Factors predictive of topographical accuracy in spine level localization
Introduction
Topography is defined as the study of the shape or surface of an object. Accurate estimation of the spinous processes and interspinous spaces between T4 and L2 represents a significant challenge (1). As a result, spine level localization by palpation in posterior approach thoracolumbar spine surgeries may be inaccurate. The intercristal line and 12th rib location are common topographic aids. The intercristal line is defined as the line joining the superior aspect of the iliac crests posteriorly (2). Chakraverty et al. suggests that clinical palpation of the intercristal line commonly identifies the L3 or L3–4 spinal levels rather than the L4 or L4–5 levels, particularly in females and patients with higher body mass indices (3). On the other hand, the intercristal line is commonly identified as the L4–5 spinal level on radiographs. This implies that depth differences of subcutaneous adiposity or thickness of thoracolumbar musculature affects the accuracy and reproducibility of clinical palpation in defining spinal levels. Clinical identification of the 12th rib requires radiological confirmation of 12th rib attachment to the T12 vertebral body. Other less reliable landmarks include the tip and spine of the scapula and the C7 spinous process (4).
Following palpation, the surgical site is commonly marked with a sterile needle and confirmed using radiographs. Depending on the confirmatory method used, this process ranges from a single posterior-anterior (PA) radiograph to continuous fluoroscopy of the spinal axis taken in the sagittal or coronal plane from the lumbosacral junction to the region of interest. In the United Kingdom, Public Health England has calculated that on average, people are exposed to about 2.7 millisieverts (mSv) of radiation a year (5). In Canada, the effective dose limit for the public is 1 mSv in 1 calendar year (6). The effective doses for PA and lateral lumbar films were 2.20 and 1.50 mSv, respectively (7). As such, minimizing radiation dose at every step of spine level localization is imperative both to patients and operating room staff.
At present, there is a paucity of literature regarding the predictive factors of accurate spine level localization in posterior approach thoracolumbar surgery. This study aims to investigate potential predictive factors portending spine level localization accuracy and to introduce a novel localization tool for posterior thoracolumbar spine surgery.
Methods
Study design
This was a prospective study. The sample size was determined according to previously described guidelines for the description and validation of new radiological methods (8).
Study population
Consecutive adult (>18 years) patients undergoing primary posterior spine surgery of the thoracolumbar spine (T4–L2) were included. Patients with prior skin incisions from previous spine surgeries were excluded from the study. The spine unit of the study hospital surgically manages patients with simple and complex spine pathology, is a level 1 trauma center and the regional spinal cord injury referral center.
Pathology related spine level localization
Following intubation and prone positioning, the spine level was determined with clinical palpation using anatomical landmarks. The intercristal line was determined and based on it, the pathology related spinous process or interspinous space corresponding to the spinal pathology was estimated and marked using a surgical ink marker. The intercristal line was taken to be the L4–5 spinal level in a young thin male and L3–4 spinal level in all other patients (3). Palpable deformities such as widening of the interspinous space in patients with traumatic flexion distraction injuries and focal kyphosis as seen on pre-operative imaging were adjuncts used to further refine this process. The Target Tape® (Vancouver, BC, Canada) was then placed on the skin overlying the surgical area.
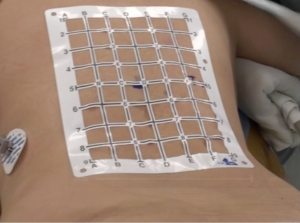
Target Tape®
The Target Tape® is a disposable self-adhesive sheet marked with radio-opaque grid lines. It is lightweight, and spans 6 to 8 vertebral bodies depending on patient size. It is placed over the area of interest as shown in Figure 1. A metallic marker either a Terumo (Shibuya-ku, Tokyo, Japan) 18-gauge 1.5-inch (40 mm) radio-opaque needle or an artery forceps was then placed in a transverse orientation over the ink marker. A thoracolumbar PA radiograph was then acquired (Figure 2). The radiograph was ensured to include either the most caudal or the most cephalad rib to enable spinal level verification. Pre-operative cross sectional imaging was evaluated to rule out anatomic variation, confirming that the T12 vertebral body was the origin of the 12th rib, and the presence of five lumbar vertebrae. Based on the location of the 12th rib and T12 vertebral body, or the location of the 1st rib, the accuracy of the skin localization was assessed. The skin incision was then planned and marked out using the grid. The normal surgical routine was then carried out, including intra-operative spine level localization.

Primary outcome
Accuracy
The primary outcome was the level of agreement between spine level localization using either the pathology related spinous process or interspinous space identified by palpation and the radio-opaque marker. Tiers of accuracy assessment were: (I) accurate; (II) one segment from presumed level; and (III) two or more segments from presumed level.
Secondary outcome
The secondary outcome was to evaluate the factors leading to increased accuracy or the misidentification of the pathology related level. The factors studied are discussed as follows.
Age
The WHO defines the elderly population as those aged 65 and above (9,10). In this age group, major integumentary system changes include the loss of subcutaneous adipose tissue, epidermis atrophy, dermal collagen stiffening, and elastin calcification (11). Furthermore, growth of the epidermal layer slows resulting in the decrease of contact area of the dermis and epidermis, causing easy separation of these layers. This may influence spine level localization as the process of clinical palpation of posterior spine anatomical landmarks may be easier. Assessment of age was dichotomized to: (I) <65 years; (II) 65 years or older (elderly).
Gender
Males and females have differing distribution of body adiposity. In the areas overlying the thoracolumbar spine, the deposition of fat in males is often in the abdominal region as opposed to females who deposit fat in the subcutaneous tissues in the back (12). Assessment of gender was dichotomized to: (I) male; (II) female.
Body mass index (BMI)
This metric gives an overview of the size of a patient and assumes that patients who are obese have significant generalized subcutaneous adiposity regardless of gender. Calculations of BMI were dichotomized to: (I) BMI <30; and (II) BMI of 30 or more indicating obesity (13).
Pathology related interspinous segments
This study investigated pathologies affecting T4 to L2. To further ascertain whether each segment had inherent complexities due to distance from the intercristal line, 12th rib, and topography of the scapula, this variable was divided into three interspinous segments: (I) T4–T8; (II) T8–T12; and (III) T12–L2.
Palpable deformity
This study defined palpable deformity as an obvious widening of the interspinous distance (ISPD) or protrusion of the skin as seen in flexion distraction injuries or post traumatic kyphosis. It does not refer to patients with scoliosis or fused spinous processes often seen in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis.
Pathology related ISPD
Being able to palpate interspinous segments and spinous processes allow the physical identification of subjacent levels using localizing anatomical landmarks such as the intercristal line or the 12th rib. This variable is defined as the distance between the posterior-most tip of the spinous processes wherein the lesion was contained on MRI. We stratified ISPD into: (I) 10 mm or less; and (II) more than 10 mm.
Pathology related spinous process to skin distance
Patients with high BMI and females are expected to have greater spinous process to skin distance and hence would be expected to be associated with poorer accuracy of localization. This variable is defined as the distance between the posterior-most tip of the spinous processes to the skin wherein the lesion was contained on MRI. If the lesion involved two spinous processes, this distance was measured using the caudal spinous process as palpation to determine spinal level is usually performed from the caudal to cephalad. We stratified this metric into: (I) 20 mm or less; and (II) more than 20 mm.
Statistical analysis
Univariate descriptive and inferential statistical methods were used to examine the distribution of the demographic, outcome and predictive variables. Crosstabulation, a joint frequency distribution of cases based on two or more categorical variables was used to investigate for relationships between the variables. Contingency table analysis was also utilized in a similar fashion. The joint frequency distribution was analyzed with the Chi-squared statistic to determine whether the variables were statistically independent or if they were associated. Statistical significance was designated as a P value of less than 0.05. Statistical analyses were performed using SPSS (version 23.0, IBM, Chicago, IL, USA).
Ethics
The study protocol was reviewed and approved by the Clinical Research Ethics Board of the University of British Colombia, Vancouver, Canada (protocol H15-02787).
Results
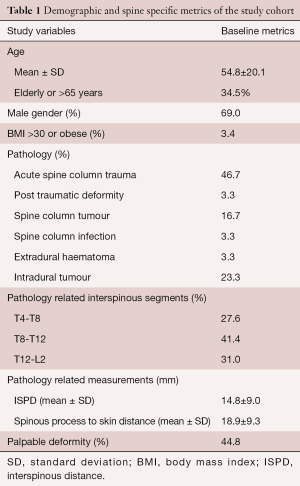
Thirty consecutive patients (69% male) undergoing primary posterior spine surgery from T4 to L2 were included in this study. Patients were consecutively recruited from November 1, 2015 to April 28, 2016. Mean and standard deviation values at assessment were: age, 54.8±20.1 years; 34.5% elderly; and 1 (3.4%) patient with BMI >30 or obese. The primary pathologies affecting the majority of patients were trauma (46.7%), intradural tumours (23.3%), and spine column tumours (16.7%) (Table 1). The most common pathology related interspinous segments were between T8 to T12 (41.4%), followed by T12 to L2 (31%) and T4 to T8 (27.6%). Forty four point eight percent of the patients had palpable deformities as a result of flexion-distraction traumatic injuries and post-traumatic kyphosis. The mean [± (standard deviation) SD] pathology related ISPD was 14.8±9.0 mm and mean (± SD) pathology related spinous process to skin distance was 18.9±9.3 mm.
Full table
Accuracy of pathology related spine level localization
Table 2 shows the accuracy of spine level localization using knowledge of topographical anatomy alone. Sixty percent of the patients had inaccurate spine level localization utilizing conventional clinical palpatory methods, while 26.7% were one spinal level inaccurate, and 33.3% were two spinal level(s), respectively. There were no patients localized inaccurately by more than 3 levels.

Full table
Predictive factors of pathology related spine level localization accuracy
Elderly
No association was identified between age (elderly vs. not elderly) to pathology related spine level localization (P=0.27).
Gender
No association was identified between gender and pathology related spine level localization (P=1.00).
BMI
Our study only had one patient who was obese (BMI of more than 30). However, that patient had accurate localization of his pathology related spine level.
Pathology related interspinous segments
Patients with pathology between T12–L2 had a 55.5% chance of accurate pathology related spine level localization while patients with pathology between T4–T8 and T8–T12 had less than 50% chance of accurate pathology related spine level localization. No association was identified between pathology related interspinous segments and pathology related spine level localization (P=0.50).
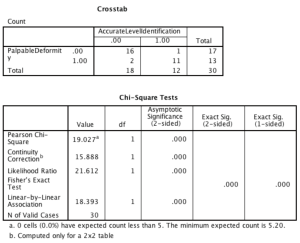
Palpable deformity
Patients with flexion-distraction injuries and focal kyphotic spine deformities had 84.6% chance of accurate pathology related spine level localization. This variable achieved statistical significance with P value of <0.001 respectively (Figure 3).
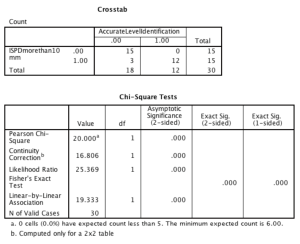
Pathology related ISPD
All patients with pathology related ISPD of less than 10 mm were inaccurately localized using clinical palpation and topographical landmarks whereas 80% of those with pathology related ISPD of more than 10 mm were accurately localized (P<0.0001) (Figure 4).
Pathology related spinous process to skin distance
Patients with pathology related spinous process to skin distance of less than 20 mm had a 44.4% chance of accurate pathology related spine level localization. No association was identified between pathology related spinous process to skin distance and pathology related spine level localization (P=0.47).
Discussion
This study is novel as it prospectively evaluates a spine surgeon’s ability to localize the pathology related spine segments using anatomical landmarks and investigates for factors predictive of localization accuracy. This study confirms that localization of pathology related spinal segments using anatomical landmarks is challenging in the thoracic and upper lumbar spine. This study, performed at a tertiary spine referral center, revealed only 40% accuracy of spine level localization utilizing conventional clinical palpation of anatomic structures, with 33.3% being inaccurate by two segments. The localization process was performed by either the staff surgeons or their fellows. This inaccuracy was not detrimental to the patient as the level was subsequently confirmed pre-operatively, using a PA radiograph of the thoracolumbar spine and the Target Tape® and intra-operatively, as per standard technique.
Mody et al., conducted a survey of members of the American Academy of Neurologic Surgeons which showed that 15% reported that, at least once, they had prepared the incorrect spine level, but noticed the mistake before making the incision (14). Half of the surgeons reported that they had done 1 or more wrong level surgeries during their career (14). As this is a self-reported study and retrospective in nature, it is inferred that this is likely an underestimate of the true incidence of incorrect spine level localization. Also, despite being accurate with level localization, the length of the skin incision may be inaccurate if level determination was performed using palpation alone, especially if the operated segments are very far apart. This could significantly increase the length of an already very long skin incision and prolong surgical time. In our prospective cohort, the Target Tape® was used to pinpoint the location of the spinous processes, pedicles and transverse processes of the entire operative region. This aided surgical exposure greatly. It also aided in the accurate placement of the spinous process array used for neuronavigation image acquisition. We found that it was useful in the determination of the length of rod required in instrumented cases, in particular minimally invasive (MIS) cases.
There is a paucity of literature on the reasons of inaccurate spinal localization. This study identified seven potential predictive variables of posterior thoracolumbar spinal localization. We included age, gender, pathology related spinous process to skin distance and BMI to address the effect of integumentary changes and adiposity predilection on the accuracy of clinical palpation. Previously, there had only been anecdotal evidence that BMI affects the accuracy of spine level localization. Unfortunately, as there were insufficient numbers, we are unable to draw any conclusions about the impact of obesity on spine level localization. Despite that, this study showed that the distance between the spinous process to the skin, which is expected to be larger in obese patients, had no effect on the accuracy of spine level localization. This is interesting as one would surmise that a short spinous process to skin distance would be a positive predictive factor of spinal localization accuracy.
Rather, the pathology related ISPD was shown to be the main predictive factor. From our study, it would seem that an ISPD of 10 mm or less would be difficult to palpate and lead to inaccuracy of spine level localization. On the other hand, large ISPDs such as in traumatic flexion distraction injuries or focal kyphotic deformities would be easily perceived and appreciated, and lead to improved accuracy. Perhaps 10 mm is the threshold of a gloved finger pad in proprioceptive accuracy.
To improve the accuracy of spine level localization, spine surgeons have previously introduced skin surface radio-opaque markers such as longitudinal grid tube surface markers (15,16), adhesive disposable skin markers (17) and percutaneously inserted fiducial screw markers (18). For this purpose, the Target Tape® is a valuable resource. It is easy to use, time saving and of low cost. It potentially decreases the radiation dose both to the patient as well as to the surgical team as it only requires a single PA thoracolumbar radiograph for level localization.
The Target Tape® is a large grid and non-invasive which eliminates repeated iterations of needle insertions and placement of multiple fiducial or other disposable skin markers. The grid has an adhesive surface that prevents movement relative to the skin. As this method utilizes a PA thoracolumbar radiograph, it is imperative that 12th rib is confirmed to originate from the T12 vertebral body. This grid can also be used for the spinal regions between T1 and T4. Despite expected radiographic inaccuracy in this region due to the change in sagittal alignment of the cervicothoracic junction, the Target Tape® would still be more accurate than previously used methods. In institutions where pre incisional films are difficult to obtain in a timely manner, a target tape (TT) may be applied to a patient in the radiology department prior to the surgery. As the TT is self-adhesive it will not move during transport to the OR. This may allow further savings of valuable operative time.
Conclusions
This study showed that poor spine level localization using anatomical landmarks was associated with pathology related ISPDs of less than 10 mm. Conversely, patients with palpable spinal deformity have their levels easily localized.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study protocol was reviewed and approved by the Clinical Research Ethics Board of the University of British Colombia, Vancouver, Canada (protocol H15-02787) and written informed consent was obtained from all patients.
References
- Harlick JC, Milosavljevic S, Milburn PD. Palpation identification of spinous processes in the lumbar spine. Man Ther 2007;12:56-62. [Crossref] [PubMed]
- Williams P, Warwick R. editors. Gray's Anatomy - 36th Edition. Edinburgh: Chruchill Livingstone; 1980.
- Chakraverty R, Pynsent P, Isaacs K. Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines? J Anat 2007;210:232-6. [Crossref] [PubMed]
- Cooperstein R, Haneline MT. Spinous process palpation using the scapular tip as a landmark vs a radiographic criterion standard. J Chiropr Med 2007;6:87-93. [Crossref] [PubMed]
- Public Health England. Ionising radiation: dose comparisons. Retrieved May 23, 2016. Available online: https://www.gov.uk/government/publications/ionising-radiation-dose-comparisons
- Canadian Nuclear Safety Commission. Radiation doses. Retrieved May 23, 2016. Available online: http://nuclearsafety.gc.ca/eng/resources/radiation/introduction-to-radiation/radiation-doses.cfm
- Simpson AK, Whang PG, Jonisch A, et al. The radiation exposure associated with cervical and lumbar spine radiographs. J Spinal Disord Tech 2008;21:409-12. [Crossref] [PubMed]
- Harrison DE, Harrison DD, Cailliet R, et al. Radiographic analysis of lumbar lordosis: centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine (Phila Pa 1976) 2001;26:E235-42. [Crossref] [PubMed]
- Orimo H, Ito H, Suzuki T, et al. Reviewing the definition of “elderly”. Geriatr Gerontol Int 2006;6:149-58. [Crossref] [PubMed]
- World Health Organization. Proposed working definition of an older person in Africa for the MDS Project. Retrieved June 1, 2016. Available online: http://www.who.int/healthinfo/survey/ageingdefnolder/en/
- Oster KA, Oster CA. Special needs population: Care of the geriatric patient population in the perioperative setting. AORN J 2015;101:443-56. [Crossref] [PubMed]
- Power ML, Schulkin J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br J Nutr 2008;99:931-40. [Crossref] [PubMed]
- Flegal KM, Carroll MD, Kuczmarski RJ, et al. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord 1998;22:39-47. [Crossref] [PubMed]
- Mody MG, Nourbakhsh A, Stahl DL, et al. The prevalence of wrong level surgery among spine surgeons. Spine (Phila Pa 1976) 2008;33:194-8. [Crossref] [PubMed]
- English PT, Dougal C, Griffiths PD, et al. Technical note: a simple method for skin/lesion localization using magnetic resonance imaging. Br J Radiol 1994;67:813-5. [Crossref] [PubMed]
- Thomson JL. A simple skin marker for magnetic resonance imaging. Br J Radiol 1988;61:638-9. [Crossref] [PubMed]
- Rosahl SK, Gharabaghi A, Liebig T, et al. Skin markers for surgical planning for intradural lesions of the thoracic spine. Technical note. Surg Neurol 2002;58:346-8. [Crossref] [PubMed]
- Upadhyaya CD, Wu JC, Chin CT, et al. Avoidance of wrong-level thoracic spine surgery: intraoperative localization with preoperative percutaneous fiducial screw placement. J Neurosurg Spine 2012;16:280-4. [Crossref] [PubMed]
Contributions: (I) Conception and design: JW Tee; (II) Administrative support: JW Tee; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: JW Tee, T Marion, J Rutges; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.


