Effect of body mass index on patient outcomes of surgical intervention for the lumbar spine
Introduction
The United States (US) is in the midst of an obesity epidemic. It is estimated that over one third of adults in the US aged 20 years or older are obese [body mass index (BMI) >30 kg/m2] (1). Secondary medical complications associated with obesity, including metabolic and musculoskeletal problems, can be extensive and significantly limit a person’s ability to function and participate in life (2).
There is a high prevalence of obese patients who elect to have lumbar surgery, despite the potential negative influence obesity may have on surgical outcomes (3-6). Obesity has the potential to affect outcomes of lumbar spine surgery in a number of ways, including intra-operative challenges, health-related problems, and because of the long-term effect of stresses due to excessive body weight. Immediate intra-operative challenges include the need for a larger incision and soft tissue retraction due to excess subcutaneous tissue, which may increase blood loss, operative time, and risk of intra-operative complications. Health-related effects of chronic obesity may increase the incidence of medical complications after surgery, including deep surgical site infection (deep infection), deep vein thrombosis (DVT), all-cause mortality, acute myocardial infarction (MI), pneumonia, pulmonary embolism (PE), and respiratory failure. Over time, excessive body weight can impose undue stress on the surgical implants, adjacent soft tissue, and joints, increasing risk for long-term surgical complications including re-operation and adjacent segment disease (ASD).
Unfortunately, there is conflicting evidence in the current literature about the effect of obesity on outcomes of lumbar spine surgery. This discrepancy may be due to variations in study design, including restriction of the inclusion criteria to a single pre-operative diagnosis (3,7-11), procedure (8,12,13), or by using a single threshold for obesity (30 kg/m2) (9,12-14), thereby limiting the generalizability of study findings across different populations and procedures. Further, no study has examined the effect of obesity on specific surgical-related, health-related, and long-term outcomes within a single patient population over a wide range of diagnoses. The purpose of the current study was to examine the effects of obesity and increasing BMI on surgical-related, health-related, and long-term outcomes of lumbar spine surgery using a community-based Spine Registry from an integrated healthcare system.
Methods
Study design, inclusion & exclusion, and data collection
We conducted a retrospective cohort study (Level III). The study sample included patients over the age of 18 who had an instrumented lumbar spine surgery, including primary lumbar spinal fusion or total disc replacement, within our large integrated US healthcare system between 1/1/2009 and 09/30/2013. Procedures performed due to infection or trauma were excluded. The study cohort consisted of procedures performed by 83 neurosurgeons and 39 ortho-spine surgeons at 15 hospitals across four distinct geographic regions (Hawaii, Northwest, Southern, and Northern California).
Our integrated healthcare system’s Spine Registry was used to identify the study cohort of instrumented lumbar spine patients. Information on the Spine Registry’s coverage, data collection procedures, and quality assurance has been detailed previously (15). Briefly, a set of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) spinal procedure codes were used to capture cases of instrumented spine surgeries through the institution’s electronic medical record (EMR) system. Patient demographics, procedural information, and outcomes were imported from the EMR and trained research associates working for the Spine Registry validated surgical complications via EMR review according to published guidelines. Re-operations for any index procedures were determined by a set of electronic screening algorithms. This study was approved by the Institutional Review Board (IRB) at the integrated healthcare system prior to data collection, and the IRB at San Diego State University, before the data were analyzed.
Exposure of interest
The patients’ BMI was the primary exposure of interest. The EMR was used to extract patient’s height and weight measurements for the one-year pre-operative time interval. These measurements were collected during each medical visit with the healthcare system. For the current study, median height and weight were used to characterize the patient’s BMI. Underweight (BMI <18.5 kg/m2) patients were excluded from the study due to their likelihood of suffering from nutritional deficiency or end stage cancer. BMI was analyzed as a continuous variable in 5 kg/m2 increments, according to the World Health Organization BMI Classification, to examine the association of increasing levels of obesity with each outcome in this study (16).
Outcomes of interest
Surgical-related outcomes included duration of surgery (from incision to close in minutes), estimated blood loss (EBL) (in mL), dural tears (yes, no), epidural hematoma identified within 30 days (yes, no), and improper implant placement treated within 30 days of the index procedure (yes, no). A chart review was conducted for all aseptic re-operations within the first 30 days of the index procedure to determine occurrences of re-operations due to improper implant placement. Health-related outcomes included deep infection within 90 days, DVT within 90 days, all-cause mortality within 90 days, acute MI within 21 days, pneumonia within 21 days, PE within 90 days, and respiratory failure within 7 days. The long-term outcomes included incidence of aseptic re-operation or surgery performed on levels adjacent to the levels treated during the primary lumbar surgery. Aseptic re-operations specifically due to ASD were evaluated as a subset of aseptic re-operations.
Confounding variables
The patient’s age at the time of the primary spinal surgery, gender (female, male), diabetes status (yes, no), smoking status (yes, no), admitting diagnosis (degenerative, spondylolisthesis, deformity, others), surgical approach (posterior, anterior, combined), and number of levels treated (1, 2, 3, 4+) were considered as potential confounders. Admitting diagnosis and the surgical approach were identified using ICD-9 procedural codes and manual chart review of each operative note.
Statistical analysis
Descriptive statistics were calculated for subjects overall and within each BMI category. Means and standard deviations (SD) or medians and interquartile ranges (IQR) were used to describe continuous variables and frequencies and proportions were used to describe categorical variables.
Continuous outcomes (operative time and blood loss) were analyzed using mixed linear models with a random intercept effect for surgeon, as well as a surgeon level covariate representing the mean BMI of patients operated on by each surgeon to address surgeon level confounding (17). Plots were used to check normality of the residuals in an imputed dataset, with no violation detected for any of the outcomes.
Binary outcomes (surgical-related: dural tears, epidural hematoma, improper implant placement; health-related: deep infection, DVT, all-cause mortality, MI, pneumonia, PE, and respiratory failure) were analyzed using conditional logistic regression models to control for surgeon effects. All models addressed the non-independence of observations due to nesting of cases within surgeon, as well as control for the confounding effect of stable surgeon characteristics without assuming equal within and between surgeon effects. BMI was grouped based on quintiles to evaluate the linearity assumption (18). The data were inspected and the linearity assumption was confirmed.
Long-term outcomes for re-operation and re-operation due to ASD were analyzed using survival analysis with a surgeon stratified Cox regression model. Either re-operation for infection or non-union, death, or termination of healthcare membership before the end of the study period constituted a censored event. Re-operations due to infection or non-union were censored at the time of re-operation because of the impact of confounding health-related factors. Proportional hazards for BMI and age were assessed based on the significance tests of simulated data (19), and there was no evidence of violation (P>0.05) in an imputed dataset. Hazard ratios (HR) were calculated to estimate relative risk of long-term outcomes.
Patient age, gender, diabetes status, smoking status, admitting diagnosis, and surgical approach were included as covariates in multivariable regression models. Number of levels treated was not significantly different among BMI categories (Chi Square P>0.05). To address missing values for admitting diagnosis, surgical approach, length of operation, and EBL, multiple imputations were performed. Each dataset was analyzed separately using the same model, and later combined to calculate the final parameter estimates (20). Data were analyzed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Threshold for statistical significance was alpha =0.05.
Results
During the study period, 8,049 patients underwent instrumented lumbar spine surgery; 1,890 (23.5%) patients had a BMI <25, 3,122 (38.8%) had a BMI of 25–30, 1,983 (24.6%) had a BMI of 30–35, 786 (9.8%) had a BMI of 35–40, and 268 (3.3%) had a BMI of 40+. 222 (2.8%) patients died during follow-up and 663 (8.2%) terminated membership. The median follow-up time was 2.0 years (IQR: 0.9–3.3). For the overall study cohort, the median BMI was 28.3 (IQR: 25.1–32.1) and median age was 63.0 (IQR: 53.0–71.0) (Table 1). Most patients in the overall cohort were female, non-diabetic, non-smoking, admitted due to degenerative disease, and underwent a posterior fusion (Table 1).
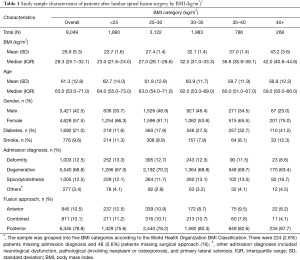
Full table
Median operation time was lowest for the BMI <25 group (218 minutes, IQR: 168–286) and highest for the BMI 40+ group (234 minutes, IQR: 182–303) (Table 2). Similarly, median EBL was lowest for both the BMI <25 and BMI 25–30 groups at 300 mL (IQR: 150–500 and 150–600, respectively) and highest for the BMI 40+ group (400 mL, IQR: 200–600) (Table 2). After adjusting for confounders, each 5 kg/m2 increase in BMI was associated with 7.8 minute increase in the duration of the surgery (95% CI: 6.0–9.5, P<0.01) and 36.0 mL increase in the EBL during surgery (95% CI: 25.5–46.5, P<0.01).
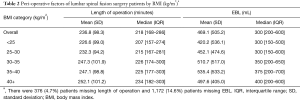
Full table
Incidence of surgical complications ranged across BMI groups from 4.0–5.2% for dural tears, 1.0–1.3% for epidural hematomas, and 0.4–1.1% for improper implant placement (Table 3). Incidence of health-related complications ranged from 0.4–3.0% for deep infection, 0.3–0.8% for DVT, 0.0–1.1% for all-cause mortality, 0.3–0.4% for MI, 0.8–1.2% for pneumonia, 0.4–1.1% for PE, and 0.0–0.5% for respiratory failure (Table 3). After adjusting for confounders, BMI was not significantly associated with dural tears, epidural hematomas, improper implant replacement, all-cause mortality, MI, pneumonia, PE, or respiratory failure (Table 4). However, every 5 kg/m2 increase in BMI was associated with 1.7 greater odds of deep infection within 90 days (95% CI: 1.4–2.1, P<0.001) and 1.5 greater odds of DVT within 90 days (95% CI: 1.1–1.9, P<0.05) (Table 4).
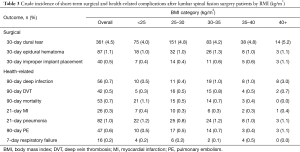
Full table
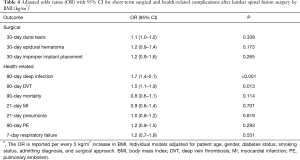
Full table
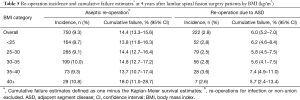
There were 750 (9.3%) lifetime aseptic re-operations performed after the index procedure (Table 5). The BMI 40+ group had the highest cumulative failure at 4 years (18.0%, 95% CI: 11.0–28.7), while cumulative failures for the other BMI categories ranged from 13.7–14.8% (Table 5). After adjustment for covariates, the overall risk of re-operation was 1.1 times higher (95% CI: 1.0–1.2, P=0.03) for every 5 kg/m2 increase in BMI. Risk of re-operation due to ASD was not associated with BMI (HR: 1.1, 95% CI: 1.0–1.2, P=0.18).
Full table
Discussion
Healthcare is evolving to focus more on optimizing patient outcomes, quality of care, and costs of care. Using data from a community-based Spine Registry, which includes a variety of diagnoses, increasing BMI was associated with a statistically significant increase in operative time, EBL, deep infection, DVT, and higher re-operation rates. However, there was no association between increasing BMI and dural tears, epidural hematomas, improper implant placement, all-cause mortality, MI, pneumonia, PE, respiratory failure, or with risk of re-operation due to ASD. Based on our findings, when holding all other covariates constant, compared to healthy weight patients (BMI <25 kg/m2), obese patients with a BMI >40 kg/m2 would require approximately 31 additional minutes of operating time, experience 144 mL more EBL during surgery, and have a 46% higher risk of aseptic re-operation. In addition, for patients with a BMI >40 kg/m2, the odds for deep infection are 279% higher and the odds for DVT are 179% higher than the odds for patients with a BMI <25 kg/m2. These patients who are more severely obese, may bear the burden of increased medical costs and poor patient-centered outcomes associated with the adverse outcomes of instrumented lumbar spine surgery.
Our findings are in agreement with some prior studies examining the effect of obesity on certain surgical and health-related outcomes in selected patient populations. De La Garza-Ramos et al. reported that in patients undergoing posterolateral fusion surgery, obesity was associated with increased blood loss but there was no difference in rates of epidural hematomas (13). Similarly, McGuire et al. reported a relationship between obesity, classified as a BMI of ≥35, and increased operative time and blood loss, but not with intraoperative complications for a sample of patients with spondylolisthesis (14). Peng et al. reported longer operative times, but no differences in blood loss or intra-complications in patients with and without obesity (12). However, this study focused on anterior lumbar disc procedures specifically. Based on the current study, which includes a variety of diagnoses and considers increasing severity of obesity, and the prior literature, increasing BMI appears to be consistently associated with increased EBL and operative time, but not intraoperative complications.
Our findings agree with most prior literature on the effect of obesity on risk of deep infection and DVT after lumbar spine surgery. In the current study, risk of deep infection and DVT at 90 days was significantly increased with increasing levels of obesity. Most prior investigators also have reported that obesity increases risk of deep surgical site infection in a variety of patient samples (13,14,21). However, in obese patients treated for degenerative scoliosis, Fu et al. showed no increase in superficial or deep infection (10). Previous investigators also consistently report that obese patients are at greater risk for DVT (4,13). In the current study, no association was found between obesity and other surgical and health-related complications including: dural tears, epidural hematomas, improper implant replacement, all-cause mortality, MI, pneumonia, PE, and respiratory failure. While investigators consistently report no increase in risk of mortality, some have reported an increased risk of the other health-related complications for obese patients (4,6,13,14,22). Therefore, based on the current study and the previous literature, it appears that obesity consistently increases risk of deep wound infection and DVT, but may also increase risk of other health-related complications in some patient populations.
Our findings related to long-term risk of re-operation and re-operation due to ASD conflict with current literature. Radcliff et al. reported no effect of BMI on re-operation rates in patients treated with a posterior decompression or fusion for spinal stenosis (7). This study was limited to only patients with lumbar stenosis, and did not include patients with spondylolysis or spondylolisthesis. Further, a large majority of patients from the study received treatment through decompression only with no fusion (85–89%).Fu et al. reported no difference in ASD or revision surgeries in obese and non-obese patients treated with lumbar fusion (10). However, investigators only divided patients into normal, overweight, and obese categories, with no stratification of obesity severity. Min et al. also reported no difference in BMI between patients with and without ASD treated with instrumented lumbar fusion (23), but this study included a relatively small population, with only two patients undergoing re-operation for ASD. Findings from the current study are in agreement with Seicean et al., who reported an increased risk of 30-day re-operations in National Surgical Quality Improvement Project (NSQIP) patients with Class II obesity and treated with elective laminectomy or fusion (22). Reporting on longer follow-up for re-operations and ASD was unavailable as the NSQIP database only tracks the first 30 days post-operatively. Based on the current study and the prior literature, evidence most consistently suggests that, for a broad range of diagnoses, increasing levels of BMI are associated with an overall increased risk of re-operation, but not an increase in risk of re-operations due to ASD after lumbar spine surgery.
There are several limitations to the current observational study. First, our study was retrospective in nature. However, the data utilized was prospectively collected into a Spine Registry, in a standardized manner to ensure validity of the information collected. In addition, the data was derived from actual clinical data and can therefore be generalized to a clinical population. Second, median follow-up time for the study sample was 2 years (IQR: 0.9–3.3), thus some patients had less than 2 years of follow-up. This reduced follow-up time may have led to an underestimate of ASD as this outcome is often chronic in nature. Third, there were fewer subjects in the higher BMI categories, which may influence generalizability of the findings for these groups. Fourth, although some investigators have reported that obesity has a negative impact on functional outcomes (3,5), we were not able to confirm their findings in the current study as functional and patient-centered outcomes are not routinely being captured by the Spine Registry. Other limitations of the study include that a majority of the procedures were performed through a posterior approach, and the data includes outcomes from but does not differentiate between minimally invasive and open procedures. Last, only all-cause mortality was captured in the registry, therefore we can not differentiate the extent to which mortality was directly related to the surgery or other comorbid conditions. However, increasing levels of obesity were not associated with all-cause mortality.
Study strengths include use of a community-based Spine Registry with validated outcomes and no dependence on industry support for clinical research. Prior studies have utilized Medicare, NSQIP, and insurance databases. These data sources are limited to specific patients, narrow outcome definitions, and a shorter duration of patient follow-up. The cohort from the current registry study represents a diverse population of patients who elected instrumented lumbar spine surgery and represent multiple geographic regions, includes surgeons from orthopedic and neurosurgical specialties, and represents real world data, enhancing generalizability. To our knowledge, this is the first study to use data from a single large cohort of patients, with a broad range of diagnoses, to evaluate the impact of increasing levels of BMI on the many different outcomes of lumbar spine surgery, including: surgical-related, health-related, and long-term outcomes.
Obesity presents a complex challenge in spine surgery. In this study of 8,049 patients with instrumented lumbar spine surgery, increasing obesity and BMI was associated with a statistically significant increase in the length of surgery, EBL, deep infection, DVT, and rate of re-operation. This information is of value when discussing surgical risk with obese patients who elect to undergo instrumented lumbar spine surgery. These findings are also of value in peri-operative management for these patients, including medical optimization prior to surgery, utilization of alternative surgical approaches and techniques, and comprehensive post-operative management. Future study is needed to determine the impact of obesity and increasing BMI on patient-centered outcomes and costs of care.
Acknowledgements
We acknowledge all the Kaiser Permanente spine surgeons who contribute to the success of the Spine Registry, as well as the Surgical Outcomes and Analysis department, which coordinates registry operations.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board (IRB) at the integrated healthcare system prior to data collection, and the IRB at San Diego State University before the data were analyzed (Approval ID number: #10418).
References
- Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States 2011-2012. JAMA 2014;311:806-14. [Crossref]
- Heuch I, Hagen K, Heuch I, et al. The impact of body mass index on the prevalence of low back pain: the HUNT study. Spine (Phila Pa 1976) 2010;35:764-8. [Crossref]
- Knutsson B, Michaëlsson K, Sandén B. Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patients from the Swedish spine register. Spine (Phila Pa 1976) 2013;38:435-41. [Crossref]
- Marquez-Lara A, Nandyala SV, Sankaranarayanan S, et al. Body mass index as a predictor of complications and mortality after lumbar spine surgery. Spine (Phila Pa 1976) 2014;39:798-804. [Crossref]
- Gum JL, Carreon LY, Stimac JD, et al. Predictors of Oswestry Disability Index worsening after lumbar fusion. Orthopedics 2013;36:e478-83. [Crossref]
- Buerba RA, Fu MC, Gruskay JA, et al. Obese class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J 2014;14:2008-18. [Crossref]
- Radcliff K, Curry P, Hilibrand A, et al. Risk for adjacent segment and same segment reoperation after surgery for lumbar stenosis: a subgroup analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 2013;38:531-9. [Crossref]
- Lau D, Ziewacz J, Park P. Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis in patients with significant obesity. J Clin Neurosci 2013;20:80-3. [Crossref]
- Rihn JA, Kurd M, Hilibrand AS, et al. The influence of obesity on the outcome of treatment of lumbar disc herniation: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am 2013;95:1-8. [Crossref]
- Fu L, Chang MS, Crandall DG, et al. Does obesity affect surgical outcomes in degenerative scoliosis? Spine (Phila Pa 1976) 2014;39:2049-55. [Crossref]
- Sato S, Yagi M, Machida M, et al. Reoperation rate and risk factors of elective spinal surgery for degenerative spondylolisthesis: minimum 5-year follow-up. Spine J 2015;15:1536-44. [Crossref]
- Peng CW, Bendo JA, Goldstein JA, et al. Perioperative outcomes of anterior lumbar surgery in obese versus non-obese patients. Spine J 2009;9:715-20. [Crossref]
- De la Garza-Ramos R, Bydon M, Abt N, et al. The impact of obesity on short- and long-term outcomes following lumbar fusion. Spine (Phila Pa 1976) 2014. [Epub ahead of print].
- McGuire KJ, Khaleel MA, Rihn JA, et al. The effect of high obesity on outcomes of treatment for lumbar spinal conditions: subgroup analysis of the spine patient outcomes research trial. Spine (Phila Pa 1976) 2014;39:1975-80. [Crossref]
- Paxton EW, Kiley ML, Love R, et al. Kaiser Permanente implant registries benefit patient safety, quality improvement, cost-effectiveness. Jt Comm J Qual Patient Saf 2013;39:246-52. [Crossref]
- The World Health Organization. Obesity and overweight fact sheet. 2015. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/
- Neuhaus JM, Kalbfleisch JD. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 1998;54:638-45. [Crossref]
- Hosmer DW, Lemeshow S, Sturdivant RX. Model-Building Strategies and Methods for Logistic Regression. Available online: https://mybiostats.files.wordpress.com/2015/03/model_building_strategies_and_methods_for_logistic_regression.pdf
- Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika 1993;80:557-72. [Crossref]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons, 1987. Available online: http://onlinelibrary.wiley.com/doi/10.1002/9780470316696.fmatter/pdf
- Lim S, Edelstein AI, Patel AA, et al. Risk factors for postoperative infections following single level lumbar fusion surgery. Spine (Phila Pa 1976) 2014. [Epub ahead of print]. [Crossref]
- Seicean A, Alan N, Seicean S, et al. Impact of increased body mass index on outcomes of elective spinal surgery. Spine (Phila Pa 1976) 2014;39:1520-30. [Crossref]
- Min JH, Jang JS, Jung B, et al. The clinical characteristics and risk factors for the adjacent segment degeneration in instrumented lumbar fusion. J Spinal Disord Tech 2008;21:305-9. [Crossref]


