechanical stability of the spine and it is responsible for transmitting up to 80% of the axial load (10). With substantial destruction of the vertebral body, the anterior support and its reconstruction may be critical for the long-term sagittal alignment and biomechanical stability (11,12).
In case of anterior and middle column damage, the posterior pedicle screw fixation alone could not offer the sufficient stability and it may even result in an implant failure, due to the high implant strain (13). Similarly, this is the situation is created in the case of VP. Therefore, it is mandatory to restore the anterior and middle column. In theory, this is achievable in two different ways: by corpectomies and expandible cage replacement or by percutaneous vertebral augmentation systems (MK). Through a corpectomy and an anterior reconstruction it is possible to increase the construct stiffness and reduces the hardware strain. Furthermore, sometimes the vertebral body destruction may produce a medullary compression. In these cases the indirect decompression of the spine cord by ligamentotaxis alone, may result not efficient as the direct anterior decompression (14,15). In addition, the correction of the deformities, especially of the lordosis, may result not so easy. Generally, in case of VP the opportunity to perform a vertebral augmentation depends on the size of pedicle and the extent of the kyphosis, but above all, it is mandatory to evaluate the signal in STIR of the MRI sequences. Only in case of hyperintense signal to the level of the fractures it is possible to perform a reduction through the MK. So the time interval after fracture takes on a limited relevance. Now, even the importance of the post-traumatic kyphosis takes on a limited relevance. This had been true until the use of the Spine Jack® (4). In fact the balloon kyphoplasty can’t allow to control the high degree deformities, because these system is not able to produce high mechanical forces (16). On the contrary, Spine Jack® allows to treat even higher segmental kyphosis resulting in serious degrees of wedging, as in the case of VP (6). Spine Jack® is a titanium implant designed to restore the height of the vertebral body in OVF, primary or secondary bone tumors, or traumatic fractures (A1, A2, A3.1 and type B in selected cases, according to AO classification) (6). By transpedicular approach, the Spine Jack® is inserted into the vertebral body and gradually expanded. The distraction caused by the device reduces the fracture not only by ligamentotaxis (especially when acting on the ALL) but especially through a mechanical direct action (4). In fact the device includes a mechanical (as opposed to the hydraulic one of the balloon kyphoplasty) working system which allows a progressive and controlled reduction of the vertebral fracture. This feature facilitates the recovery of the collapsed vertebra and provides a tridimensional support in order to mechanically stabilize the vertebrae (17). After the reduction, PMMA is injected into the vertebral body. The use of two devices symmetrically positioned inside the vertebral body allows a homogeneous spreading of the PMMA (18,19). The expansion of the device causes a preferential direction of the flow of the PMMA thus reducing the risk of leakage. When injected, the inter-digitation of the PMMA produces a large contact area below the midline; this is essential in order to confer stability to the vertebral body. The device has a “self-locking security system” that allows to significantly reduce the risk of vertebral endplate breakage (6,19).
In case of corpectomy and expandable titanium cage implant, the procedure-related complication rate is potentially higher: this approach in fact may involve severe intraoperative bleeding and long surgical times, leading to increased postoperative pain, convalescence, and risk of complications (20-24). On the contrary, in case of percutaneous MK, there is not intraoperative bleeding and the mean surgical time is critically reduced.
It is important to inform the reader that there are various devices available, but each of them has its own characteristics and its specific methods of operation (6). The VBS® is a titanium device provided with a hydraulic working system which could be responsible for a partial and not immediate possibility to control the opening of the device, especially in cases of VP (6). On the other hand, OsseoFix® is provided with a mechanical working system which allows a progressive and controlled reduction of the vertebral fracture, but it has an indirect mechanism of action (6). In fact, is the compaction of the trabecular bone that leads to an increase in vertebral body height and not the device itself. In this case there is no direct lift mechanism (6). We chose Spine Jack® because it is provided of a mechanical working system and a direct lift mechanism which allows to obtain great recovery of the vertebral body height (6). Naturally the sample size of the present study is small and it requires additional observations and a longer duration follow-up in order to further corroborate these recommendations.
Conclusions
Based on our experience, we can affirm that the anterior and middle column reconstruction by Spine Jack, represents a valid alternative to the corpectomy and expandible cage replacement in cases of VP, especially in elderly people and for high operative risk patients. In order to perform this technique, the correct indications must be respected: the hyperintense signal in STIR MRI sequences to the level of the fractures must be present. The eventual posterior spinal cord compression must be inferior to 1/3 and 2/3 respectively in case of fractures level above and below the spinal cord without neurological defects. In these cases the MK can be performed alone; otherwise, a direct posterior spinal cord decompression must be done. Furthermore it is mandatory to evaluate the state of the ALL. When it is possible, the percutaneous MK represents an effective surgical treatment as an alternative to corpectomy, equally respectful of the principles of spine biomechanics, but at the same time able to reduce the main operating time and the associated surgical risks. Naturally additional observations and a longer duration follow-up will further corroborate these recommendations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained from the ethics clearance committee of the hospital health administration. All patients were informed about the study procedures and they signed an informed consent form.
References
- Heary RF, Kumar S. Decision-making in burst fractures of the thoracolumbar and lumbar spine. Indian J Orthop 2007;41:268-76. [Crossref] [PubMed]
- Bottai V, Giannotti S, Raffaetà G, et al. Underdiagnosis of osteoporotic vertebral fractures in patients with fragility fractures: retrospective analysis of over 300 patients. Clin Cases Miner Bone Metab 2016;13:119-22. [PubMed]
- Vannucci L, Masi L, Gronchi G, et al. Calcium intake, bone mineral density, and fragility fractures: evidence from an Italian outpatient population. Arch Osteoporos 2017;12:40. [Crossref] [PubMed]
- Vanni D, Pantalone A, Bigossi F, et al. New perspective for third generation percutaneous vertebral augmentation procedures: Preliminary results at 12 months. J Craniovertebr Junction Spine 2012;3:47-51. [Crossref] [PubMed]
- Becker S, Tuschel A, Chavanne A, et al. Balloon kyphoplasty for vertebra plana with or without osteonecrosis. J Orthop Surg (Hong Kong) 2008;16:14-9. [Crossref] [PubMed]
- Vanni D, Galzio R, Kazakova A, et al. Third-generation percutaneous vertebral augmentation systems. J Spine Surg 2016;2:13-20. [Crossref] [PubMed]
- Keshavarzi S, Newman CB, Ciacci JD, et al. Expandable titanium cages for thoracolumbar vertebral body replacement: initial clinical experience and review of the literature. Am J Orthop (Belle Mead NJ) 2011;40:E35-9. [PubMed]
- Röllinghoff M, Siewe J, Zarghooni K, et al. Effectiveness, security and height restoration on fresh compression fractures--a comparative prospective study of vertebroplasty and kyphoplasty. Minim Invasive Neurosurg 2009;52:233-7. [Crossref] [PubMed]
- Berjano P, Lamartina C. Minimally invasive lateral transpsoas approach with advanced neurophysiologic monitoring for lumbar interbody fusion. Eur Spine J 2011;20:1584-6. [Crossref] [PubMed]
- Baghaie M, Gillet P, Dondelinger RF, et al. Vertebra plana: benign or malignant lesion? Pediatr Radiol 1996;26:431-3. [Crossref] [PubMed]
- Harms J. Screw-threaded rod system in spinal fusion surgery. In: Dorman TA. editor. Spine: State of the Art Review. Vol 9. Philadelphia, PA: Hanley & Belfus, 1992:541-75.
- Sasso RC, Renkens K, Hanson D, et al. Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech 2006;19:242-8. [Crossref] [PubMed]
- Oda I, Abumi K, Yu BS, et al. Types of spinal instability that require interbody support in posterior lumbar reconstruction: an in vitro biomechanical investigation. Spine (Phila Pa 1976) 2003;28:1573-80. [Crossref] [PubMed]
- Dunn HK. Anterior stabilization of thoracolumbar injuries. Clin Orthop Relat Res 1984.116-24. [PubMed]
- Shono Y, McAfee PC, Cunningham BW. Experimental study of thoracolumbar burst fractures. A radiographic and biomechanical analysis of anterior and posterior instrumentation systems. Spine (Phila Pa 1976) 1994;19:1711-22. [Crossref] [PubMed]
- Prokop A, König B, Schultheiss M, et al. Kyphoplasty update: What are the limits - what is possible? Unfallchirurg 2011;114:1035-40. [Crossref] [PubMed]
- Luo J, Adams MA, Dolan P. Vertebroplasty and Kyphoplasty Can Restore Normal Spine Mechanics following Osteoporotic Vertebral Fracture. J Osteoporos 2010;2010:729257. [Crossref] [PubMed]
- Krüger A, Oberkircher L, Flossdorf F, et al. Differences in the restoration of vertebral height after treatment of osteoporotic vertebra compression fractures: Cadaver study. Eur Spine J 2012;21:1415-9.
- Noriega DC, Ramajo RH, Lite IS, et al. Safety and clinical performance of kyphoplasty and SpineJack(®) procedures in the treatment of osteoporotic vertebral compression fractures: a pilot, monocentric, investigator-initiated study. Osteoporos Int 2016;27:2047-55. [Crossref] [PubMed]
- Liang B, Huang G, Ding L, et al. Early results of thoraco lumbar burst fracture treatment using selective corpectomy and rectangular cage reconstruction. Indian J Orthop 2017;51:43-8. [Crossref] [PubMed]
- Archavlis E, Papadopoulos N, Ulrich P. Corpectomy in destructive thoracolumbar spine disease: Cost-effectiveness of 3 different techniques and implications for cost reduction of delivered care. Spine (Phila Pa 1976) 2015;40:E433-8. [Crossref] [PubMed]
- Holland CM, Bass DI, Gary MF, et al. Thoracic lateral extracavitary corpectomy for anterior column reconstruction with expandable and static titanium cages: clinical outcomes and surgical considerations in a consecutive case series. Clin Neurol Neurosurg 2015;129:37-43. [Crossref] [PubMed]
- Deukmedjian AR, Manwaring J, Le TV, et al. Corpectomy cage subsidence with rectangular versus round endcaps. J Clin Neurosci 2014;21:1632-6. [Crossref] [PubMed]
- Shousha M, El-Saghir H, Boehm H. Corpectomy of the fifth lumbar vertebra, a challenging procedure. J Spinal Disord Tech 2014;27:347-51. [Crossref] [PubMed]