Hypoglossal nerve paresis secondary to anterior approach of upper cervical spine followed by spontaneous recovery
Introduction
Complications of anterior cervical spine approach are typically related to vascular structures and aerodigestive tract (1,2). The aim of our work is to report a less common complication that may happen in the anterior approach to upper segments of the cervical spine.
Case presentation
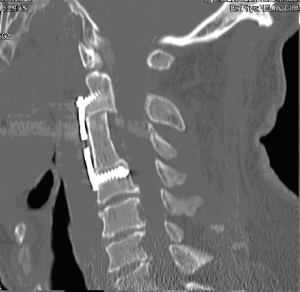
A 63-year-old male with no relevant past medical history was transferred to the emergency room after suffering an impact of a beam to the top of his head while working. The patient suffered with intense neck pain. Physical examination showed no neurological problems. Cervical spine CT showed a C3 vertebral body fracture with several fragments, associated with a fracture to the vertebral lamina (Figure 1). There was no invasion to the spinal canal. The CT head scan showed no traumatic injuries.
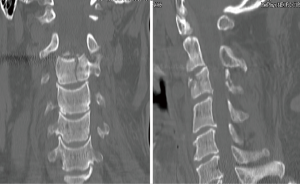
Surgery for cervical spine stabilization was performed. Intervention consisted of a right side anterior approach to the upper cervical spine. In this procedure, after platysma muscle dissection, retraction of the upper digastric and the submandibular gland was necessary. Finally, C3 corpectomy and placement of an iliac crest autograft with plate and screws was carried out. There were no intraoperative incidences. Postoperative cervical spine CT showed adequate resection of vertebral body with appropriate placement of graft, plate and screws (Figure 2). However, the patient presented dysarthria and dysphagia, accompanied by subjective uncoordinated tongue movement in the immediate postoperative period. Physical examination revealed a moderate limitation in mobility of the tongue to the right side without other accompanying neurological defects (Figure 3). Ten days after surgery he began to experience partial disappearance of his symptoms. During the outpatient follow-up he experienced progressive improvement with complete resolution of symptoms.
Discussion
Hypoglossal nerve injury is a common complication in surgery of anterior cervical region soft tissue. It has been frequently described in the approach of cervical carotid artery (3). However, its incidence in the approach to the cervical spine has been scarcely reported (4,5).
Hypoglossal nerve and cranially facial and glossopharyngeal nerves may be found in the dissection of the anterior cervical triangle of the neck. Injury of these nerves is not uncommon in surgical procedures in which soft tissue dissection of this region is necessary (resection of gill cysts, carotid body tumors, etc.) (4).
Blunt dissection through soft tissue is usually performed to approach the upper cervical spine in order to avoid the possibility of relevant structures injury. Nevertheless, interruption of venous vessels located in the surgical pathway may be necessary. In a retropharyngeal approach to the upper cervical spine, the hypoglossal nerve may mimic a venous vessel, so great caution is mandatory when interrupting venous-like structures in this location (6).
This case describes a hypoglossal neuropraxia probably related to the soft tissue traction generated by the upper part of the self-retaining retractor.
Dysphagia and dysarthria are usually the most frequent symptoms of hypoglossal nerve injury. Both symptoms appear frequently in the postoperative period after cervical spine surgery performed through the anterior approach, so the diagnosis of hypoglossal nerve paresis in these cases can be challenging. Dysarthria may be confused with dysphonia, secondary to recurrent laryngeal nerve retraction while dysphagia is often related to oesophagus retraction. Thus, hypoglossal palsy is not be noticed unless an evident tongue deviation occurs (4).
To the best of our knowledge, there are only two previously reported cases of hypoglossal injury after an anterior approach to the upper cervical spine (4,5). In one of these cases the patient suffered permanent hypoglossal palsy (4) and in the other, symptoms improved after 3 weeks (5). In our experience, the patient experienced spontaneous improvement of hypoglossal paresis 10 days after the onset of symptoms, with the subsequent disappearance of dysphagia and dysarthria completely.
Conclusions
In the approach to the upper cervical spine, hypoglossal nerve injury may be caused by soft tissue retraction performed during vertebral body exposure. In our experience, unlike the cases previously described in the literature, the patient had complete improvement of paresis with total disappearance of symptoms.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Edwards CC 2nd, Karpitskaya Y, Cha C, et al. Accurate identification of adverse outcomes after cervical spine surgery. J Bone Joint Surg Am 2004;86-A:251-6. [Crossref] [PubMed]
- Zeidman SM, Ducker TB, Raycroft J. Trends and complications in cervical spine surgery: 1989-1993. J Spinal Disord 1997;10:523-6. [Crossref] [PubMed]
- Weiss K, Kramár R, Firt P. Cranial and cervical nerve injuries: local complications of carotid artery surgery. J Cardiovasc Surg (Torino) 1987;28:171-5. [PubMed]
- Sengupta DK, Grevitt MP, Mehdian SM. Hypoglossal nerve injury as a complication of anterior surgery to the upper cervical spine. Eur Spine J 1999;8:78-80. [Crossref] [PubMed]
- Yasuda T, Togawa D, Hasegawa T, et al. Hypoglossal nerve palsy as a complication of an anterior approach for cervical spine surgery. Asian Spine J 2015;9:295-8. [Crossref] [PubMed]
- Emery SE, Bolesta MJ. Complications of cervical spine surgery. In: Bridwell KW, DeWald RL. editors. The textbook of spinal surgery, 2nd edition. Philadelphia: Lippincott-Raven, 1997:1427-38.