Symptomatic pseudarthrosis requiring revision surgery after 1- or 2-level ACDF with plating: peek versus allograft
Introduction
Cervical spondylosis may present with a combination of neck pain, radiculopathy, and/or myelopathy. Any of these manifestations can impair a patient’s quality of life. Anterior cervical discectomy and fusion (ACDF) is the conventional surgical treatment when non-operative measures have failed to improve the patient’s symptoms (1-4). ACDF involves removing the intervertebral disc and fusing the adjacent vertebrae to stabilize the diseased segment(s). An interbody spacer (artificial or biologic) can be placed between the vertebrae, providing structural support, and serving as a fusion substrate scaffold. Smith and Robinson first described the ACDF procedure (4). They advocated iliac crest autograft as the interbody graft material, but this has been shown to be associated with donor site morbidity such as pain and infection (5). Interbody implants have been designed to avoid these complications while maintaining good fusion rates and clinical outcomes. Commonly used materials include allograft bone, metal, and polyetheretherketone (PEEK) (6). A number of studies have been performed to describe and compare the clinical efficacy of these materials (7-9). Most of these studies compared titanium to PEEK spacers. There are some regional preferences in interbody devices of choice—PEEK is most commonly used in Europe but allograft is more commonly used in the United States (6). There is a scarcity of literature showing a head to head comparison of PEEK and allograft spacers in the context of ACDF surgery and the incidence of postoperative symptomatic pseudarthrosis (10).
The aim of this study was to compare the clinical outcomes of PEEK and allograft spacers in ACDF surgery with respect to the incidence of symptomatic pseudarthrosis requiring revision surgery. Symptomatic pseudarthrosis included patients with radiographic signs of pseudarthrosis at a minimum of 6 months post-operatively with new or recurrent clinical symptoms.
Methods
Subjects and surgery
We retrospectively reviewed patients who underwent 1- or 2-level ACDF at a single spine center from January 2010 to December 2014. Subjects who had more than a 2-level ACDF, prior cervical spine surgery, local/systemic infection, neoplasm, or cervical trauma were excluded. Patients who were under 18 or over 70 years old or who did not consent to research were also excluded from this study. Patients requiring revision surgery for other reasons (e.g., adjacent segment level disease and kyphosis) were not included. This study was approved by the Allina Health Institutional Review Board (1046904-2) under Expedited review category #5, with a waiver of consent granted. Study outcomes will not affect the future management of the patients. Patients’ personal data have been secured for subject privacy.
All surgeries were performed under general anesthesia, by a left sided Smith-Robinson approach. After removal of the disc and decompression of neural structures, an interbody spacer was placed, either an allograft or PEEK cage. The type of spacer was based on surgeon’s preference. The graft or cage was sized to as much as possible fill the space between the uncinate processes and between the anterior and posterior edges of the endplates. A combination of locally harvested autograft and cancellous allograft chips was used in both PEEK and allograft interbody groups to augment fusion. In some cases, demineralized bone matrix (DBM) was added as a graft extender. Anterior plates and screws were used in all cases. Patients were discharged within 24–48 hours after surgery. A soft collar was used for comfort for 2 to 4 weeks following surgery. Revision surgery for patients with symptomatic pseudarthrosis is typically posterior instrumented fusion with local autograft with or without allograft at our practice.
Clinical evaluation
Clinical outcomes were evaluated using the Neck Disability Index (NDI) and Visual Analogue Scale (VAS) for neck and arm pain. Patient charts were reviewed for subsequent anterior or posterior cervical spine surgery.
Radiographic evaluation
Anterior-posterior and lateral radiographs of the cervical spine were taken at 1-, 3-, 6-, 12-, and 24-month postoperatively. The intervertebral heights of the operative segments were measured at immediate postoperative follow-up and at last follow-up. Subsidence was defined as a decrease in the intervertebral height of 2 mm or more between the immediate postoperative and final postoperative radiographs. Patients with inadequate radiographic follow-up were excluded from radiographic analyses. A computed tomography (CT) scan was performed on all patients suspected to have a pseudarthrosis. Pseudarthrosis was defined as no bridging bone seen across the intervertebral space and/or radiolucency between the spacer and an adjacent vertebral body.
Data source
Data were extracted from the patients’ electronic health records within our local hospital.
Statistical analysis
Subjects were divided into two cohorts, allograft and PEEK, to compare demographics, functional outcomes, reoperation rates, and subsidence. Data were analyzed using SPSS 12.0 (SPS, Inc., Chicago, IL, USA). Statistical tests included chi-square or Fisher’s exact tests for categorical variables and Student’s t-tests and paired t-tests for continuous variables. Two multinomial logistic regression analyses were conducted with material (allograft or PEEK) and number of levels (1 or 2) as independent categorical variables and dependent outcomes of pseudarthrosis or subsidence. The threshold for statistical significance was P=0.05. Additional statistical analyses on functional outcomes, plate type and graft type were conducted by dividing subjects into cohorts according to subsidence or pseudarthrosis.
Results
Subjects and surgery
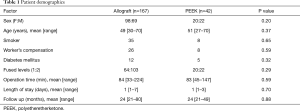
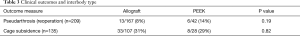
A total of 209 patients (91 males and 118 females) who met the selection criteria with a 21-month minimum follow up were analyzed. Median follow-up was 24 months in the allograft group (range 21 to 80) and 24 months in the PEEK group (range 21 to 49). One hundred and sixty-seven patients had an allograft spacer and 42 patients had a PEEK spacer. There was no significant difference in demographics, smoking status, or workers compensation status between the two groups (Table 1). All patients received anterior plates and screws.
Full table
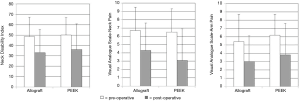
Clinical outcomes
Patients improved significantly when comparing index preoperative and final follow-up NDI, VAS-neck, and VAS-arm (P<0.01, P<0.01, and P=0.02, respectively). Allograft and PEEK cohorts were not statistically different with respect to improvements in patient-reported outcomes (Figure 1). The proportions of patients who achieved minimal clinically important difference (MCID) in patient-reported outcomes were not different between cohorts (Table 2).

Full table
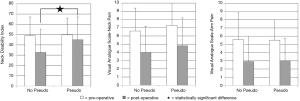
Reoperations
The rate of revision surgery for pseudarthrosis was 8% (13/167) in the allograft group and 14% (6/42) in PEEK patients; this difference was not statistically significant (P=0.19) (Table 3). Pseudarthrosis rate was not significantly different between 1- and 2-level surgeries with respect to interbody material type (allograft or PEEK) and number of levels (1 or 2) (P=0.07). In allograft bone cases, there was a trend toward more pseudarthrosis in 2-level cases, but this was not significant (P=0.06, Pearson’s correlation coefficient). Patients who developed symptomatic pseudarthrosis had significantly less function (higher NDI scores) at final follow-up compared to asymptomatic patients (P=0.02) (Figure 2). However, this difference was not observed in the VAS-neck and VAS-arm. The proportions of patients who achieved MCID in patient-reported outcomes were not different (Table 4).
Full table

Full table
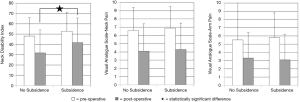
Radiographic outcomes
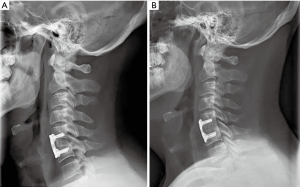
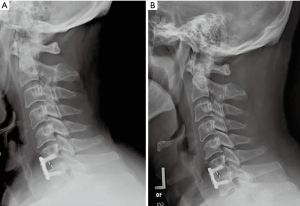
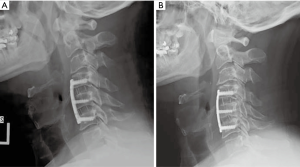
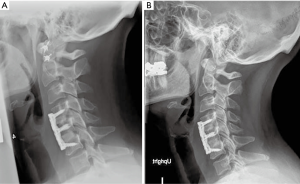
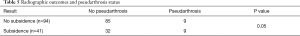
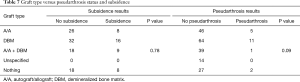
Of the 209 patients included in the study, 135 had radiographs that allowed measurement of subsidence with a minimum 1 year follow up. Figures 3-6 depict typical examples of radiographic outcomes. The rates of subsidence were 31% in the allograft group and 29% among the PEEK patients (Table 3). This difference was not statistically significant (P=0.82). Subsidence and pseudarthrosis trended together, but there was no statistically significant association between clinical outcomes and subsidence (Table 5). Subsidence was not significantly different between 1- and 2-level surgeries with respect to interbody material type (allograft or PEEK) and number of levels (1 or 2) (P=0.65). Patients who developed subsidence had a significantly less function (higher NDI scores) at final follow-up compared to asymptomatic patients (P=0.01). However, this difference was not observed in the VAS-neck and VAS-arm (Figure 7). The proportions of patients who achieved MCID in patient-reported outcomes were not different (Table 6). There were five groups for grafting technique (Table 7). There were no differences in subsidence or reoperation for according to graft type. There were no differences in subsidence or reoperations between the allograft and PEEK cohorts with respect to plate manufacturer (data not shown).
Full table

Full table
Full table
Discussion
Allograft and PEEK are the most commonly used spacers for ACDF surgery (11). Good and excellent outcomes have been reported for both (12-14). However, Krause et al. reported a lower rate of pseudarthrosis among allograft patients compared to PEEK in 1-level ACDF (10). Likewise, Pirkle et al. reported a higher union rate with allograft compared to other cages such as PEEK, titanium and porous mesh metal (9). The current study is in concordance with the above trends: revision surgery for pseudarthrosis was 8% for allograft bone and 14% for PEEK, however, this difference was not statistically significant.
Pseudarthrosis is not an uncommon complication of ACDF surgery. However, it is not routinely symptomatic and as such can be deemed ‘stable’ and not require revision surgery. The reported incidence of pseudarthrosis was reported as high as 20% and 50% for single and multilevel ACDF, respectively (15-18). Phillips et al. reported poor clinical outcomes in the majority of patients with pseudarthrosis, 67% of whom required revision surgery (19). Similarly, Buttermann et al. reported poor outcomes in patients with pseudarthrosis in a 10+ year prospective study. Reported revision surgery for pseudarthrosis repair was performed in 10% of patients—most often within 2 years of the primary surgery (2).
In this study, revision surgery for pseudarthrosis was 8% for allograft bone and 14% for PEEK spacers in 1- or 2-level ACDF. These results are comparable to the literature. Reoperation rates for pseudarthrosis was almost twice as high in the PEEK group compared to allograft, though this was not statistically significant. Nonetheless, revision surgery for any reason may be considered to be clinically significant. Patients needing a revision do not do as well functionally as those who do not receive a revision. As such, this information could be useful in clinical practice and surgeons will want to be aware of the potentially higher revision rate for PEEK.
The reported subsidence rates of different intervertebral spacers in ACDF surgery range from 0% to 48% (20,21). Yson et al. compared allograft and PEEK cages and found subsidence rates of 28% and 29%, respectively (22). Cabraja et al. compared titanium and PEEK cages and found subsidence rates of 20.5% and 14.3%, respectively (7). The literature shows that the type of intervertebral spacer might not be the only factor that affects subsidence rates. Other factors such as implant geometry, distraction during surgery, cervical alignment, age, surgical technique and use of plates may also play a role (23-25). It is not clear if subsidence is only a radiographic finding, or if it adversely affects clinical outcomes. While some studies reported worse clinical outcomes with subsidence, others have shown no correlation between subsidence and clinical outcomes (22,26-29). In the current study, subsidence was associated with worse functional outcomes (post-operative NDI scores were statistically higher for patients with subsidence). Karikari et al., in a meta-analysis of 35 articles, concluded that the type of implant did not affect the subsidence rate. They also found that neither clinical outcomes nor fusion rates were affected by subsidence (30). In this study, the subsidence rate was 29% for PEEK and 31% for allograft, which is concordant with the literature.
We found that the symptomatic pseudarthrosis rate was not different between 1- and 2-level surgeries. Veeravagu et al. reported that the rate of reoperations increases with increasing number of levels fused (31). The reasons for the difference between their study and ours may be that we included only reoperations for symptomatic pseudarthrosis and only considered allograft and PEEK as interbody materials. Veeravagu did not differentiate for interbody type or reasons for reoperation. Likewise, we found that subsidence did not depend on the number of levels. Our result agrees with Lin et al. (14). They found no difference in subsidence between 1-, 2-, and 3-level reconstructions among ACDF procedures using a PEEK interbody cage.
Limitations to this study include those inherent of any retrospective review. However, given the paucity of data regarding this topic this represents the first step towards a higher level study (randomized prospective trial) to answer the research question of which spacer option has a higher association with symptomatic pseudarthrosis following 1- or 2-level ACDF. Secondly, the disproportion sample sizes (allograft, 167 patients, and PEEK, 42 patients) may have an effect on the results. We note, however, that this disparity mirrors North American surgeon preferences for allograft over PEEK (6). Third, we studied only symptomatic pseudarthrosis. Other important diagnoses that may require revision surgery (e.g., adjacent segment level disease and kyphosis) are not included (11). Fourth, all of our subjects were plated. Therefore, we are unable to study this as a factor. However, the question “to plate or not to plate” has been the considerably discussed elsewhere in the literature (32). Finally, differences in surgical techniques have the potential to affect outcomes. The projected effects of these technical differences on fusion and symptomatic pseudarthrosis are difficult to assess given the nature of the study. A future prospective study by a single surgeon, comparing both PEEK and allograft with equal number of patients in each group could yield more definitive conclusions to the research question.
Conclusions
This study analyzed allograft and PEEK ACDF spacers with regards to clinical outcome (NDI, VAS-neck, VAS-arm), radiographic measurement (subsidence), and revision rate for symptomatic pseudarthrosis. Both allograft and PEEK interbody spacer showed similar improvement in clinical outcomes following index ACDF surgery. Patients with pseudarthrosis requiring revision surgery had lower functional outcomes. Subsidence rates were similar between allograft and PEEK. Patients with subsidence had lower functional outcomes. Reoperation rates for symptomatic pseudarthrosis following index 1- or 2-level ACDF was higher in the PEEK interbody group, but this was not statistically significant.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-19-419). AAM reports personal fees from Stryker, personal fees from Zimmer, outside the submitted work; TAG reports personal fees from Medtronic, outside the submitted work; JDS reports personal fees from Medtronic, personal fees from Stryker, outside the submitted work; The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Allina Health Institutional Review Board (1046904-2) under Expedited review category #5, with a waiver of consent granted. Study outcomes will not affect the future management of the patients. Patients’ personal data have been secured for subject privacy.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bohlman HH, Emery SE, Goodfellow DB, et al. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 1993;75:1298-307. [Crossref] [PubMed]
- Buttermann GR. Anterior cervical discectomy and fusion outcomes over 10 years: a prospective study. Spine (Phila Pa 1976) 2018;43:207-14. [Crossref] [PubMed]
- Li J, Zheng Q, Guo X, et al. Anterior surgical options for the treatment of cervical spondylotic myelopathy in a long-term follow-up study. Arch Orthop Trauma Surg 2013;133:745-51. [Crossref] [PubMed]
- Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607-24. [Crossref] [PubMed]
- Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2003;28:134-9. [Crossref] [PubMed]
- Yoon ST, Konopka JA, Wang JC, et al. ACDF graft selection by surgeons: survey of AOSpine members. Global Spine J 2017;7:410-6. [Crossref] [PubMed]
- Cabraja M, Oezdemir S, Koeppen D, et al. Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord 2012;13:172. [Crossref] [PubMed]
- Niu CC, Liao JC, Chen WJ, et al. Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech 2010;23:310-6. [Crossref] [PubMed]
- Pirkle S, Kaskovich S, Cook DJ, et al. Cages in ACDF are associated with a higher nonunion rate than allograft: A stratified comparative analysis of 6130 patients. Spine (Phila Pa 1976) 2019;44:384-8. [Crossref] [PubMed]
- Krause KL, Obayashi JT, Bridges KJ, et al. Fivefold higher rate of pseudarthrosis with polyetheretherketone interbody device than with structural allograft used for 1-level anterior cervical discectomy and fusion. J Neurosurg Spine 2018;30:46-51. [Crossref] [PubMed]
- van Eck CF, Regan C, Donaldson WF, et al. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine (Phila Pa 1976) 2014;39:2143-7. [Crossref] [PubMed]
- Cho DY, Liau WR, Lee WY, et al. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery 2002;51:1343-9; discussion 1349-50. [Crossref] [PubMed]
- Grossman W, Peppelman WC, Baum JA, et al. The use of freeze-dried fibular allograft in anterior cervical fusion. Spine (Phila Pa 1976) 1992;17:565-9. [Crossref] [PubMed]
- Lin HL, Cho DY, Liu YF, et al. Change of cervical balance following single to multi-level interbody fusion with cage. Br J Neurosurg 2008;22:758-63. [Crossref] [PubMed]
- Bolesta MJ, Rechtine GR 2nd, Chrin AM. One- and two-level anterior cervical discectomy and fusion: the effect of plate fixation. Spine J 2002;2:197-203. [Crossref] [PubMed]
- Brodke DS, Zdeblick TA. Modified Smith-Robinson procedure for anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 1992;17:S427-30. [Crossref] [PubMed]
- Cannada LK, Scherping SC, Yoo JU, et al. Pseudarthrosis of the cervical spine: a comparison of radiographic diagnostic measures. Spine (Phila Pa 1976) 2003;28:46-51. [Crossref] [PubMed]
- Emery SE, Fisher JR, Bohlman HH. Three-level anterior cervical discectomy and fusion: radiographic and clinical results. Spine (Phila Pa 1976) 1997;22:2622-4. [Crossref] [PubMed]
- Phillips FM, Carlson G, Emery SE, et al. Anterior cervical pseudarthrosis. Natural history and treatment. Spine (Phila Pa 1976) 1997;22:1585-9. [Crossref] [PubMed]
- Feng SW, Chang MC, Chou PH, et al. Implantation of an empty polyetheretherketone cage in anterior cervical discectomy and fusion: a prospective randomised controlled study with 2 years follow-up. Eur Spine J 2018;27:1358-64. [Crossref] [PubMed]
- Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138-44. [Crossref] [PubMed]
- Yson SC, Sembrano JN, Santos ER. Comparison of allograft and polyetheretherketone (PEEK) cage subsidence rates in anterior cervical discectomy and fusion (ACDF). J Clin Neurosci 2017;38:118-21. [Crossref] [PubMed]
- Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J 2007;16:1395-400. [Crossref] [PubMed]
- Lee YS, Kim YB, Park SW. Risk factors for postoperative subsidence of single-level anterior cervical discectomy and fusion: the significance of the preoperative cervical alignment. Spine (Phila Pa 1976) 2014;39:1280-7. [Crossref] [PubMed]
- Truumees E, Demetropoulos CK, Yang KH, et al. Effects of disc height and distractive forces on graft compression in an anterior cervical discectomy model. Spine (Phila Pa 1976) 2002;27:2441-5. [Crossref] [PubMed]
- Chen Y, Wang X, Lu X, et al. Comparison of titanium and polyetheretherketone (PEEK) cages in the surgical treatment of multilevel cervical spondylotic myelopathy: a prospective, randomized, control study with over 7-year follow-up. Eur Spine J 2013;22:1539-46. [Crossref] [PubMed]
- Kast E, Derakhshani S, Bothmann M, et al. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev 2009;32:207-14; discussion 214. [Crossref] [PubMed]
- Lee CH, Kim KJ, Hyun SJ, et al. Subsidence as of 12 months after single-level anterior cervical inter-body fusion. Is it related to clinical outcomes? Acta Neurochir (Wien) 2015;157:1063-8. [Crossref] [PubMed]
- Wu WJ, Jiang LS, Liang Y, et al. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J 2012;21:1374-82. [Crossref] [PubMed]
- Karikari IO, Jain D, Owens TR, et al. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech 2014;27:1-10. [Crossref] [PubMed]
- Veeravagu A, Cole T, Jiang B, et al. Revision rates and complication incidence in single- and multilevel anterior cervical discectomy and fusion procedures: an administrative database study. Spine J 2014;14:1125-31. [Crossref] [PubMed]
- Oliver JD, Goncalves S, Kerezoudis P, et al. Comparison of outcomes for anterior cervical discectomy and fusion with and without anterior plate fixation: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2018;43:E413-22. [Crossref] [PubMed]