
Multi-modal pain control regimen for anterior lumbar fusion drastically reduces in-hospital opioid consumption
Introduction
The United States is in the midst of an unprecedented opioid epidemic. More than 2 million people are addicted to prescription opioids (1). The rate of deaths involving opioid overdose has increased over 200% since 2000 (2). Recent studies have shown that surgery is a risk factor for developing opioid dependence (3-5). In opioid-naive patients, 3% continued to use opioids for more than 90 days after major elective surgery (3). A greater amount of initial opioid use is associated with greater risks of long-term use, misuse, and overdose (6,7).
Opioids have numerous dose-dependent adverse effects, including nausea, ileus, urinary retention, respiratory depression, hyperalgesia, and delirium, which can impair postoperative recovery. Additionally, opioids are associated with worse clinical outcomes including higher complication rate, longer hospital stay, higher costs, and need for early revision surgery (8-11). Thus, perioperative opioid use should be limited to the lowest effective dose and the shortest duration.
The multimodal pain control (MMPC) approach was developed to decrease perioperative opioid consumption (12). The principle of MMPC is to use multiple agents in a combination of both systemic and regional anesthesia in efforts to reduce overall opioid consumption. MMPC targets several different pathways and mediators involved in nociception to improve analgesic effect, reduce the doses of each agent to minimize the side-effects (12,13). MMPC has been reported to be associated with less postoperative pain and opioid consumption, shorter hospital stay, and increased patient satisfaction in other elective orthopedic procedures (14-16).
In spine surgery, several studies have examined the efficacy of MMPC. Intravenous lidocaine, ketamine, postoperative intramuscular local anesthetic infiltration, and oral pregabalin have been reported to reduce postoperative pain and opioid consumption (17-20). The number of patients undergoing spine surgery is increasing (21) and patients with spine pathology have a high incidence of preoperative opioid use, ranging from 20% to 55% (22,23). Alarmingly, as much as 38% of patients undergoing spine surgery were still on opioids one year after surgery (24). Given these reports, developing a protocol to minimize opioid consumption following elective spine surgery is of paramount importance. Here, we established the perioperative pain management protocol using MMPC approach. The purpose of this study was to evaluate the efficacy of the protocol on patients undergoing single-level anterior lumbar interbody fusions (ALIF).
We present the following article/case in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-629).
Methods
Subject
This is a retrospective comparative study. A retrospective review of a prospective, single-surgeon, surgical database was utilized for consistency in surgical technique. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of University of Louisville (#18.1197) and individual consent for this retrospective analysis was waived. Consecutive patients undergoing single-level ALIF with subsequent posterior fixation/fusion for degenerative lumbar conditions were identified before and after initiation of the MMPC protocol.
Sample size calculation
The sample size calculation is based on the parameters α=0.05 (two-sided) and power: 1-β=0.8. With MMPC having a medium effect size of 0.5 on reducing postoperative opioid consumption the sample size was calculated to be 102.
Outcome
Our primary outcome was total, in-hospital opioid consumption, which was calculated and normalized to the morphine milligram equivalents (MMEs). Postoperative opioids were administered based on doctors’ pro re nata order and pain severity. Total daily opioid consumption was calculated and converted to the MMEs as follows:
MMEs = total dose (mg) × MME conversion factor
MME conversion factor is 0.1 for tramadol, 1 for morphine and hydrocodone, 1.5 for oxycodone, and 4 for hydromorphone. Then, MMEs of used opioids were added.
We compared baseline demographic, surgical data [estimated blood loss (EBL), surgical time, level fused, and primary vs. revision], and preoperative opioid use as all of these could affect postoperative pain and opioid use. We defined revision surgery as history of spine surgery involving the same level, such as pseudoarthrosis and adjacent segment disease. As well as baseline demographic, the length of hospital stay (LOS), cost, rate of postoperative ileus were assessed.
Surgical procedure
Patients were placed in the supine position. The approach was transperitoneal for L5–S1 and retroperitoneal for the proximal levels. For the transperitoneal approach, a transverse incision was made between the umbilicus and the symphysis pubis. The exposed linea alba was vertically divided using monopolar diathermy. Peritoneum was bluntly perforated, and colon was retracted superiorly and laterally. The retroperitoneum was divided in the middle line, and the iliac arteries and veins are then retracted laterally, with the median sacral vessels double clipped and divided. The anterior disc space dissection is performed with a Kittner to avoid injury to the sympathetic nerves to reduce the risk of retrograde ejaculation.
Retroperitoneal approach was done using a left paramedian incision. The anterior rectus sheath was opened, and the rectus mobilized laterally. A retroperitoneal pocket was created bluntly to place a spinal Thompson retractor and blunt dissection carried out between the iliac vessels and psoas muscles.
Once the disc of interest was exposed, the disc was excised using a knife followed by Cobb elevator and endplate preparation tools. It was then dilated to accommodate a cage. The endplates were cleaned off all disc, and the posterior annulus was exposed. A cage was packed with an allograft and bone graft substitutes or extenders. It was impacted into the disc space with good fit and fixation. Patients were then positioned in the prone position and posterior fusion were performed in standard fashion.
Regimen
The MMPC protocol consisted of a preoperative oral regimen of cyclobenzaprine (10 mg), gabapentin (600 mg), acetaminophen (1 g), and methadone (10 mg). Postoperatively patients received a bilateral transverse abdominis plane (TAP) block with 0.5% Ropivacaine prior to extubation. This regimen is based on the fact that patients undergoing combined procedure typically complain of abdominal pain as well as back pain and spasm postoperatively. Therefore, we included TAP block in addition to standard pain medications such as cyclobenzaprine, gabapentin, and acetaminophen.
Statistical analysis
Difference between groups were analyzed using Fisher exact test for categorical variables or Mann-Whitney U test for continuous variables. All statistical analyses were performed using SPSS Statistics 25 (IBM Corp., Armonk, NY, USA). A statistical significance was defined as P value <0.05.
Results
Patient demographics
In total, 68 patients in the MMPC cohort and 39 in the non-MMPC cohort were identified. There was no difference in baseline demographics including sex, body mass index (BMI), smoking status, or preoperative opioid use between the two groups. The MMPC cohort was older (56.8 vs. 51.6 years, P=0.026). There was no difference in surgical data including operative time, EBL, number of fused levels, and rate of revision surgery (Table 1).
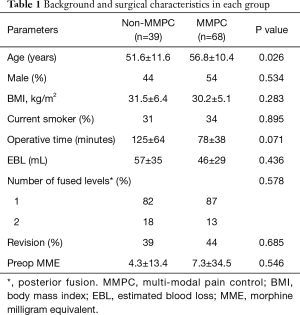
Full table
In-hospital opioid consumption
Although there was no difference in the MMEs on the day of surgery (58.5 vs. 66.9, P=0.387), cumulative MMEs each day after surgery was significantly lower in the MMPC cohort, with final cumulative MMEs being reduced by 62% (120.2 vs. 314.8, P<0.001) (Table 2).
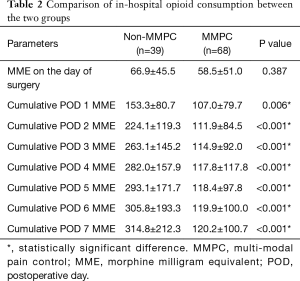
Full table
Secondary outcomes
Postoperative ileus was identified more in the non-MMPC cohort (6 patients; 15%) compared to the MMPC cohort (4 patients; 6%) although there was no statistical difference (P=0.102). Similarly, there was no difference in LOS (4.5 days in the non-MMPC; 3.8 days in the MMPC, P=0.246) and index hospital costs ($24,627 in the non-MMPC; $25,755 in the MMPC, P=0.824).
Discussion
MMPC was initially introduced in abdominal surgery and is currently used in orthopedic and spine procedures. Although some studies have shown that MMPC reduced opioid consumption (16,25-27) other studies have not (28). A variety of agents are available for MMPC and have been studied to reduce postoperative opioid consumption. There are numerous reports detailing the efficacy of acetaminophen for postoperative pain management, showing reduced LOS, opioid consumption, and complication rate (29-31). Gabapentin also has been studied regarding its efficacy in the reduction of postoperative pain and opioid consumption (16,32,33). TAP block has been considered an effective analgesia for abdominal surgery (34,35). These studies examined the efficacy of a single modality, with each medication having a significant benefit in reducing postoperative opioid consumption. Since our patients underwent ALIF and subsequent posterior fusion surgery, our regimen included a combination of oral agents and a TAP block. In our cohort and regimen, MMPC significantly decreased in-hospital opioid consumption (62%). In our cohort and regimen, MMPC significantly decreased in-hospital opioid consumption (62%). Soffin et al. examined the efficacy of MMPC including pre-incisional TAP block, regularly scheduled non-opioid analgesics (gabapentin, acetaminophen, ketorolac) for ALIF and lateral lumbar interbody fusion (LLIF) (36), which is similar to our study. They showed median MME was 57.5. The MMEs are much lower than those of our patients, which may be due to the difference in procedure. They evaluated patients undergoing ALIF/LLIF without posterior procedures whereas our patients all underwent posterior fusion. Also, their study did not have a control group, and sample size was small (n=32). In our study, we compared opioid consumption between MMPC and non-MMPC (control group) with relatively large size. Our finding provided a concrete evidence in the efficacy of MMPC regimen including TAP block.
There was no significant difference in the LOS in the present study. Meta-analysis of 11 prospective randomized clinical trials examining the efficacy of intramuscular local anesthetic infiltration prior to wound closure has shown that it significantly reduced postoperative opiate requirements, but did not reduce LOS after lumbar surgery (19). Brown et al. evaluated local infiltration of liposomal bupivacaine after lumbar fusion surgery and also found no reduction in LOS (28). On the contrary, Gianesello et al. reported that perioperative pregabalin administration after major spine surgery reduced LOS with less postoperative opioid consumption (32). It appears that a gastrointestinal complication due to opioids may affect the LOS; postoperative nausea, vomiting, and constipation were significantly less in the pregabalin group in their cohort, resulting in earlier postoperative up-site position, oral intake, and subsequent discharge. In our cohort, gastrointestinal complication was more common in the non-MMPC group, but the difference was not statistically significant, which may be related to the equivalent LOS in our study. Further evaluation with a larger sample size might be necessary to truly differentiate this as we feel clinically we have noticed a reduced number of these complications since we initiated the protocol.
Debate exists regarding the impact of MMPC on the hospital cost. Surgery-related materials such as implant and bone graft choices may influence cost more than MMPC (37). However, several studies reported that MMPC has a positive impact on the cost. Carr et al. compared the LOS and cost in major elective spine surgeries between traditional perioperative care and enhanced perioperative care including MMPC (38). They found that enhanced perioperative care decreased LOS and cost in major elective spine surgeries. A large part of difference in the cost was attributed to shorter hospital and intensive care unit stay. Similarly, in pediatric scoliosis surgery, preoperative patient education and MMPC have led to a decrease in LOS of 1.3 to 2 days and a 22% decrease in hospital cost (39,40). Another study revealed that postoperative intravenous acetaminophen is associated with shorter LOS, lower doses of opioids, and lower cost (31). In the present study, there was no difference in the cost, which may be due to less opioid-related complications in our cohort.
There are several limitations in this study. First, this is a retrospective study with a relatively small sample size. This is because we limited inclusion to patients undergoing single-level ALIF performed by a single surgeon. This type of study also limits the generalizability of these results. Conversely, a single-surgeon study can minimize the impact of difference in procedure and surgical skill. Second, some bias may be present. MMPC group was not blinded to surgeons, which might lead to less narcotics prescription in the group. Thirdly, we evaluated not chronic opioid dependence after discharge but in-hospital opioid consumption. Further research is necessary to see the downstream effects. Nonetheless, our findings are valuable as the amount of in-hospital opioid may have strong impact on the transition to chronic opioid use, especially in opioid naïve patients (6,7). Lastly, we only evaluated patients undergoing single-level ALIF. There are numerous spine surgery procedures and majority is posterior only approach. TAP block is not applicable for posterior only approach. Modification of protocol is necessary for posterior only procedures.
Conclusions
We examined the effect of an MMPC regimen in patients undergoing single-level ALIF for degenerative conditions. Our regimen significantly reduced in-hospital opioid consumption. An MMPC may reduce risk of opioid dependence as a greater amount of initial opioid exposure is associated with greater risks of long-term use.
Acknowledgments
A part of this study was presented in the annual meeting of the North American Spine Society 2020.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-629
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-629
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-629
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-629). Dr. JLG reports personal fees from Acuity, personal fees from Medtronic, personal fees from DePuy, personal fees from Alphatec, from Stryker, from Acuity, from K2M, from NuVasive, personal fees from Pfizer, outside the submitted work; Dr. CHC 3rd reports personal fees from Alphatec, personal fees from Medtronic, personal fees from NuVasive, personal fees from Alphatec, personal fees from Medtronic, personal fees from Titan, personal fees from SRS Committee, personal fees from NASS Committee, outside the submitted work; Dr. MD reports personal fees from Medtronic, personal fees from NuVasive, outside the submitted work; Dr. RKO 2nd reports personal fees from Medtronic, personal fees from NuVasive, grants from Pfizer, grants from Texas Scottish Rite Hospital, grants from Alan L. & Jacqueline B. Stuart Spine Research, grants from Cerapedics, grants from SRS, grants from Medtronic, grants from OREF, grants from ISSG, outside the submitted work; Dr. JRD 2nd reports personal fees from Medtronic, personal fees from DePuy, other from Federation Of Spine Association, other from SRS, personal fees from Pfizer, outside the submitted work; Dr. SDG reports personal fees from Medtronic, outside the submitted work; Dr. LYC reports personal fees from AO spine, personal fees from Center for Spine Surgery and Research of the University of Southern Denmark, personal fees from University of Louisville Institutional Review Board, grants from Scoliosis Research Society Research, grants from Orthopedic Educational Research Fund, grants from Integra, grants from Pfizer, personal fees from Pfizer, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Norton Healthcare (#18.1197) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Murthy VH. Ending the Opioid Epidemic - A Call to Action. N Engl J Med 2016;375:2413-5. [Crossref] [PubMed]
- Rudd RA, Aleshire N, Zibbell JE, et al. Increases in Drug and Opioid Overdose Deaths--United States, 2000-2014. MMWR Morb Mortal Wkly Rep 2016;64:1378-82. [Crossref] [PubMed]
- Clarke H, Soneji N, Ko DT, et al. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ 2014;348:g1251. [Crossref] [PubMed]
- Sun EC, Darnall BD, Baker LC, et al. Incidence of and Risk Factors for Chronic Opioid Use Among Opioid-Naive Patients in the Postoperative Period. JAMA Intern Med 2016;176:1286-93. [Crossref] [PubMed]
- Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg 2017;152:e170504. [Crossref] [PubMed]
- Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ 2018;360:j5790. [Crossref] [PubMed]
- Shah A, Hayes CJ, Martin BC. Factors Influencing Long-Term Opioid Use Among Opioid Naive Patients: An Examination of Initial Prescription Characteristics and Pain Etiologies. J Pain 2017;18:1374-83. [Crossref] [PubMed]
- Lee D, Armaghani S, Archer KR, et al. Preoperative Opioid Use as a Predictor of Adverse Postoperative Self-Reported Outcomes in Patients Undergoing Spine Surgery. J Bone Joint Surg Am 2014;96:e89. [Crossref] [PubMed]
- Zywiel MG, Stroh DA, Lee SY, et al. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am 2011;93:1988-93. [Crossref] [PubMed]
- Pivec R, Issa K, Naziri Q, et al. Opioid use prior to total hip arthroplasty leads to worse clinical outcomes. Int Orthop 2014;38:1159-65. [Crossref] [PubMed]
- Ben-Ari A, Chansky H, Rozet I.. Preoperative Opioid Use Is Associated with Early Revision After Total Knee Arthroplasty: A Study of Male Patients Treated in the Veterans Affairs System. J Bone Joint Surg Am 2017;99:1-9. [Crossref] [PubMed]
- Beverly A, Kaye AD, Ljungqvist O, et al. Essential Elements of Multimodal Analgesia in Enhanced Recovery After Surgery (ERAS) Guidelines. Anesthesiol Clin 2017;35:e115-43. [Crossref] [PubMed]
- Gritsenko K, Khelemsky Y, Kaye AD, et al. Multimodal therapy in perioperative analgesia. Best Pract Res Clin Anaesthesiol 2014;28:59-79. [Crossref] [PubMed]
- Dwyer AJ, Thomas W, Humphry S, et al. Enhanced recovery programme for total knee replacement to reduce the length of hospital stay. J Orthop Surg (Hong Kong) 2014;22:150-4. [Crossref] [PubMed]
- Machin JT, Phillips S, Parker M, et al. Patient satisfaction with the use of an enhanced recovery programme for primary arthroplasty. Ann R Coll Surg Engl 2013;95:577-81. [Crossref] [PubMed]
- Crisologo PA, Monson EK, Atway SA. Gabapentin as an Adjunct to Standard Postoperative Pain Management Protocol in Lower Extremity Surgery. J Foot Ankle Surg 2018;57:781-4. [Crossref] [PubMed]
- Farag E, Ghobrial M, Sessler DI, et al. Effect of perioperative intravenous lidocaine administration on pain, opioid consumption, and quality of life after complex spine surgery. Anesthesiology 2013;119:932-40. [Crossref] [PubMed]
- Garg N, Panda NB, Gandhi KA, et al. Comparison of Small Dose Ketamine and Dexmedetomidine Infusion for Postoperative Analgesia in Spine Surgery--A Prospective Randomized Double-blind Placebo Controlled Study. J Neurosurg Anesthesiol 2016;28:27-31. [Crossref] [PubMed]
- Perera AP, Chari A, Kostusiak M, et al. Intramuscular Local Anesthetic Infiltration at Closure for Postoperative Analgesia in Lumbar Spine Surgery: A Systematic Review and Meta-Analysis. Spine (Phila Pa 1976) 2017;42:1088-95. [Crossref] [PubMed]
- Jiang HL, Huang S, Song J, et al. Preoperative use of pregabalin for acute pain in spine surgery: A meta-analysis of randomized controlled trials. Medicine (Baltimore) 2017;96:e6129. [Crossref] [PubMed]
- Weiss AJ, Elixhauser A. Trends in Operating Room Procedures in U.S. Hospitals, 2001-2011: Statistical Brief #171. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US), 2006.
- Armaghani SJ, Lee DS, Bible JE, et al. Preoperative narcotic use and its relation to depression and anxiety in patients undergoing spine surgery. Spine (Phila Pa 1976) 2013;38:2196-200. [Crossref] [PubMed]
- Walid MS, Hyer L, Ajjan M, et al. Prevalence of opioid dependence in spine surgery patients and correlation with length of stay. J Opioid Manag 2007;3:127-8, 130-2. [Crossref] [PubMed]
- Dunn LK, Yerra S, Fang S, et al. Incidence and Risk Factors for Chronic Postoperative Opioid Use After Major Spine Surgery: A Cross-Sectional Study With Longitudinal Outcome. Anesth Analg 2018;127:247-54. [Crossref] [PubMed]
- Merchea A, Lovely JK, Jacob AK, et al. Efficacy and Outcomes of Intrathecal Analgesia as Part of an Enhanced Recovery Pathway in Colon and Rectal Surgical Patients. Surg Res Pract 2018;2018:8174579. [Crossref] [PubMed]
- Talboys R, Mak M, Modi N, et al. Enhanced recovery programme reduces opiate consumption in hip hemiarthroplasty. Eur J Orthop Surg Traumatol 2016;26:177-81. [Crossref] [PubMed]
- Niemelainen M, Kalliovalkama J, Aho AJ, et al. Single periarticular local infiltration analgesia reduces opiate consumption until 48 hours after total knee arthroplasty. A randomized placebo-controlled trial involving 56 patients. Acta Orthop 2014;85:614-9. [Crossref] [PubMed]
- Brown L, Weir T, Shasti M, et al. The Efficacy of Liposomal Bupivacaine in Lumbar Spine Surgery. Int J Spine Surg 2018;12:434-40. [Crossref] [PubMed]
- Bowman B, Sanchez L, Sarangarm P.. Perioperative Intravenous Acetaminophen in Pediatric Tonsillectomies. Hosp Pharm 2018;53:316-20. [Crossref] [PubMed]
- Cooke FE, Samuels JD, Pomp A, et al. A Randomized, Double-Blind, Placebo-Controlled Trial of Intravenous Acetaminophen on Hospital Length of Stay in Obese Individuals Undergoing Sleeve Gastrectomy. Obes Surg 2018;28:2998-3006. [Crossref] [PubMed]
- Hansen RN, Pham AT, Boing EA, et al. Comparative analysis of length of stay, hospitalization costs, opioid use, and discharge status among spine surgery patients with postoperative pain management including intravenous versus oral acetaminophen. Curr Med Res Opin 2017;33:943-8. [Crossref] [PubMed]
- Gianesello L, Pavoni V, Barboni E, et al. Perioperative pregabalin for postoperative pain control and quality of life after major spinal surgery. J Neurosurg Anesthesiol 2012;24:121-6. [Crossref] [PubMed]
- Khurana G, Jindal P, Sharma JP, et al. Postoperative pain and long-term functional outcome after administration of gabapentin and pregabalin in patients undergoing spinal surgery. Spine (Phila Pa 1976) 2014;39:E363-8. [Crossref] [PubMed]
- Carney J, McDonnell JG, Ochana A, et al. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg 2008;107:2056-60. [Crossref] [PubMed]
- Colibaseanu DT, Osagiede O, Merchea A, et al. Randomized clinical trial of liposomal bupivacaine transverse abdominis plane block versus intrathecal analgesia in colorectal surgery. Br J Surg 2019;106:692-9. [Crossref] [PubMed]
- Soffin EM, Freeman C, Hughes AP, et al. Effects of a multimodal analgesic pathway with transversus abdominis plane block for lumbar spine fusion: a prospective feasibility trial. Eur Spine J 2019;28:2077-86. [Crossref] [PubMed]
- Raudenbush BL, Gurd DP, Goodwin RC, et al. Cost analysis of adolescent idiopathic scoliosis surgery: early discharge decreases hospital costs much less than intraoperative variables under the control of the surgeon. J Spine Surg 2017;3:50-7. [Crossref] [PubMed]
- Carr DA, Saigal R, Zhang F, et al. Enhanced perioperative care and decreased cost and length of stay after elective major spinal surgery. Neurosurg Focus 2019;46:E5. [Crossref] [PubMed]
- Fletcher ND, Andras LM, Lazarus DE, et al. Use of a Novel Pathway for Early Discharge Was Associated With a 48% Shorter Length of Stay After Posterior Spinal Fusion for Adolescent Idiopathic Scoliosis. J Pediatr Orthop 2017;37:92-7. [Crossref] [PubMed]
- Sanders AE, Andras LM, Sousa T, et al. Accelerated Discharge Protocol for Posterior Spinal Fusion Patients With Adolescent Idiopathic Scoliosis Decreases Hospital Postoperative Charges 22. Spine (Phila Pa 1976) 2017;42:92-7. [Crossref] [PubMed]


