Decompression versus decompression and fusion for degenerative lumbar stenosis: analysis of the factors influencing the outcome of back pain and disability
Introduction
Degenerative lumbar spinal stenosis describes a condition in which there is diminished space available for the neural and vascular elements in the lumbar spine, secondary to degenerative changes in the spinal canal (1). Recent randomized trials have shown that surgery is more effective than non-operative treatment for patients with lumbar stenosis (2). Surgical options include decompression and decompression plus fusion. Decompression alone is suggested for patients not affected by back pain without instability. Lumbar fusion is considered appropriate in patients with concomitant spondylolisthesis (3).
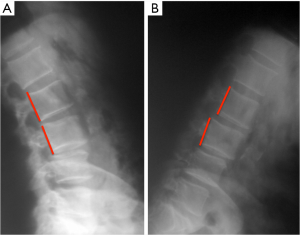
The indications for fusion in patients without concomitant spondylolisthesis have not been clarified (4). There is evidence indicating that patients with lumbar stenosis, without deformity or instability, treated with wide decompression or facetectomy may suffer from iatrogenic lumbar instability (5). Dynamic X-rays in flexion and extension is used by some authors to detect a “hidden” lumbar instability (6), but it is still unclear how to consider and treat it. In this article we use the terms of “hidden spondylolisthesis”, “dynamic instability” or “micro-instability” as synonyms indicating the minor spondylolisthesis detectable at the flexion-extension X-ray but not present on static imaging. The objective of this study is to analyze the results in patients operated for lumbar stenosis without instability and deformity.
Materials and methods
Participants in this study include consecutive patients undergoing surgery for degenerative lumbar stenosis without deformity, spondylolisthesis or instability at our Department from June 2010 to January 2014. Patients undergoing standard posterior decompression or standard posterior decompression plus pedicle screw fixation were eligible for recruitment. All the patients underwent clinical examination, 3T-MRI scan, CT scan and static and dynamic X-ray for preoperative assessment.
Inclusion criteria were: pre-operative midsagittal spinal canal diameter of 12 mm or less on CT scan, ongoing symptoms for a minimum of 12 weeks with no improvement to conservative treatment. Exclusion criteria were: congenital, traumatic and neoplastic lumbar stenosis, spondylolisthesis (on static X-ray), lumbar scoliosis (Cobb>10°), previous lumbar surgery, other types of operations (endoscopic decompression, anterior interbody fusions, interspinous devices etc.). Recruited patients were divided into two groups: Decompression group (D) and Decompression-Fusion group (F).
Setting
An independent spinal surgeon reviewed clinical records and neuroimaging (3T-MRI scan, CT scan and static and dynamic X-ray) of the selected patients. All the patients underwent static and dynamic X-ray. Dynamic X-ray was executed in both standing and recumbent position, obtaining a maximal movement of both flexion and extension. Patients were assigned to the “micro-instability” group if they presented a sagittal translation ≥4 mm or ≥8% and a sagittal rotation ≥10° in L1–L5 and ≥ 2° in L5–S1 (as widely accepted by many authors) (7).
All the patients were interviewed by a psychologist for evaluation of lumbar back pain and disability on June 2015. Back pain was assessed by the Graphic Rating Scale (GRS) (8); Disability by the Oswestry Disability Index (ODI) 2.0 (9).
We analyzed the following factors: age, gender, levels of stenosis, pre-surgical “micro-instability”, post-surgical “micro-instability”.
Statistical analysis plan
We conducted t-tests to analyze if the variations of Pain and Disability were related to the surgical operation. Two analyses of variance were conducted to verify the results of the types of surgery and their interaction with age and gender. The Age factor was obtained dividing the total ages of patients into three classes: under 65 years old (adult), from 65 to 75 (young-old) and over 75 (old).
Two analyses of variance were used to investigate the effect of surgery on the decrease of Pain and Disability according to the levels of stenosis, pre-surgical micro-instability and post-surgical micro-instability. Four categories based on the number of levels involved were created (1, 2, 3 and 4 or more levels).
Finally, we conducted two analyses of variance within two groups: decompression (D) and decompression/fusion (F).
The level of significance for all analyses was chosen at P<0.05. Statistical interpretation of the data was executed using SPSS v19 software (SPSS Inc., Chicago, Illinois, USA).
Results
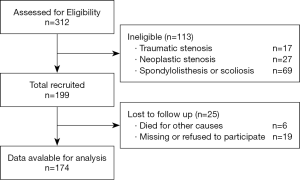
We analyzed a cohort study according to the STROBE guidelines (10). The analysis was conducted through outpatient visit and clinical records evaluation. The follow-up ranged from 18 to 60 months [mean 38.56 months; standard deviation (sd) =9.72]. Among 312 patients undergoing surgery for lumbar stenosis, 69 were excluded since they were affected by concomitant spondylolisthesis or scoliosis, 44 were excluded as they were treated with other techniques, 6 died for other causes and 19 were missing or refused to participate (Figure 1).
A total of 174 patients were enrolled in the study. There were 93 males (53.4%) and 81 females (46.6%), with a mean age of 65.29 (sd=10.0). The range of follow up was from 18 to 60 months (mean 38.56 months; sd=9.72).
The pre-surgical micro-instability was observed in 72 cases (41.4%), 50 (69.4%) female and 22 (30.6%) male (Figure 2). About 102 patients (58.6%) reported no abnormal movements on dynamic X-ray. Decompression (D) was executed in 82 cases (47.1%); 41 (50%) were female with a mean age of 68.22 (sd=9.49) and 41 (50%) patients were male with a mean age of 64.66 (sd=8.36). Decompression-Fusion (F) was executed in 92 cases (52.9%); 52(56%) were female with a mean age of 65.20 (9.68) and 40 (40.3%) were male with a mean age of 64.43 (sd=9.72).
In the post-surgical period, 20 (24.4%) D group patients had vertebral micro-instability; 11 (26.8%) were female and 9 (22%) male. Among F group patients, only 3 (5.8%) had vertebral micro-instability; all of them were female. All these patients had post-surgical micro-instability in the vertebra just above the fixation (junction syndrome).
No difference between D and F groups was observed in terms of pre-surgical GRS {M =7.45, sd=0.15 and M=7.53, sd=0.14 respectively for D and F group patients, F [1,172] =0.154, P=0.69}. The composition of the sample in terms of age and gender, and the distribution of these indicators in the two types of surgery, leads us to compare adequately the dependent measures using statistical analysis.
We conducted two t-tests to investigate the decrease of pain and disability depending from surgery. Results showed that both GRS and ODI scores had a statistically significant decrease after surgery (P<0.001).
The mean score of GRS in pre-surgical period was 7.49 (sd=1.363) while in the post-surgical period was 2.46 (sd=2.394).
The mean score of ODI in the pre-surgical period was 47.55 (sd=10.478) while in the post-surgical period was 11.56 (10.803).
Effect of surgery, age and gender on decrease of pain (GRS) and disability (ODI)
An analysis of variance using the decrease of pain (GRS pre-post) as dependent variable and Type of surgery (D-F), Age, Gender and their interaction as factors showed that only the Main effects of the factors were significant. No interaction from these factors was statistically significant. The main effect of type of surgery {F [1,173] = 4.88, P= 0.02, η2partial=0.29}, age {F [1,173] = 3.87, P= 0.02 η2partial= 0.46} was statistically significant and gender {F [1,173] =3.20, P= 0.07, η2partial= 0.19} was trending towards significance (Table 1).
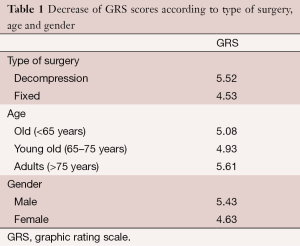
Full table
The analysis obtained on the decrease of disability (ODI pre–post) revealed: the main effects of surgery, gender and age were not significant; the three-way interaction between surgery, gender and age was significant. This result means that the factors had no independent effect on the decrease of disability but their interaction can reveal significance differences (Table 2).
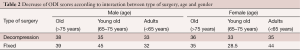
Full table
Effect of surgery on the decrease of pain (GRS) and disability (ODI) depending from: levels of stenosis, pre-surgical micro-instability and post-surgical micro-instability
An analysis of variance was used for testing the decrease of pain (GRS) and disability (ODI) according to the levels of stenosis [1-2-3-4]. Results showed a significant interaction for GRS scores {F [1,173] =4.08, P= 0.008, η2partial=0.67} (Table 3) and no interaction for ODI scores (P=0.10).
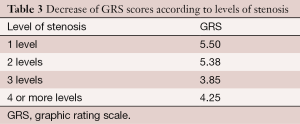
Full table
Further analyses of variance revealed no significant interaction between either decrease of pain scores (GRS) or disability scores (ODI) with type of surgery (D F) (P=0.20 and P=0.83).
Another analysis of variance was conducted to test the hypothesis that the pre-surgical micro-instability could have effects on decrease of pain (GRS) and disability (ODI) according to the type of surgery (D-F) and the levels of stenosis. No significant interaction could be found. Only the main effect of pre-surgical micro-instability on GRS was significant (P=0.007); patients with a pre-surgical micro-instability had a lower decrease on pain (mean=5.49 vs. mean=4.38) (Table 4).
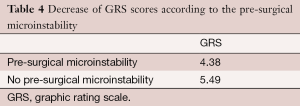
Full table
Analyses within two groups: decompressed (D) and fixed (F)
Decompression Group: A one-way analysis of variance was conducted on Decompressed-patients without pre-surgical micro-instability using the post-surgical micro-instability as factor. Results {F [1,69] =20.11, P<0.01, η2partial=0.22} showed a significant interaction (Table 5).
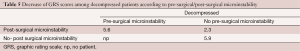
Full table
Fusion Group: For what concern patients undergoing decompression and Fusion, the analysis of variance reveals a significant interaction {F [1,59] =5.25, P=0.02, η2partial =0.83} (Table 6).
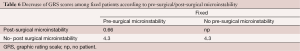
Full table
The results for ODI scale revealed similar results: fixed patients having both a pre-and post-surgical micro-instability reported the lowest improvement in disability with a mean ODI score decrease of 15 points {F [1,59]=6.86, P=0.01, η2partial=0.10}. Decompression patients having no pre-surgical micro-instability but reporting a post-surgical micro-instability had a mean ODI score decrease of 27,37 {F [1,69]=3.48, P=0.06, η2partial=0.49}. In all the other cases, the mean scores of decrease on disability were ranging from 34 to 38 points.
Discussion
The overall decrease of GRS and ODI scores between pre- and post-surgery is statistically significant. The female patients have lower benefits from surgery, either for decompression alone or decompression and fusion group. The overall decrease of pain and disability after surgery is lower for females. Patients with three or more levels of stenosis reported lower decrease in pain and disability comparing with patients with one or two levels of stenosis. As expected, a stenosis involving more levels is a more severe disease than a stenosis involving one or two, and requires a more aggressive surgery (11). Analysis of the results about disability shows that benefits derived from the type of surgery cannot be considered absolutely, but have statistically significant values only if considered in relation to age and gender. The young-old female patients that underwent fixation surgery reported the least improvement in disability. We conclude that the effect of the type of surgery on the decrease of pain and disability is influenced by the levels of stenosis. We suggest that even if not statistically significant, the lower improvement in symptoms obtained from patients with four or more levels of stenosis should be interesting to investigate; for example, the lower improvement in disability obtained from patients with four levels of stenosis that underwent posterior decompression (D) comparing to those underwent fixation (F) (mean =11 vs. mean =24 respectively).
The micro-instability
“Micro-instability” is a common occurrence in our patient sample, as reported in approximately 40% of cases. Some surgeons use flexion-extension X-ray to evaluate if there is “micro-instability” and fuse these patients (6). However nothing is known about the natural history of the micro-instability group, and no validated study shows how to interpret and treat this condition. In our study the patients with a pre-surgery micro-instability had a lower decrease of pain (mean=5.49 vs. mean=4.38) regardless of the type of surgery. This evidence indicates that: (I) patients affected by lumbar stenosis with micro-instability are more serious than those affected by lumbar stenosis alone; (II) the stabilization is not more effective than laminectomy in reducing the symptoms associated with micro-instability.
It is still unclear whether the pain associated with micro-instability is caused by the slippage of the vertebra or by other factors as morphological changes of the vertebral column and facet joints. Different results have been deduced from the analyses about iatrogenic micro-instability. Patients with post-surgical micro-instability have the worst outcome, whether they are fused or decompressed alone. It is interesting to note that decompressed patients who had a pre-surgical micro-instability (that did not get worse in post-surgical period) have an outcome quite comparable to the decompressed patients without pre-surgical and post-surgical instability.
Pre- and post-surgical micro-instability are two different events. The iatrogenic micro-instability should be considered as a complication of surgery. It is associated with the highest GRS scores, particularly in fixed patients (junction syndrome). However it can develop also after simple laminectomy, when the vertebral metamere weakens. Some studies conclude that lumbar fusion and instrumentation are not associated with an increased rate of reoperation at index or adjacent levels compared with non-fusion techniques (12,13).
Posterior decompression alone or plus fusion?
Our study supports posterior decompression as the preferred option in this patient cohort. Sometimes the choice of the surgeon is to stabilize the spine even in the absence of micro-instability. In patients with degeneration of the disk and facet joints, it can be difficult if not impossible to remove the lamina, the ligamentum flavum, and perform a foraminotomy without weakening the vertebral metamere.
The fixation can have an indication to avoid the risk of iatrogenic instability. In the assessment of that risk, the surgeon must consider: the height of the disk, the degeneration of facet joints and ligaments, the presence of osteoporosis, but also the structure of the whole column and then the sagittal balance.
Conclusions
The present series must be interpreted in the context of its limitations: the retrospective nature of the review and the fact that patients were not randomized. Therefore the groups are not homogeneous and comparable.
Posterior decompression appears to be the gold standard option for treatment of lumbar stenosis without instability and deformity. The dynamic X-ray plays a negligible role in the pre-operative period. It has its utility in the post-operative period in order to assess the existence of an iatrogenic instability. The fixation should be considered only to prevent post-surgical instability. If the patient has a dynamic instability detected by a dynamic X-ray, the choice of fusion is not justified by a clinical benefit. The “micro-instability” is a radiological finding that has its clinic surrogate but is not able to guide the choice of the type of surgery. Moreover the significance of “micro-instability” is still unclear. We suggest a prospective study following patients with asymptomatic micro-instability to definitively understand the clinical history.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kreiner DS, Shaffer WO, Baisden JL, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 2013;13:734-43. [Crossref] [PubMed]
- Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 2008;358:794-810. [Crossref] [PubMed]
- Resnick DK, Watters WC 3rd, Sharan A, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: lumbar fusion for stenosis with spondylolisthesis. J Neurosurg Spine 2014;21:54-61. [Crossref] [PubMed]
- Resnick DK, Watters WC 3rd, Mummaneni PV, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 10: lumbar fusion for stenosis without spondylolisthesis. J Neurosurg Spine 2014;21:62-6. [Crossref] [PubMed]
- Jolles BM, Porchet F, Theumann N. Surgical treatment of lumbar spinal stenosis. Five-year follow-up. J Bone Joint Surg Br 2001;83:949-53. [Crossref] [PubMed]
- Landi A, Gregori F, Marotta N, et al. Hidden spondylolisthesis: unrecognized cause of low back pain? Prospective study about the use of dynamic projections in standing and recumbent position for the individuation of lumbar instability. Neuroradiology 2015;57:583-8. [Crossref] [PubMed]
- Dupuis PR, Yong-Hing K, Cassidy JD, et al. Radiologic diagnosis of degenerative lumbar spinal instability. Spine (Phila Pa 1976) 1985;10:262-76. [Crossref] [PubMed]
- Freyd M. The Graphic Rating Scale. J Educ Psychol 1923;14:83-102. [Crossref]
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- STROBE Statement: STrengthening the Reporting of OBservational studies in Epidemiology. 2008. Available online: http://www.strobe-statement.org/News%20Archive.html
- Sigmundsson FG, Jönsson B, Strömqvist B. Preoperative pain pattern predicts surgical outcome more than type of surgery in patients with central spinal stenosis without concomitant spondylolisthesis: a register study of 9051 patients. Spine (Phila Pa 1976) 2014;39:E199-210. [Crossref] [PubMed]
- Radcliff K, Curry P, Hilibrand A, et al. Risk for adjacent segment and same segment reoperation after surgery for lumbar stenosis: a subgroup analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976) 2013;38:531-9. [Crossref] [PubMed]
- Kim CH, Chung CK, Park CS, et al. Reoperation rate after surgery for lumbar spinal stenosis without spondylolisthesis: a nationwide cohort study. Spine J 2013;13:1230-7. [Crossref] [PubMed]