
Surgical correction of rigid cervicothoracic deformity in a transgender patient: case report
Introduction
The cervical spine is an essential anatomic structure that protects neurologic elements and is fundamental for maintenance of horizontal gaze. Normal alignment of the cervical spine, particularly in the sagittal plane, is imperative for normal physiologic function and low muscle energy expenditure. Cervicothoracic kyphosis is a spinal condition which moves the center of gravity anteriorly, resulting in increased energy expenditure and decreased ability to maintain horizontal gaze. Furthermore, this may result in cervical myelopathy secondary to spinal cord stretching and alteration in microcirculation (1). Spondyloarthropathies, such as ankylosing spondylitis, can result in anomalous fusion of the spine and is a potential etiology for spinal deformity, resulting in significant patient morbidity and impact on overall quality of life.
Due to inflammatory processes that first affect the facet joints, patients with ankylosing spondylitis begin to flex their spine to offload contact pressures. Bridging of syndesmophytes occur, eventually leading to ankylosis and the characteristic bamboo spine appearance on radiographs (2,3). This eventually leads to patients developing a fixed kyphotic deformity that is largely centered at the cervicothoracic and thoracolumbar junctions (4). In an attempt to compensate for the deformity, patients flex their knees and extend their hips to restore horizontal gaze, though this requires profound energy expenditure and cannot be sustained for prolonged periods of time (5). Several radiographic measures are used to measure and monitor the cervicothoracic deformity, including the Chin-Brow vertical angle (CBVA), the C2–C7 sagittal vertical axis (SVA), and C2–C7 angle (6). We report a unique surgical case of spondyloarthropathy affecting the posterior spinal elements only, resulting in severe chin-on-chest deformity in a transgender patient. The authors present the case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-584).
Case presentation
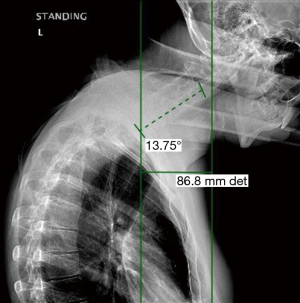
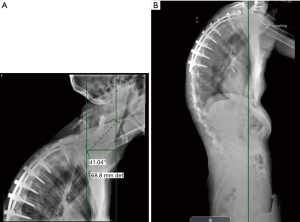
The patient is a 26-year-old transgender female (male to female) with progressive kyphotic cervicothoracic deformity due to spinal fusion of posterior elements only (Figure 1). As a child, she underwent Nuss bar placement for pectus excavatum, and this was subsequently removed. She was found to be HLA-B27 positive and was being treated with adalimunab. For her gender transition, she was being treated with high dose estrogens and anti-androgens. She did undergo pre-operative bone health evaluation and was found to have a lumbar Z score of −0.1. Clinically, she demonstrated a near chin on chest deformity with a rigid, fixed kyphotic deformity (Figure 2). She was very unhappy with her inability to look straight ahead. Imaging demonstrated a C2–C7 SVA of 8.7 cm and a C2 to C7 angle of 13.7 degrees (Figures 3,4). After exhausting non-operative treatment, and after extensive discussions about surgical correction and the associated risks with her, as well as her rheumatologist and family, surgical intervention was agreed upon. She underwent a C2–T8 posterior spinal fusion with a T3 pedicle subtraction osteotomy (PSO) and C3–7 cervical facet osteotomies. This location was chosen as the optimal osteotomy location as it was felt to be the apex of the deformity and thus provided the site for the largest correction of her deformity. In briefly reviewing the various types of osteotomies, we felt the PSO would provide the largest correction per level. In the PSO a closing wedge osteotomy of the vertebral body occurs with extension through the pedicle. This is held in place with dorsal spinal instrumentation. Uniquely, thoracic pedicle subtraction osteotomies, such as hers, often require partial rib resections (Figure 5).

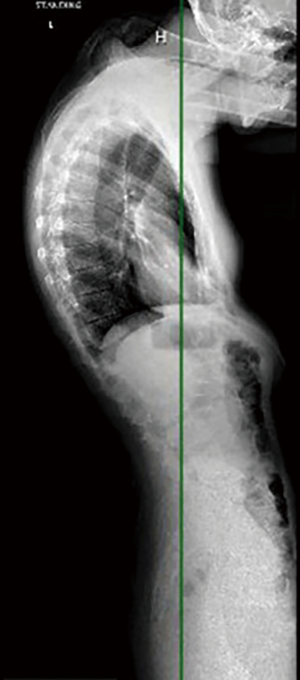

She had no intraoperative complications and was very happy with her postoperative outcome and restoration of horizontal gaze. However, she did require a Dubroff tube for feeding due to severe dysphagia (Figure 6). Nutritionist was consulted and optimized her intake to ensure adequate nutrients. By her 3-month post-operative visit, this was removed and she was able to tolerate oral intake well. By her 1-year post-operative visit, she was performing activities she enjoyed without restrictions, though she did report occasional muscular aches, and reported an improved quality of life. Postoperative 1-year imaging is shown in (Figure 7). There were substantial improvements in the C2–C7 SVA and C2–C7 angle, as well as her global alignment.

Consent was obtained from this patient for publication of this case report.
Discussion
Ankylosing spondylitis (AS) is a systemic inflammatory disease that predominately affects the axial skeleton leading to pain, deformity, and in some instances neurological deficits (2,7-9). Deformity of the spine can occur in all regions of the spine, though the kyphotic deformity of the cervical spine is poorly tolerated due to inability to maintain a horizontal gaze. AS is primarily seen in white males of non- Asian/African heritage (7,9). Symptoms begin to develop in most patients when they are in their twenties. While there is no single known cause of the disease there, 90% of patients with AS are found to be positive for Human Leukocyte Antigen subtype B-27 (HLA-B27) (7,10). Attempts at understanding the role that androgens play in the pathogenesis of AS is not yet fully elucidated, but there is belief that men have more severe disease, and faster progression of the disease (11-13).
This case report is the first to report correction of complex deformity in a transgender patient. Many studies have demonstrated low bone mass in trans-women and recommend pre-operative bone health evaluations when patients have elevated risk factors. These risk factors include; initiation/termination of hormone therapy especially post gonadectomy, prior fragility fracture, and low levels of vitamin D (14-16). It is imperative to evaluate bone health in this patient population prior to deformity correction to identify any underlying metabolic abnormality that may affect bone density. Evidence regarding rates and risk factors of spinal fusion in patients on hormone replacement or therapy is lacking and a focus for future research.
Goals for successful correction of cervical kyphosis are maintenance of comfortable horizontal gaze, decompression of neurological elements, and stable fusion of the head aligned with the pelvis. Once the location of the osteotomy is chosen, a standard dorsal approach to the spine is performed. Once the spine is exposed the authors prefer to utilize intra-operative navigation to place pedicle screws or lateral mass screws cranial and caudal to the osteotomy site. Hardware is not placed at the intended osteotomy site. A complete laminectomy is performed, along with removal of the superior articulating facet and inferior articulating facet. The exposed pedicle remains intact and is decancellated using a burr. From this decancellated pedicle the vertebral body is decancellated, and eventually the pedicle is amputated at the pedicle body junction. Using a Woodson or similar tool, a plane is established between the remaining body and the spinal cord. The cortex of the body is impacted into the decancellated portion of the vertebral body, creating a defect just anterior the spinal cord. Under direct visualization the defect in the body is closed, ensure no kinking of the cord. In the thoracic spine the ribs are partially removed, to allow for closure of the vertebral body defect. If they are not removed, they prevent closure of the osteotomy site. This closure is held in place with the instrumentation that was placed prior to the osteotomy.
A number of complications may occur following complex cervical deformity correction, including infection, new neurologic deficit, nonunion, or distal junctional kyphosis. One of the most common and most debilitating, however, is dysphagia. It is imperative to counsel patients about this preoperatively. Due to the severity of the kyphotic deformity in patients undergoing major cervical surgery, many already have baseline subclinical swallowing dysfunction (17). It is important to established baseline level of function with evaluation by an otolaryngologist, especially if patients have any complaints of dysphagia preoperatively. Post-operatively many patients report clinically significant dysphagia, and there should be a low threshold for multi-disciplinary approach with speech language pathology and nutritional consult to assess safe swallowing and metabolic needs to aid in bone healing (18,19).
Conclusions
Cervicothoracic deformity is a complex pathology resulting in significant patient morbidity and decreased quality of life. Surgical correction aims to restore sagittal alignment but has a high complication profile. Patients must be warned that complications are likely, though severity can vary from trouble swallowing to neurological compromise (20,21). Our patient presented a number of unique challenges, including a complex rigid cervicothoracic deformity in the context of posterior spinal element fusion only. While posterior elements of the spine are normally affected first in spondyloarthropathies such as ankylosing spondylitis, the lack of anterior spinal involvement is unique and could be attributed to hormonal therapy in this patient. Alternatively, this may be a unique pattern of spinal fusion not yet completely described in the literature.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-584).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/jss-20-584). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Consent was obtained from this patient for publication of this case report.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tan LA, Riew KD, Traynelis VC. Cervical Spine Deformity-Part 1: Biomechanics, Radiographic Parameters, and Classification. Neurosurgery 2017;81:197-203. [Crossref] [PubMed]
- Kubiak EN, Moskovich R, Errico TJ, et al. Orthopaedic management of ankylosing spondylitis. J Am Acad Orthop Surg 2005;13:267-78. [Crossref] [PubMed]
- van Tubergen A, van der Heijde D, Dougados M, et al. Are syndesmophytes most prevalent in the lumbar or in the cervical spine in patients with ankylosing spondylitis and do they develop in a specific direction? Rheumatology (Oxford) 2012;51:1432-9. [Crossref] [PubMed]
- Ankylosing Spondylitis and Related Disorders in Benzel's Spine Surgery. In: Benzel EC (ed). Spine Surgery. Philadelphia: 2017, Elsevier.
- Moses MJ, Tishelman JC, Zhou PL, et al. McGregor's slope and slope of line of sight: two surrogate markers for Chin-Brow vertical angle in the setting of cervical spine pathology. Spine J 2019;19:1512-7. [Crossref] [PubMed]
- Simmons EH. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop Relat Res 1977.65-77. [PubMed]
- Olivieri I, van Tubergen A, Salvarani C, et al. Seronegative spondyloarthritides. Best Pract Res Clin Rheumatol 2002;16:723-39. [Crossref] [PubMed]
- Braun J, Sieper J. Ankylosing spondylitis. Lancet 2007;369:1379-90. [Crossref] [PubMed]
- Dean LE, Jones GT, MacDonald AG, et al. Global prevalence of ankylosing spondylitis. Rheumatology (Oxford) 2014;53:650-7. [Crossref] [PubMed]
- Feldtkeller E, Khan MA, van der Heijde D, et al. Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis. Rheumatol Int 2003;23:61-6. [Crossref] [PubMed]
- Masi AT. Do sex hormones play a role in ankylosing spondylitis?. Rheum Dis Clin North Am 1992;18:153-76. [PubMed]
- Aydin T, Karacan I, Demir SE, et al. Bone loss in males with ankylosing spondylitis: its relation to sex hormone levels. Clin Endocrinol (Oxf) 2005;63:467-9. [Crossref] [PubMed]
- Gooren LJ, Giltay EJ, van Schaardenburg D, et al. Gonadal and adrenal sex steroids in ankylosing spondylitis. Rheum Dis Clin North Am 2000;26:969-87. [Crossref] [PubMed]
- Rothman MS, Iwamoto SJ. Bone Health in the Transgender Population. Clin Rev Bone Miner Metab 2019;17:77-85. [Crossref] [PubMed]
- Van Caenegem E. TʼSjoen G. Bone in trans persons. Curr Opin Endocrinol Diabetes Obes 2015;22:459-66. [Crossref] [PubMed]
- Wiepjes CM, de Blok CJ, Staphorsius AS, et al. Fracture Risk in Trans Women and Trans Men Using Long-Term Gender-Affirming Hormonal Treatment: A Nationwide Cohort Study. J Bone Miner Res 2020;35:64-70. [Crossref] [PubMed]
- Iyer S, Kim HJ, Bao H, et al. Cervical Deformity Patients Have Baseline Swallowing Dysfunction but Surgery Does Not Increase Dysphagia at 3 Months: Results From a Prospective Cohort Study. Global Spine J 2019;9:532-9. [Crossref] [PubMed]
- Klein JD, Hey LA, Yu CS, et al. Perioperative nutrition and postoperative complications in patients undergoing spinal surgery. Spine (Phila Pa 1976) 1996;21:2676-82. [Crossref] [PubMed]
- Hu SS, Fontaine F, Kelly B, et al. Nutritional depletion in staged spinal reconstructive surgery. The effect of total parenteral nutrition. Spine (Phila Pa 1976) 1998;23:1401-5. [Crossref] [PubMed]
- Daubs MD, Brodke DS, Annis P, et al. Perioperative Complications of Pedicle Subtraction Osteotomy. Global Spine J 2016;6:630-5. [Crossref] [PubMed]
- Choi HY, Hyun SJ, Kim KJ, et al. Radiographic and Clinical Outcomes Following Pedicle Subtraction Osteotomy: Minimum 2-Year Follow-Up Data. J Korean Neurosurg Soc 2020;63:99-107. [Crossref] [PubMed]



