Feasibility of endoscopic discectomy by inter laminar approach at a high volume tertiary public hospital in a developing country
Introduction
Lumbar disc herniation is a common condition. It occurs in 5.1% men & 3.7% women (1). It can be disabling condition. After failure of conservative treatment; surgery is the next line of management. It consists of discectomy performed either open or by minimally invasive techniques. Endoscopic discectomy was first introduced by Foley and Smith which had a tubular retraction system (2). It is being used increasingly nowadays .They offer the advantage of minimal tissue damage, direct visualisation of surgical field & usual familiarity to the surgeon (3). The aim of our study is twofold. First, to check its feasibility at a tertiary public sector hospital and second to know the learning curve.
Methods
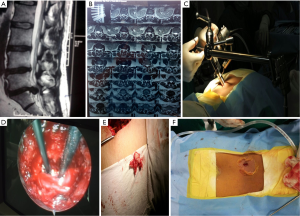
It is a prospective study of 80 patients with single level lumbar disc herniation who were treated with endoscopic lumbar discectomy using tubular retractors .Inclusions were patients who failed conservative treatment consisting of 6 weeks of structured physical therapy, NSAIDS for pain and epidural steroids as needed. Exclusions were patients having instability or previous spine surgery. All patients had pre-op standing AP, lateral, bending X-rays; T1 AND T2 weighted sagittal and axial MRI from 1.5T Siemens machine to detect instability and level of compression. All patients were operated by a single senior surgeon having experience of 15 years.
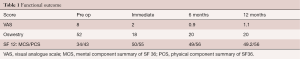
Duration of surgery, blood loss, and day of mobilization, complications and duration of hospitalisation were noted. Functional outcome was assessed pre op & post op (immediate, 6 months, 12 months) using VAS score, Oswestry Disability Index, SF 12 Score and modified MacNab criteria for which p values were calculated.
Operative procedure
The patient was positioned in prone position with bolsters below the chest and on the iliac crest keeping the abdomen free, head end raised and pressure points well padded. The surgeon stands on the side of the herniation. Using lateral fluoroscopy imaging on ipsilateral side, a 20 G spinal needle was inserted at the level of the involved disc space. The needle was inserted one index finger width lateral to the midline. The needle should be either targeted superiorly, at the disc level or inferiorly, depending upon the anatomy of the herniation or sequestration. A 16–18 mm incision was then made centered over the needle and was deepened till the fascia. The incision was 18 mm if a 16 mm-diameter tube was used. The target site was the inferior lamina of the superior vertebrae that was the junction of lamina and medial facet. The incision is made around 1–1.5 cm around one finger breath from spinous process. The incision is made slightly more laterally for central disc or in case when opposite side decompression is required so that the tube can be angled for approaching the central aspect and opposite side. The initial dilator was then inserted .The initial dilator was used to sweep off the paraspinal muscle mass and palpate the bony landmarks. Sequential dilators were then inserted. The marking on the final dilator at the level of skin provides the depth of the tubular retractor. If the marking is between 4 and 5 then a number 5 tubular retractor should be used. The final tubular retractor, which was 18 or 16 mm in diameter, was then docked with the flexible arm as the final working channel. The 18 mm tube was most commonly used in this series. The 16 mm tube was utilized in cases where the disc herniation was small and restricted to the disc space without any migration. Then, laminectomy was done, till the junction of the inner cortex and ligamentum flavum was encountered. A cleft was created in the ligamentum flavum with a no. 4 Penfield dissector. The flavum was then excised medially and laterally using a no. 2 Kerrison Rongeur to get a good visualization of the dural sac and nerve root.
It was important to determine preoperatively on the MRI, whether the location of the disc was in the axilla or the shoulder of the nerve root. An inferiorly migrated disc was generally in the axilla of the nerve root. In case of a shoulder disc the nerve root once identified, can be retracted medially using a nerve root retractor. The disc was then identified. The bulge in a contained disc can be well appreciated on the LED screen connected. Then, an annulotomy was done with a no. 15 blade on a bayonet handle in cruciate manner or the annular tear if present can be probed with a nerve hook. The disc was then probed using a nerve hook and the herniated fragment was delivered out of the annulus. The fragment was then removed with a disc forceps. Multiple attempts were made to seek hidden disc fragments with a nerve hook till adequate nerve root decompression was performed. A pulsatile central dural sac and nerve root that was mobile was considered an adequate decompression surgery (Figure 1). The epidural bleeding was controlled using a combination of bipolar cautery, bone wax and Gelfoam. The thoracolumbar fascia and subcutaneous tissue were closed using 2-0 Vicryl. The skin was closed using3-0 Monocryl. A single dose of intravenous antibiotic was given on the same night as a standard protocol.
Postoperatively, all patients were mobilized as soon as the pain subsides and were discharged 48 hours post-surgery. The patients were allowed to go back to work after 3 weeks. A gradual back-strengthening program was started after 6 weeks.
Results
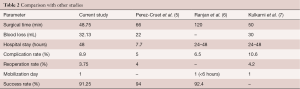
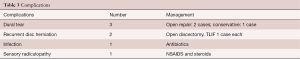
The mean age of our patients was 34.9 years (range, 17 to 72 years) and male to female ratio was 2.6:1. All patients were followed for a minimum of 12 months. All had herniation of a single lumbar disc (chart 1). Ten percent (n=8) patients had neurological involvement pre-op while the remaining had normal neurology. Five percent (n=4) patients had taken epidural steroids earlier. Patients were discharged 48 hours after surgery as per department protocol to undergo physical therapy. On an average blood loss was 32.13 mL and the duration of surgery was 48.75 min. Complication rate was 8.9% with 3.75% reoperation rate. There were three cases of dural tear, one infection, two recurrences and one case of severe sensory radiculopathy in the post-operative period.
The mean VAS score improved from 8 to 1.1, Oswestry Disability Index from 52 to 20 and SF 12 scores (MCS/PCS) from 34/43 to 49.2/56 with P value significant (P<0.05) using the t-test for biostatical analysis. These improvements were either maintained or deteriorated slightly at final follow up (Table 1). As per modified MacNab Criteria 77.5% were excellent, 13.75% good, 7.5% fair and 1.25% poor. Success rate was 91.25% by including the excellent and good categories.
Full table
Discussion
Mixter and Barr reported the first discectomy in 1934 (4). Since then various techniques have come about to achieve this. Discectomy using tubular retractors are in vogue now since the last decade. This study was conducted in a tertiary public sector hospital with high patient load (more than 50 spine surgeries a month) where treatment is provided free of cost and catering to mostly the economically backward classes of the society. Therefore introduction of a new technique should have a favourable learning curve and be feasible and cost effective to the public system.
Our study performed in this regard shows results that are at par with various national and international studies (Table 2). Our average surgical time was 48.75 minutes, however baring the initial five cases which could be considered as learning curve the average time was 35 minutes. We did not use an operating microscope. This decreased our cost of treatment and learning curve of hand-eye coordination. We had three dural tears, two occurred in the initial five cases which required conversion to open surgery and primary dural repair after a laminectomy at the involved level. Third was a small rent which occurred in the 54th case and did not require conversion to open surgery. There was a single case of infection which was treated with empirical antibiotics as advised by infectious disease specialist. There were two cases of recurrence on the same side, both occurred within a period of 6 months of follow up. One was managed with decompression with interbody fusion PLIF and the other by open discectomy. One of our patients had severe post-operative sensory radiculopathy but resolved with conservative care (Table 3).
Full table
Full table
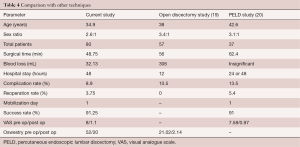
For the treatment of single level lumbar disc herniations, it was found that results with regards to blood loss, duration of hospital stay, systemic effects were better for microsurgical and endoscopic techniques when compared to open technique (8). Endoscopic discectomy gives smaller incision, less local trauma and faster recovery than open discectomy (9-12). Its results are similar to microscopic discectomy (13). But it can address opposite side pathology as well (14). Percutaneous endoscopic lumbar discectomy (PELD), the latest armour in the field of ever developing minimal invasive spine surgery, boasts the advantages of even a smaller incision and can be performed under local anaesthesia (15). The outcomes however remain similar even the short term when compared with one of the studies (16). Though PELD has many advantages, certain potential pitfalls remain making it a difficult technique to acclimatise and master in such a high volume setup with economical constraints. Some drawbacks include difficulty in L5–S1 (17), high riding iliac crest with a L4–5 pathology (these form the bulk of patients in our case), central disc, calcified disc (6), apprehensive patients, difficulty to assess opposite side and long learning curve (15). Many surgeons are convinced of advantages of the system and have included this system as part of their inventory. However, due to difficulty in orientation with scope and two-dimensional vision, availability of less space, frustrating and steep learning curve, and inability to master hand eye coordination, majority of surgeons are not able to continue with the technique. The patience and perseverance to work through narrow confines and work closely with a surgeon who has mastered the technique is the key to learn (18). Learning curve for our series was five cases considering the fact that the complication rate was 3/5 in them and also a longer time interval (Table 4). Rate of complications seems similar in both open and endoscopic techniques; however results reported are extremely nonhomogeneous in different series (21).
Full table
Conclusions
Endoscopic discectomy using the tubular retractor system and the inter-laminar approach is a great advancement in the field of spine surgery and is able to demonstrate outcomes equivalent to all other time tested and newer techniques. This method can become the gold standard especially in a high volume tertiary public sector to cater a large volume of patient and provide as near to a state of art treatment to these patient, also its use in multi-faceted patient profiles makes it best suited in this regard.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical clearance of the concerned board for performing this research was taken along with written and informed consent of all the patients participating in the study.
References
- Heliövaara M, Impivaara O, Sievers K, et al. Lumbar disc syndrome in Finland. J Epidemiol Community Health 1987;41:251-8. [Crossref] [PubMed]
- Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg 1997;3:301-7.
- Kim YB, Hyun SJ. Clinical applications of the tubular retractor on spinal disorders. J Korean Neurosurg Soc 2007;42:245-50. [Crossref] [PubMed]
- Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal cord. N Engl J Med 1934;211:210-4. [Crossref]
- Perez-Cruet MJ, Foley KT, Isaacs RE, et al. Microendoscopic lumbar discectomy: technical note. Neurosurgery 2002;51:S129-36. [Crossref] [PubMed]
- Ranjan A, Lath R. Microendoscopic discectomy for prolapsed lumbar intervertebral disc. Neurol India 2006;54:190-4. [PubMed]
- Kulkarni AG, Bassi A, Dhruv A. Microendoscopic lumbar discectomy: Technique and results of 188 cases. Indian J Orthop 2014;48:81-7. [Crossref] [PubMed]
- Gotfryd A, Avanzi O. A systematic review of randomised clinical trials using posterior discectomy to treat lumbar disc herniations. Int Orthop 2009;33:11-7. [Crossref] [PubMed]
- Li SH, Li HZ, Zhao JR. Clinical comparison between micro-endoscopic discectomy (MED) and open discectomy for treatment of lumbar disc herniation. Zhongguo Gu Shang 2008;21:349-51. [PubMed]
- Ruetten S. Full-endoscopic Operations of the Spine in Disk Herniations and Spinal Stenosis. Surg Technol Int 2011;21:284-98. [PubMed]
- Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 2007;61:545-9; discussion 549. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine 2007;6:521-30. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931-9. [Crossref] [PubMed]
- Wada K, Sairyo K, Sakai T, et al. Minimally invasive endoscopic bilateral decompression with a unilateral approach (endo-BiDUA) for elderly patients with lumbar spinal canal stenosis. Minim Invasive Neurosurg 2010;53:65-8. [Crossref] [PubMed]
- Ahn SS, Kim SH, Kim DW. Learning Curve of Percutaneous Endoscopic Lumbar Discectomy Based on the Period (Early vs. Late) and Technique (in-and-out vs. in-and-out-and-in): A Retrospective Comparative Study. J Korean Neurosurg Soc 2015;58:539-46. [Crossref] [PubMed]
- Yoon SM, Ahn SS, Kim KH, et al. Comparative Study of the Outcomes of Percutaneous Endoscopic Lumbar Discectomy and Microscopic Lumbar Discectomy Using the Tubular Retractor System Based on the VAS, ODI, and SF-36. Korean J Spine 2012;9:215-22. [Crossref] [PubMed]
- Choi G, Lee SH, Raiturker PP, et al. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery 2006;58:ONS59-68; discussion ONS59-68.
- Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong) 2011;19:30-4. [Crossref] [PubMed]
- Hirano Y, Mizuno J, Takeda M, et al. Percutaneous endoscopic lumbar discectomy - early clinical experience. Neurol Med Chir (Tokyo) 2012;52:625-30. [Crossref] [PubMed]
- Kaushal M, Sen R. Posterior endoscopic discectomy: Results in 300 patients. Indian J Orthop 2012;46:81-5. [Crossref] [PubMed]
- Anichini G, Landi A, Caporlingua F, et al. Lumbar Endoscopic Microdiscectomy: Where Are We Now? An Updated Literature Review Focused on Clinical Outcome, Complications, and Rate of Recurrence. Biomed Res Int 2015;2015:417801.
Contributions:(I) Conception and design: SM Soman; (II) Administrative support: JV Modi; (III) Provision of study materials or patients: JV Modi; (IV) Collection and assembly of data: J Chokshi; (V) Data analysis and interpretation: SM Soman; (VI) Manuscript writing: All authors; (VII): Final approval of manuscript: All authors.


