Traumatic dislocation of the S1 polyaxial pedicle screw head: a case report
Introduction
Implant failure is not an uncommon complication following instrumented surgeries of the spine. However, polyaxial screw head dislocation in the absence of a manufacture defect is extremely rare and represents a biomechanical overload of the screw, leading to early failure.
Posterior pedicle screw fixation constructs revolutionized the way instrumented spine surgeries are performed in the 1990s with many biomechanical and clinical studies showing its superiority over other existing constructs. Its strength in fixation stems from its ability to span 3 columns of the spine making them great tools in the correction of major spinal deformities. However, this results in a sudden transition of rigidity between the instrumented and non-instrumented spine, with increased stress also receding in this construct. Failure thus occurs either in the form of adjacent segment disease, loosening of the screw-bone interface or breakage of the implants.
In this study, we report a rare early complication of implant failure following posterior instrumented interbody fusion of the lumbar spine at L5/S1 level.
Case presentation
A 58-year-old gentleman presented with a 6 year history of lower back pain which was worse over the past 6 months. This was associated with radicular pain to the right buttock, posterior thigh, lateral leg and dorsum of the foot. The patient also complained of paresthesia over the same distribution. The pain was aggravated on bending backwards and he was unable to walk for more than 15 minutes due to his symptoms. He did not have any urinary or bowel complaints.
On examination, there was paravertebral spinal muscle spasms found and a midline bony step was palpable over the lower back. His lumbar excursion was limited to 4 cm. Neurological examination showed preserved power in both lower limbs with hyporeflexia noted over the right ankle jerk. Sensation was also normal in both lower limbs and the patient walked with a normal gait.
X-rays performed using EOS technology (Biospace Med, Paris, France) revealed a Meyerding grade 2 isthmic spondylolisthesis of L5/S1 associated with lumbosacral kyphosis and a balanced global spinal alignment. Slip angle was 20.1 degrees and dynamic X-rays showed movement at L5/S1 associated with a vacuum sign at the interbody space (Figure 1). Following treatment with back care advice, analgesics and physiotherapy for 3 months, his symptoms did not improve and he was planned for surgical treatment.
Computed Tomography (CT) confirmed the lysis defects at both pars interarticularis associated with asymmetrical olisthesis with the right side having a greater degree of slippage. This resulted in axial rotation of the vertebral. Prominent anterior and posterior syndesmophytes was also noticed on the CT images (Figure 2A). Magnetic resonance imaging (MRI) scan was also performed as part of the pre-operative workup which showed mild central canal stenosis secondary to spondylolisthesis with severe bilateral foraminal stenosis resulting in compression of exiting L5 nerve roots (Figure 2B,C).
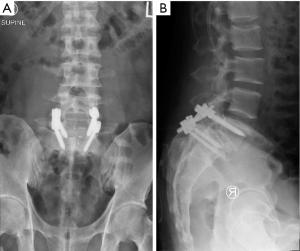
The patient underwent the index surgery comprising of open bilateral decompression laminectomy, complete bilateral facetectomies, transforaminal lumbar interbody fusion using polyaxial pedicle screw (7.5 mm)-titanium rod (5.5 mm) construct with size 12 mm Polyetheretherketone (PEEK) cage and attempted reduction of the spondylolisthesis at the L5/S1 level. As the deformity remains stiff despite posterior release, decision was made intra-operatively to accept partial reduction of the sagittal deformity. Electromyographic signals were normal throughout the surgery. His immediate post-operative recovery was uneventful and he was discharged on the 4th post-operation day. X-rays taken was shown in Figure 3.
Ten days after his index surgery, the patient attempted to bend forward to pick an item off the floor and felt a give in the back which was accompanied by immediate lower back pain. This was associated with a recurrence of right lower limb pain and numbness in the same distribution as his pre-operative symptoms.
Repeat X-rays revealed a dislocation of the right S1 polyaxial screw head from the screw shank and a loss of reduction of his spondylolisthesis (Figure 4). The contralateral implants were otherwise unremarkable. CT scan confirmed these X-ray findings. In addition, no bony fracture or loosening of implants were noted (Figure 5).
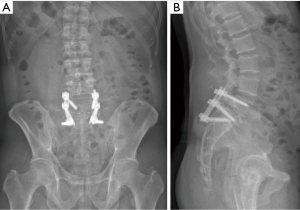
In view of these findings, revision surgery was planned for the patient. During the surgery, the damaged right S1 screw (Figure 6) was removed and replaced by a larger size screw. The left S1 screw was also exchanged for a larger size screw as it was in the opinion that this screw might also be loose due to concentrated stress following failure on the right side. Indeed, the torque to remove the left screw was found to be lower although there was no frank loosening. Both L5 screws were inspected and retained. New S2-alar screws were placed under fluoroscopic guidance to increase the distal purchase at the sacrum in view of the likely high force required to fully reduce this deformity. The interbody cage was then removed. Annular release was performed using a cobb elevator bilaterally all the way to the anterior longitudinal ligament. Full reduction of the spondylolisthesis was then performed under electromyogram and fluoroscopic monitoring judiciously levering on distally tightened rods engaged in S1 and S2-alar screw heads.
Thereafter, The patient had improvement of his symptoms post-operatively and was discharged 6 days after the second operation. His latest X-rays at 6 months of follow-up showed bony union at L5/S1 (Figure 7). His ODI score was 9 at 6 month follow up.
The dislocated polyaxial screw and the securing nut was sent for an independent laboratory evaluation. Analysis findings were consistent with overload of the multiaxial screw retaining ring and no evidence to suggest a defect in manufacturing of components were found.
Discussion
Pedicle screw is an integral part of the spine surgeon’s armamentarium. It provides strength in reduction and allows rigid fixation for the treatment of wide array of spinal deformities (1). Failure of implants often results due to abnormal high stresses that are transmitted across the instrumentation before bony union occurs (2,3). Multiple modes of implant failure have been described in the literature which includes implant breakage, loosening and screw pullout (2-7). They often lead to poor patient outcomes and the need for revision surgery (4,5). The failure of implants from dislocation of the screw at the polyaxial head-neck junction has not been described in the literature. In this case, apart from the likelihood that the transmitted forces across the implant could have exceeded the ultimate tensile stress of the implant, mechanical weakness at the polyaxial head-neck junction may also have contributed to this rare complication. Results from laboratory testing showing no manufacture defects support a biomechanical cause which resulted in overload of the screw at this weak junction, leading to early failure.
Polyaxial screws are developed to ease the efforts in rod insertion at the expense of the screw strength and its capabilities in deformity correction (8-12). By having an articulating head-neck junction, the load to failure is inevitably weaker compared to monoaxial screws and has been shown in biomechanical studies (2,3,13). When these polyaxial screws are employed in surgery, several measures can be considered to avoid premature failure of these screws and can be demonstrated using this case study.
Reduction of spondylolisthesis has been one of the most controversial topics in lumbar deformity surgery (5,14,15). Advocates of reduction emphasize the need to restore lordosis of the lower lumbar spine and overall sagittal balance which in turn has been shown to determine outcomes of deformity surgery (5,6,16) At the same time, the main objective of achieving bony union in these surgeries has always believed to be the key to surgical success (17,18). Reduction of the spondylolisthesis can then allow more overlapping surfaces for better interbody fusion to occur. Contrary to this, many other surgeons are also plagued by the high rates of neurological deficits following reduction of high grade spondylolisthesis (4-6). Although many parameters have been identified as risk factors resulting in neurological complications, some are not entirely modifiable and the outcome often unpredictable (5,6,19). As such, it may be prudent to consider the real need for reduction of high grade spondylolisthesis on a case-by-case basis.
In the event that reduction is deemed necessary, adequate release is as important as delivering strength in the overall implant construct. Bilateral facet joint release is crucial in these cases and may be supplemented by anterior releases (17,20). In our case report, the patient underwent bilateral complete facetectomy during his index surgery. Albeit this posterior release, reduction was difficult and a suboptimal reduction was accepted by the surgeon. During the revision surgery, additional attempt was also made via the use of cobb elevator to release the annulus from posteriorly. This made the reduction of the olisthesis eventually possible. In terms of improving the strength of the fixation, several factors can be considered. This includes the use of larger diameter pedicle screws, medialisation of pedicle screws, bicortical pedicle screw purchase, cortical bone trajectory technique during insertion, cortical pedicle screws, and placement of more screws with multiple anchor points. In our case, further bicortical S2-alar screws were placed in addition to upsized S1 pedicle screws during the revision surgery. Moreover, larger interbody cages to allow an anterior strut support has also been proposed to improve the strength of the overall construct (17,21,22).
Several authors have described varying techniques in the reduction of spondylolisthesis (4-8,23-26). Concerns of interference resulting from an earlier placed interbody cage generate the fear for cage displacement or screw pullout during the reduction process. In our case study, the initial cage size was 12 mm in height. This cage was removed for the reduction to take place during the revision surgery to reduce the possible interference caused by the interbody cage and the adjacent endplates. New cages were placed bilaterally only after sizing the interbody space post-reduction and smaller 10 mm height cages were then found to be more appropriate. In the author’s opinion, resistance from friction caused by an oversized cage could also have contributed to the increased stress transmitted across the posterior construct. Therefore it remains an option to consider to reduce the olisthesis without an existing interbody cage and to only gauge the appropriate size cage after reduction is achieved. In this way, both the reduction process and the sizing of interbody cages will not be compromised.
Lastly, this patient had an asymmetrical spondylolisthesis with the slippage worse on the right side compared to the left. In such a situation, more reduction occurring on the right side resulted in greater stress borne by the right sided screws. Whilst the posterior instrumentation may be bilateral, asymmetrical failure of implants will be more likely on the right side. As such, supplementary fixation should always be considered if there is any doubt in the screw purchase. Failure of the right sided polyaxial screw at the head-neck junction evidently demonstrates this point.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- McCormick J, Aebi M, Toby D, et al. Pedicle screw instrumentation and spinal deformities: have we gone too far? Eur Spine J 2013;22 Suppl 2:S216-24. [Crossref] [PubMed]
- Camp JF, Caudle R, Ashmun RD, et al. Immediate complications of Cotrel-Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine (Phila Pa 1976) 1990;15:932-41. [Crossref] [PubMed]
- McCord DH, Cunningham BW, Shono Y, et al. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976) 1992;17:S235-43. [Crossref] [PubMed]
- Jutte PC, Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J 2002;11:594-8. [Crossref] [PubMed]
- Lonstein JE, Denis F, Perra JH, et al. Complications associated with pedicle screws. J Bone Joint Surg Am 1999;81:1519-28. [Crossref] [PubMed]
- Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine (Phila Pa 1976) 1993;18:2231-8; discussion 2238-9. [Crossref] [PubMed]
- Devlin VJ, Boachie-Adjei O, Bradford DS, et al. Treatment of adult spinal deformity with fusion to the sacrum using CD instrumentation. J Spinal Disord 1991;4:1-14. [PubMed]
- Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res 1988.10-23. [PubMed]
- Kuklo TR, Potter BK, Polly DW Jr, et al. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2005;30:2113-20. [Crossref] [PubMed]
- Chen SH, Mo Lin R, Chen HH, et al. Biomechanical effects of polyaxial pedicle screw fixation on the lumbosacral segments with an anterior interbody cage support. BMC Musculoskelet Disord 2007;8:28. [Crossref] [PubMed]
- Wang X, Aubin CE, Crandall D, et al. Biomechanical analysis of 4 types of pedicle screws for scoliotic spine instrumentation. Spine (Phila Pa 1976) 2012;37:E823-35. [Crossref] [PubMed]
- Fogel GR, Reitman CA, Liu W, et al. Physical characteristics of polyaxial-headed pedicle screws and biomechanical comparison of load with their failure. Spine (Phila Pa 1976) 2003;28:470-3. [Crossref] [PubMed]
- Serhan H, Hammerberg K, O'Neil M, et al. Intraoperative techniques to reduce the potential of set-screw loosening in long spinal constructs: a static and fatigue biomechanical investigation. J Spinal Disord Tech 2010;23:e31-6. [Crossref] [PubMed]
- Edwards CC, Bradford DS. Instrumented reduction of spondylolisthesis. Spine (Phila Pa 1976) 1994;19:1535-7. [Crossref] [PubMed]
- Transfeldt EE, Mehbod AA. Evidence-based medicine analysis of isthmic spondylolisthesis treatment including reduction versus fusion in situ for high-grade slips. Spine (Phila Pa 1976) 2007;32:S126-9. [Crossref] [PubMed]
- Bradford DS. Treatment of severe spondylolisthesis. A combined approach for reduction and stabilization. Spine (Phila Pa 1976) 1979;4:423-9. [Crossref] [PubMed]
- Moshirfar A, Rand FF, Sponseller PD, et al. Pelvic fixation in spine surgery. Historical overview, indications, biomechanical relevance, and current techniques. J Bone Joint Surg Am 2005;87 Suppl 2:89-106. [PubMed]
- Kleinstueck FS, Fekete TF, Mannion AF, et al. To fuse or not to fuse in lumbar degenerative spondylolisthesis: do baseline symptoms help provide the answer? Eur Spine J 2012;21:268-75. [Crossref] [PubMed]
- Proietti L, Scaramuzzo L, Schiro GR, et al. Complications in lumbar spine surgery: A retrospective analysis. Indian J Orthop 2013;47:340-5. [Crossref] [PubMed]
- Jaumard NV, Welch WC, Winkelstein BA. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng 2011;133:071010. [Crossref] [PubMed]
- Chong E, Pelletier MH, Mobbs RJ, et al. The design evolution of interbody cages in anterior cervical discectomy and fusion: a systematic review. BMC Musculoskelet Disord 2015;16:99. [Crossref] [PubMed]
- Jost B, Cripton PA, Lund T, et al. Compressive strength of interbody cages in the lumbar spine: the effect of cage shape, posterior instrumentation and bone density. Eur Spine J 1998;7:132-41. [Crossref] [PubMed]
- Allen BL Jr, Ferguson RL. A. 1988 perspective on the Galveston technique of pelvic fixation. Orthop Clin North Am 1988;19:409-18. [PubMed]
- Chang TL, Sponseller PD, Kebaish KM, et al. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976) 2009;34:436-40. [Crossref] [PubMed]
- Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976) 2010;35:2245-51. [Crossref] [PubMed]
- Martin CT, Witham TF, Kebaish KM. Sacropelvic fixation: two case reports of a new percutaneous technique. Spine (Phila Pa 1976) 2011;36:E618-21. [Crossref] [PubMed]