MRI based analysis of grade of spinal canal stenosis and grade of compression of nerve root by lumbar disc herniation as tools to predict probability to need surgical treatment
Introduction
Lumbar disc herniations (LDHs) are mostly treated non-operatively. Indications for immediate surgery are cauda equina syndrome and progressive or high-grade motor deficit. Patients with a LDH without indication for immediate surgical treatment (PWN) and unsuccessful conservative treatment receive postponed surgical treatment (1-4). Postponed surgery is reported to lead to significant later return to work and later improvement of radicular pain and health-related quality of life than early surgery (1,2,4).
There are currently no objective parameters in the literature that may help to determine if non-operative treatment in PWN will be successful or if they will eventually be treated surgically. If those patients who will eventually need surgery could be distinguished from those who will not need surgery, they could be offered an early surgical intervention and benefit from faster recovery, earlier return to work and shorter duration of administration of pain medication.
Identifying these patients by imaging has been shown to be difficult: imaging of the lumbar spine did not show any correlation with clinical symptoms in several reports (5-7).
However, there are some investigations that report that morphology and size of LDH may have an impact on clinical symptoms: Thelander et al. (8) reported a correlation of size of LDH with radicular pain. Carragee et al. (9) reported a correlation of size of LDH and size of spinal canal with presence of radicular pain and time of pain before a MRI scan was conducted: patients with a larger size of LDH had a shorter duration of symptoms before the MRI, i.e., received a MRI earlier after onset of symptoms. Carlisle et al. (10) reported a positive correlation of volume of LDH with probability to receive operative treatment.
Nevertheless, there is still no data on impact of morphologic parameters of LDH on probability to be operated for PWI. Carlisle et al. (10) and Carregee et al. (9) compared all patients with LDH who received surgery to patients who were treated non-operatively. Patients with an indication for immediate surgery (e.g., cauda equina syndrome or high-grade motor deficit) were included in these investigations. Thelander et al. (8) reported exclusively on patients that have not been operated. Carragee et al. (9) did not exclude patients with chronical pain syndrome and did not differentiate between acute or chronical pain. Thus, these studies provide very important data for patients with LDH in general, but data of PWI with regard to probability of operative treatment are obscured in these results.
A grading system of nerve root compromise by LDH was established by Pfirrmann et al. (11) (shifted, deviated or compressed). However, the influence of grade of nerve root compromise on the success of conservative treatment of PWI has yet not been investigated.
Methods
We retrospectively included patients with radicular pain or neurologic deficit that matched the affected level and side in the patient’s MRI, acute onset of pain (less than 6 weeks before admission to our institution) and in whom a MRI was performed after onset of the pain that led to the admission to our institution from 02.2008 to 12.2017 in a single-center study. All patients received the same intravenous pain medication according to step 3 of the WHO pain ladder. Patients who showed improvement of their pain (VAS <8) were not given inpatient treatment and were excluded.
We also excluded patients younger than 18 or older than 65 years, with a neurological deficit <3/5 according to Janda, with workers’ compensation involvement, chronic pain syndrome, with a spinal deformity, malignancy, history of prior spinal surgery, currently treated by effective anticoagulation and patients with other contraindications for surgical treatment because of medical conditions.
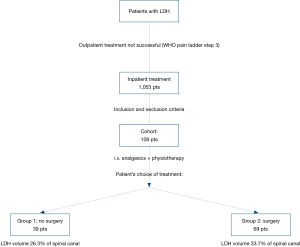
Power analysis was based on data of previous studies on volume of LDH (8,10) and showed that at least 35 patients were needed in each group to reach a high statistical power (>0.8). We identified 1,053 consecutive patients who received inpatient treatment of a LDH in our institution from 02.2008 to 12.2017 by diagnostic code. After applying inclusion and exclusion criteria we enrolled 108 patients in our analysis. Thirty-nine patients were treated non-operatively (Group 1), 69 were treated by operation (Group 2) (Figure 1).
All included patients were treated non-operatively by the same protocol: they received the same dosage of intravenous analgesics (tramadol and metamizole) and the same type and frequency of physiotherapy (45 minutes per day). All patients were informed that they could choose between non-operative and operative treatment and were advised that non-operative treatment was recommended by the same team of spine specialists (>10 years of experience) lead by the senior author. We monitored if conversion to operative treatment was chosen by the patients or not for 6 weeks after admission to our institution. Patients who were not operated were allocated in Group 1, patients who were treated surgically were allocated in Group 2.
We recorded demographic data of patients, date of onset of pain, location and self-reported intensity (by VAS) of pain, neurological deficits, date of operation (if patients were operated), time of hospital stay and date of patients’ MRI after onset of pain.
The following data were recorded from the patients’ MRI’s
Cross sectional size of spinal canal and of LDH, location of LDH and grading of nerve root compromise (11) (touched, deviated or compressed). Measurements of spinal canal and LDH were performed according to Carragee et al. (9) and Thelander et al. (8) by an investigator that was not involved in the treatment of the patients.
Our hypothesis was that patients who eventually chose operative treatment would have more compression of the affected spinal nerve root and higher percentages of spinal canal stenosis than patients who were not treated by an operation.
Statistical analysis
Statistical Analysis was performed by SPSS 25 (© IBM, Armonk, USA). Descriptive Data are given as mean and standard error of mean. We tested all continuous variables for normal distribution by Kolmogorov-Smirnov tests.
Since volume of LDH did not show normal distribution, a one-sided Man-Whitney U Test (test number 1) was applied to compare percent (%) spinal canal compromise based on cross-sectional area of LDH of operated and not-operated patients.
We performed further statistical testing to establish a simple grading tool
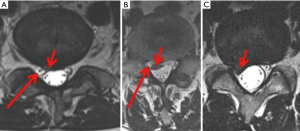
We divided degree of spinal canal stenosis into three groups: (I) stenosis 0–10%, (II) stenosis 11–50% and (III) stenosis of more than 50% (Figure 2). This grading system was tested by a Chi-Square test (test number 2). To adjust for multiple testing, Bonferroni adjustment was applied. The adjusted significance level for tests number 1 and 2 was P<0.025.
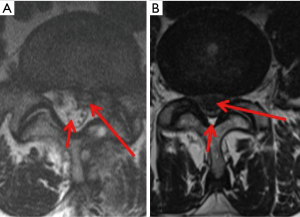
Effect of LDH on nerve root (Figure 3) (test number 3) was analyzed by another Chi-Square test. A significance level of P<0.05 was determined.
Power analysis was performed by G-Power (12,13).
This study was approved by the local ethics committee (registry number 5503) and was conducted according to the revised declaration of Helsinki.
No funding was received.
Results
Mean age of all patients was 43.9 (1.1) years, 43.41 (1.9) in Group 1, 44.1 (1.3) in Group 2. Hospital stay was 9.8 (0.5) days for all patients, 7.4 (0.6) days in Group 1, and 11.1 (0.6) days in Group 2. Grade of motor deficit did not change during conservative treatment and was 3.5 (0.1) for all patients, 3.7 (0.1) in Group 1, 3.4 (0.1) in Group 2. BMI was 26.3 (0.5) for all patients, 25.5 (0.6) in Group 1, 26.8 (0.6) in Group 2. Apart from hospital stay (P<0.05), all other parameters did not show a difference that was significant between Group 1 and 2 (P>0.05). Days of conservative treatment before surgery was 5.8 (0.5) days. Further descriptive data are given in Tables 1-3.
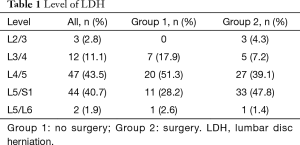
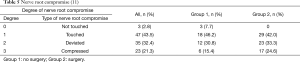
Full table
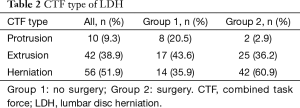
Full table
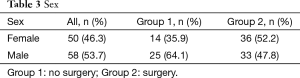
Full table
Percent (%) spinal canal compromise based on cross-sectional area of LDH was 30.9% (1.5%) for all patients, 26.3% (2.1%) in Group 1, 33.7% (2.0%) in Group 2. The difference was significant (P<0.025) with a high statistical power (>80%).
Degree of spinal canal stenosis [(I) stenosis 0–10%, (II) stenosis 11–50% and (III) stenosis of more than 50%] (Table 4) showed a difference that was significant between Group 1 (no surgery) and Group 2 (surgery) (P<0.025) with a medium effect size (0.3).
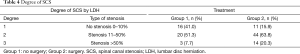
Full table
Grade of nerve root compromise (11) (Figure 3) did not show a difference that was significant between Group 1 and 2 (P>0.05) with a low effect size (0.1) (Table 5).
Discussion
This is the first study that investigates impact of size of LDH on treatment of patients without severe neurological deficit and without chronical low back pain.
Former investigations reported that size of LDH has a significant impact on outcome of treatment. Larger LDH are reported to show better outcome after surgical treatment and worse outcome after conservative treatment than smaller LDH (10). Early surgical treatment is reported to show significant better results with regard to time to return to work and improvement of health-related quality of life than postponed surgical treatment (1,2,4).
In our cohort, PWI who had a Grade 3 (Figure 2) spinal canal stenosis i.e., a larger LDH had a significantly higher probability of being treated by operation than other PWI.
Combined, these data indicate that surgery for PWI with high-grade (>50%) spinal canal stenosis may benefit from an early surgical treatment.
However, the weaknesses of this investigation do not allow a general recommendation to perform surgical treatment in all these cases: type of treatment in PWN is influenced by multiple factors including psychological and social variables, type of non-operative treatment and by the individual health care professionals.
We aimed to control these factors by our inclusion and exclusion criteria, but we could not avert all biases: psychosocial factors are reported to have significant impact on outcome and type of treatment (10), which is why we excluded patients with workers’ compensation involvement and chronical pain syndrome. Nevertheless, exclusion of all, especially more subtle, psychosocial factors is not possible and may have led to a bias in our investigation since type of treatment has always been chosen by the patient, and not by the spine surgeon.
Non-operative treatment was performed by a standardized protocol and all patients were equally advised by the same team that non-operative treatment was recommended. However, patients’ decision for type of treatment may have been influenced by the other health care professionals that were involved (physiotherapists and nurses).
We did not investigate long-term outcome of our patients since rate of additional or recurrent LDH after initial LDH is reported to be up to 25% and symptoms of a “second” LDH are often not to tell apart from “first” LDH (14-16). Analysis of patients with duration of pain for more than six weeks before admission to our institution or a longer follow up after onset of pain might cause a bias because of possible chronification of symptoms. Longer follow up might also lead to a bias by a non-detected additional LDH.
Long-term results of surgical versus non-surgical treatment are already reported in other studies: analyses of long-term results are still not conclusive, mostly because of substantial patient crossover between treatment groups (1,3), but Lurie et al. (2) still concluded that “careful selected patients” would benefit from surgical treatment.
A higher number of patients have been treated surgically [77] than conservatively [42]. This may be due to the preselection of patients: Only patients with severe pain (VAS ≥8) that persisted in spite of administration of intravenous pain medication according to step 3 of the WHO pain ladder were included in this investigation. All other patients (successfully treated by WHO steps 1 or 2) are usually not treated surgically.
Degree of nerve root compromise showed no impact on type of treatment in PWN.
The statistical power of the analysis of size of LDH with regard to choice of treatment was high, but the power of the analysis of impact of grade of compromise of nerve root was low and has to be interpreted under the light of this low statistical power.
On the one hand the careful selection of patients we performed is an advantage of this investigation, but on the other hand it also is a weakness since these results cannot be applied on all patients with a LDH but only for PWN and acute onset of pain without deformities or other spinal disorders and without psychosocial disorders.
It is not valid to derive a general recommendation for surgical treatment if PWN present with a high-grade stenosis of the spinal canal. Every single patient has to be evaluated and advised individually. However, the results of this study may be of value for explanatory discussions with PWN who have to decide which kind of treatment, operative or non-operative, they prefer.
Conclusions
Patients with a LDH without an indication for immediate surgical treatment had a significantly higher probability to need surgical treatment if they had a high-grade stenosis of the spinal canal by the LDH.
However, a high-grade stenosis of the spinal canal in PWI does not constitute a general indication for surgical treatment. The results of this study merely provide information for patients, and spine specialists, to be implemented in a decision-process that leads to an individual recommendation for type of treatment.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/jss-19-424). MRK reports personal fees from Globus Medical, outside the submitted work. RK reports personal fees from Corin, personal fees from Nuvasive, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the local ethics committee (registry number 5503) and was conducted according to the revised declaration of Helsinki.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Balaji VR, Chin KF, Tucker S, et al. Recovery of severe motor deficit secondary to herniated lumbar disc prolapse: is surgical intervention important? A systematic review. Eur Spine J 2014;23:1968-77. [Crossref] [PubMed]
- Lurie JD, Tosteson TD, Tosteson AN, et al. Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial. Spine (Phila Pa 1976) 2014;39:3-16. [Crossref] [PubMed]
- Matsui H, Kanamori M, Kawaguchi Y, et al. Clinical and electrophysiologic characteristics of compressed lumbar nerve roots. Spine (Phila Pa 1976) 1997;22:2100-5. [Crossref] [PubMed]
- Petr O, Glodny B, Brawanski K, et al. Immediate versus delayed surgical treatment of lumbar disc herniation for acute motor deficits: the impact of surgical timing on functional outcome. Spine (Phila Pa 1976) 2019;44:454-63. [Crossref] [PubMed]
- Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am 1990;72:403-8. [Crossref] [PubMed]
- Elfering A, Semmer N, Birkhofer D, et al. Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine (Phila Pa 1976) 2002;27:125-34. [Crossref] [PubMed]
- Iwabuchi M, Murakami K, Ara F, et al. The predictive factors for the resorption of a lumbar disc herniation on plain MRI. Fukushima J Med Sci 2010;56:91-7. [Crossref] [PubMed]
- Thelander U, Fagerlund M, Friberg S, et al. Describing the size of lumbar disc herniations using computed tomography. A comparison of different size index calculations and their relation to sciatica. Spine (Phila Pa 1976) 1994;19:1979-84. [Crossref] [PubMed]
- Carragee EJ, Kim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine (Phila Pa 1976) 1997;22:1650-60. [Crossref] [PubMed]
- Carlisle E, Luna M, Tsou PM, et al. Percent spinal canal compromise on MRI utilized for predicting the need for surgical treatment in single-level lumbar intervertebral disc herniation. Spine J 2005;5:608-14. [Crossref] [PubMed]
- Pfirrmann CW, Dora C, Schmid MR, et al. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology 2004;230:583-8. [Crossref] [PubMed]
- Faul F, Erdfelder E, Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-91. [Crossref] [PubMed]
- Faul F, Erdfelder E, Buchner A, et al. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009;41:1149-60. [Crossref] [PubMed]
- Fritzell P, Knutsson B, Sanden B, et al. Recurrent versus primary lumbar disc herniation surgery: patient-reported outcomes in the Swedish Spine Register Swespine. Clin Orthop Relat Res 2015;473:1978-84. [Crossref] [PubMed]
- Jansson KA, Németh G, Granath F, et al. Surgery for herniation of a lumbar disc in Sweden between 1987 and 1999. An analysis of 27,576 operations. J Bone Joint Surg Br 2004;86:841-7. [Crossref] [PubMed]
- Keskimäki I, Seitsalo S, Osterman H, et al. Reoperations after lumbar disc surgery: a population-based study of regional and interspecialty variations. Spine (Phila Pa 1976) 2000;25:1500-8. [Crossref] [PubMed]