
Correlation of neural foraminal motion after surgical treatment of cervical radiculopathy with long-term patient reported outcomes
Introduction
Surgical treatment of cervical degenerative disease with anterior cervical discectomy and fusion (ACDF), or arthroplasty with an artificial disc (AD) is considered highly successful; however, development of adjacent segment pathology (ASP) and reoperation involving adjacent segments occur after the initial surgery. The rate of adjacent segment reoperations after ACDF and AD have been reported to be up to 13.5% for more than 24 months follow-up (1).
It had been postulated that the pathophysiology of ASP was associated with altered biomechanics of the unoperated levels due to fusion of a vertebral segment, which places the other unoperated levels under greater stress than normal, for the case of ACDF. Motion preservation strategies have been developed as an alternative treatment with this in mind (2). Although recent meta-analyses of randomized controlled trials collectively indicate less adjacent segment degeneration and a lower incidence of secondary surgery involving adjacent segments for arthroplasty cohorts compared to fusion (3,4), a direct correlation between cervical spine motion after surgery and long-term outcomes has not been established.
If segmental motion is a determining factor in progression, one would expect a correlation between segment motion after surgery and future clinical outcomes. Therefore, the objective of this study was to examine correlations between cervical spine motion after surgery and long-term patient reported outcomes. Cervical motion is often characterized as the range of motion for the entire cervical spine or that of a given vertebra relative to the other in a segment; however, such range of motion variables have not been different between surgery types that give different clinical outcomes (4). Changes in the dimensions of the cervical neural foramina are considered to play a role in nerve root compression and development of cervical radiculopathy (5-7). Therefore, the focus of the current study was on dynamic dimensions of the foramina, which are known to change during physiological motion of the cervical spine (8,9). It was hypothesized that higher range and smaller values of foraminal dimensions observed during physiological motion of the neck correlate with worse longer-term patient reported outcomes.
Methods
Following institutional approval and informed consent, a convenience sample of 23 patients treated for cervical radiculopathy at C5–6 were enrolled. Sixteen patients underwent single-level ACDF (4 males, 12 females) and 7 patients underwent single-level cervical arthroplasty with an AD (3 males, 4 females). The mean time between surgery and the time of cervical spine motion measurements was 23.6 (standard deviation 6.8) months. The age range of patients at the time of motion measurements was 28–71 years. Patients with no complications or evidence of pseudarthrosis (ACDF group), device failure (AD group), or heterotopic ossification (AD group) were eligible for inclusion. All patients in the study also had no evidence of radiculopathy at the index level at the time of motion measurements.
Biplane X-ray images were acquired at 60 Hz during three trials of axial neck rotation and three trials of neck extension as previously described (10). CT images were also acquired of the cervical spine from C3 to the first thoracic vertebrae for each patient. Scans were performed on a LightSpeed16 system (GE Medical Systems, Milwaukee, WI, USA), in axial mode with 0.625-mm slice spacing, 0.25×0.25 pixel size, approximately 130 mm field of view (FOV) and 512×512 acquisition matrix. The subaxial cervical vertebrae (C3 to C7) were manually segmented (Mimics 12.0, Materialise, Leuven, Belgium) and reconstructed into 3D bone models. 3D positions and orientations of C3 through C7 were determined for every frame of the biplane X-ray images using the model-based tracking technique described previously (10-12).
Measurements of dynamic foraminal dimensions were performed following previously described procedures (9). Briefly, custom software was used to identify four anatomical landmarks per foramen on the 3D reconstructed model. The landmarks describing the vertebral foramen consisted of the most superior point of the inferior pedicle, the most inferior point of the superior pedicle, the anterolateral aspect of the superior vertebral body inferior notch, and the posterolateral aspect of the inferior vertebral body superior notch. Foraminal height (FH) and width (FW) were then calculated as the 3D distance between the supero-inferior (SI) and antero-posterior (AP) markers, respectively. The measurements were performed bilaterally at the upper and lower adjacent levels (C4–5 and C6–7, respectively), and were repeated for each frame of data. The minimum and the range of FH and FW values achieved during a motion task were averaged over three trials for the right and the left foramen. After that, the minimum of the left and right FH and FW was recorded as the minimum FH and minimum FW (FH.Min and FW.Min, respectively) for that participant. Similarly, the maximum of the two foramina was recorded to calculate the range of FH and FW (FH.Range and FW.Range, respectively). In addition, 3D FH and FW values were recorded from static views in neutral position (FH and FW, respectively).
In order to correlate dynamic foraminal motion with the clinical status of the participants longitudinally, the participants were given standard surveys at 6.5±1.1 years post-surgery. Each patient was assessed using the following validated patient reported outcome measures (13): the modified Japanese Orthopedic Association score (mJOAS) (14), the Neck Disability Index (NDI) including the visual analogue scale (VAS) for neck and arm pain, and the EuroQol EQ-5D score. The VAS and NDI assess for pain and functional disability directly related to neck and arm symptoms (higher worse). The mJOAS is a disease specific scale for assessing myelopathy (higher better) and the EQ-5D is a general health assessment (higher better).
Five patients did not return for follow-up, resulting in 7 female and 4 male patients {age 44.6±9.3 [28–58] years} in the ACDF group. Statistical analyses were performed using the data from the final cohort of 18 patients, for whom both motion and survey results were available. There was no evidence of a difference between AD and ACDF groups in terms of age (P>0.29), sex (P>0.78) or months after surgery at the time of initial testing (P>0.13) for the final cohort of 18 patients.
The correlations between clinical outcomes and adjacent segment foraminal motion were examined using Pearson’s correlation. When significant, regression analysis was used to examine the relationship. When looking at ACDF and AD patients, one would expect the motion characteristics that determine development of ASP to be universal, and be at play regardless of the segment being adjacent to an AD or a fused segment. Therefore, the two groups were pooled.
In order to enhance interpretation of the observed results, secondary analyses were performed using the mixed model ANOVA framework, and differences in foraminal variables between motion types and among intervertebral levels were examined. First, interactions between motion type and level were examined. Data were pooled over nonsignificant effect variables in final models. All analyses were performed using JMP (Cary, NC, USA) and statistical significance was set as P<0.05.
Results
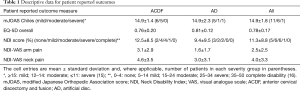
The majority of patients had mild (≥15) or moderate [12–14] levels of myelopathy according to their mJOAS, and none (0–4%) to moderate (15–24%) level of neck disability according to NDI (Table 1). No difference was found in any patient reported outcome between ACDF and AD groups.
Full table
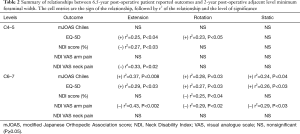
Higher mJOA scores were associated with higher values of minimum dynamic and static FWs at the C6–7 level (Table 2, Figure 1). The minimum FW at C6–7 achieved during neck extension appeared more explanatory than the other measurements for mJOAS (r2=0.37 vs. 0.24–0.28).
Full table
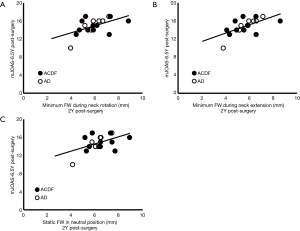
Higher EQ-5D scores were associated with higher values of minimum dynamic and static FWs at the C6–7 level, and with minimum dynamic widths at the C4–5 level (Table 2). The minimum FW at C6–7 achieved during neck extension appeared more explanatory than the other measurements for EQ-5D (r2=0.29 vs. 0.23–0.27).
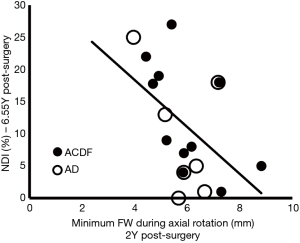
Higher NDI % scores were associated with lower values of minimum FW during extension at the C4–5 and during rotation at the C6–7 adjacent levels (Table 2, Figure 2). Interestingly, higher values of NDI VAS for arm pain were associated with lower values of FW.Min at the lower adjacent level whereas higher values of NDI VAS scores for neck pain were associated with lower values of FW.Min at the upper adjacent levels.
All other correlations between dynamic or static foraminal variables from the adjacent levels and patient reported outcomes were nonsignificant. Notably, FH was not associated with the outcomes.
With regards to the FH changes observed during motion, a significant effect of motion type was found on FH.Min (P<0.0001). FH.Min measured from static images was significantly greater than those from the dynamic assessment, but no difference was found between neck extension and rotation (Table 3). The effect of motion type was significant also on FH.Range (P<0.005), with the range being greater in axial rotation than in extension (Table 3).
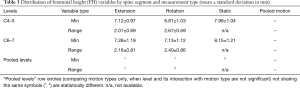
Full table
A significant effect of motion type was found on FW.Min as well (P<0.0007). As in the case of FH.Min, FW.Min measured from static images were significantly greater than those from the dynamic assessment, but no difference was found between neck extension and rotation (Table 4). In addition, the effect of level on FW.Min was significant (P<0.0001), with FW.Min being smaller at C4–5 than the C6–7 level (Table 4). Both motion type (P<0.02) and level (P<0.004) were significant in FW.Range, with FW.Range being greater in neck extension than rotation and greater at the C4–5 level than at the C6–7 level (Table 4).
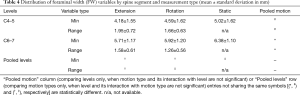
Full table
Discussion
The levels of function and pain as measured from NDI and mJOAS (Table 1) were generally in agreement with a recent report with a cohort and follow-up period similar to ours (17). Although our NDI scores were lower on average compared to some previous studies, considering the large variability in these results, they are well within the reported ranges (18-22). The differences may be attributable to inclusion criteria such as no radiculopathy at the time of motion analysis (2 years post-surgery), single- vs. multi-level surgery and follow-up time. We used 2-year post-operative motion as the baseline, as the effect of fusion surgery on cervical motion may not reach a steady state at earlier time points (23).
In general, worsening scores (lower mJOAS, EQ-5D and higher NDI) were associated with lower values of minimum FW, consistent with the idea that wider foramina are less likely to compress nerve roots and cause myelopathic symptoms. However, this result was not coincident with a correlation between increased range of foraminal motion and worsening symptoms. As such, the association between narrow foramina and worsening symptoms may not necessarily be a result of increased range of foraminal motion at adjacent levels, that is often considered to occur compensatory to limited motion at the surgery site.
The persistent correlation of FW rather than FH with the outcomes may be due to the smaller value of FW than FH, presenting a more critical distance between the foraminal wall and the nerve root. As such, factors that affect FW directly may be important determinants of outcomes. These may include dynamic factors such as translation of vertebral bodies during neck motion, and static factors such as the AP alignment or spondylotic changes from disc/osteophyte complexes.
Although results were generally in agreement between motion types including static images, the correlations found from neck extension were stronger. Smaller values of FW were achieved during dynamic measurements compared to the static measurement, suggesting that dynamic measurements are more relevant to risk of nerve root compression. Smaller FW was observed during neck extension than during neck rotation in a previous study of young asymptomatic subjects (9); however, there was no such significant difference in the current study. As such, the stronger correlation for neck extension cannot simply be attributable to smaller FW observed during this type of motion. It is possible that dynamic foraminal dimensions are more reliably measurable during neck extension than during neck rotation. The variability of FW among repeated trials were less in neck extension than in rotation in previous work (9), supporting this argument. Alternatively, dynamic mechanisms involved in the development of clinical outcomes, though not revealed by the current tests, are better represented in neck extension tasks.
Measurements from the lower adjacent C6–7 level during neck extension were more strongly and consistently (across different motion and outcome types) associated with the mJOAS (r2=0.37 vs. 0.23–0.28), EQ-5D (r2=0.29 vs. 0.23–0.26) and NDI Arm Pain VAS (r2=0.43 vs. 0.22–0.29) outcomes than from the upper adjacent level, consistent with C6–7 being the most common adjacent level to degenerate after surgical treatment of C5–6 (24). This is despite the fact that C6–7 has larger foramina than superior levels (25,26). More recent studies utilizing ultrasonography and larger patient samples report that nerve root size also increases from superior to inferior levels (27-29), suggesting that larger foraminal size at the C6–7 level does not protect this segment from risk due to the correspondingly large nerve roots. Future work could benefit from incorporation of nerve root measurements in the analysis of foraminal motion. It is possible that results from the lower adjacent C6–7 level correlate better with mJOAS, EQ-5D and NDI Arm Pain VAS because C6–7 nerves control and provide sensation to arms and wrists, which may have more pronounced effects on patients’ own evaluation of their myelopathic symptoms, general well-being and arm pain. Whereas measurements from the upper adjacent C4–5 level had better correlations with NDI Neck Pain VAS and overall NDI scores, possibly because the upper levels provide sensation to more superior regions, i.e., the neck mantle and shoulder, than do the other levels examined.
The limitations of this study included a relatively small number of patients. Nonetheless, the current data would be valuable in guiding future larger scale studies aiming to establish causative relationships or protocols for utilizing foraminal motion in predicting outcomes. The data from ACDF and AD groups were largely overlapped (Figures 1,2), as would be expected if there is universality of the relationships between dynamic foraminal motion and the outcomes. However, future work with larger samples of each group may reveal differences in the way foraminal motion is related to clinical outcomes between AD and ACDF surgeries. The lack of baseline data on patient reported outcomes must also be recognized. Given that the majority of the participants in the current study had mJOAS that would put them in the mild or moderate myelopathy categories at the time of follow-up, their baseline value might be of less concern. Further studies with larger range of outcomes and baseline data would help with identification of which relationships between foraminal motion and patient reported outcomes have prognostic value. We were unable to acquire magnetic resonance imaging (MRI) images from all patients who participated in follow-up surveys. As such, radiographic findings accompanying patient reported outcomes are not reported.
In conclusion, the current study demonstrated an association between dynamic foraminal motion, notably minimum FW achieved during neck motion, and patient reported outcomes in patients who received surgical treatment for cervical radiculopathy followed up for 6.5 years. Though motion-related factors were associated with the outcomes, these factors were not necessarily representative of increased range of motion at adjacent levels. The relationships found in this work provide insight into the potential role of motion related factors in the development of pain and loss of function, and may be useful in further development of prognostic markers and preventative interventions. Additional, larger studies are needed to establish the causative nature of the current observations.
Acknowledgments
Funding: Part of this work was supported by a CNS Fellowship Award in Spine (VC). The sponsor had no involvement in study design, collection, analysis and interpretation of data, writing of the report or decision to submit the article for publication.
Footnote
Conflicts of Interest: SW Bartol owns shares in Sentio LLC, is a consultant for LDR and DePuy Synthes, and a member of the Medical Board of Trustees of MTF. A Basheer is a consultant for DePuy/Synthes Spine and SeaSpine. V Chang is a consultant for Globus Medical and SpineGuard. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was reviewed and approved by the Institutional Review Board (IRB Protocol #9165). All participants provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dong L, Wang D, Chen X, et al. A Comprehensive Meta-Analysis of the Adjacent Segment Parameters in Cervical Disk Arthroplasty Versus Anterior Cervical Discectomy and Fusion. Clin Spine Surg 2018;31:162-73. [Crossref] [PubMed]
- Fekete TF, Porchet F. Overview of disc arthroplasty-past, present and future. Acta Neurochir (Wien) 2010;152:393-404. [Crossref] [PubMed]
- Hu Y, Lv G, Ren S, et al. Mid- to Long-Term Outcomes of Cervical Disc Arthroplasty versus Anterior Cervical Discectomy and Fusion for Treatment of Symptomatic Cervical Disc Disease: A Systematic Review and Meta-Analysis of Eight Prospective Randomized Controlled Trials. PloS One 2016;11:e0149312. [Crossref] [PubMed]
- Dong L, Xu Z, Chen X, et al. The change of adjacent segment after cervical disc arthroplasty compared with anterior cervical discectomy and fusion: a meta-analysis of randomized controlled trials. Spine J 2017;17:1549-58. [Crossref] [PubMed]
- Abbed KM, Coumans JV. Cervical radiculopathy: pathophysiology, presentation, and clinical evaluation. Neurosurgery 2007;60:S28-34. [Crossref] [PubMed]
- Yousem DM, Atlas SW, Goldberg HI, et al. Degenerative narrowing of the cervical spine neural foramina: evaluation with high-resolution 3DFT gradient-echo MR imaging. AJNR Am J Neuroradiol 1991;12:229-36. [PubMed]
- Wainner RS, Gill H. Diagnosis and nonoperative management of cervical radiculopathy. J Orthop Sports Phys Ther 2000;30:728-44. [Crossref] [PubMed]
- Anderst WJ. Automated measurement of neural foramen cross-sectional area during in vivo functional movement. Comput Methods Biomech Biomed Engin 2012;15:1313-21. [Crossref] [PubMed]
- Chang V, Basheer A, Baumer T, et al. Dynamic measurements of cervical neural foramina during neck movements in asymptomatic young volunteers. Surg Radiol Anat 2017;39:1069-78. [Crossref] [PubMed]
- McDonald CP, Chang V, McDonald M, et al. Three-dimensional motion analysis of the cervical spine for comparison of anterior cervical decompression and fusion versus artificial disc replacement in 17 patients: clinical article. J Neurosurg Spine 2014;20:245-55. [Crossref] [PubMed]
- McDonald CP, Bachison CC, Chang V, et al. Three-dimensional dynamic in vivo motion of the cervical spine: assessment of measurement accuracy and preliminary findings. Spine J 2010;10:497-504. [Crossref] [PubMed]
- Bey MJ, Zauel R, Brock SK, et al. Validation of a new model-based tracking technique for measuring three-dimensional, in vivo glenohumeral joint kinematics. J Biomech Eng 2006;128:604-9. [Crossref] [PubMed]
- Vavken P, Ganal-Antonio AK, Quidde J, et al. Fundamentals of Clinical Outcomes Assessment for Spinal Disorders: Clinical Outcome Instruments and Applications. Global Spine J 2015;5:329-38. [Crossref] [PubMed]
- Chiles BW 3rd, Leonard MA, Choudhri HF, et al. Cervical spondylotic myelopathy: patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery 1999;44:762-9; discussion 769-70. [Crossref] [PubMed]
- Fehlings MG, Wilson JR, Kopjar B, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am 2013;95:1651-8. [Crossref] [PubMed]
- Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 1991;14:409-15. [PubMed]
- Tian W, Yan K, Han X, et al. Comparison of the Clinical and Radiographic Results Between Cervical Artificial Disk Replacement and Anterior Cervical Fusion: A 6-Year Prospective Nonrandomized Comparative Study. Clin Spine Surg 2017;30:E578-86. [Crossref] [PubMed]
- Schroeder GD, Coric D, Kim HJ, et al. Are patient-reported outcomes predictive of patient satisfaction 5 years after anterior cervical spine surgery? Spine J 2017;17:943-52. [Crossref] [PubMed]
- Meisel HJ, Jurak L, Antinheimo J, et al. Four-year results of a prospective single-arm study on 200 semi-constrained total cervical disc prostheses: clinical and radiographic outcome. J Neurosurg Spine 2016;25:556-65. [Crossref] [PubMed]
- Hisey MS, Zigler JE, Jackson R, et al. Prospective, Randomized Comparison of One-level Mobi-C Cervical Total Disc Replacement vs. Anterior Cervical Discectomy and Fusion: Results at 5-year Follow-up. Int J Spine Surg 2016;10:10. [Crossref] [PubMed]
- Burkus JK, Traynelis VC, Haid RW Jr, et al. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial: Clinical article. J Neurosurg Spine 2014;21:516-28. [Crossref] [PubMed]
- Sasso RC, Anderson PA, Riew KD, et al. Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am 2011;93:1684-92. [Crossref] [PubMed]
- Anderst WJ, West T, Donaldson WF 3rd, et al. Longitudinal Study of the Six Degrees of Freedom Cervical Spine Range of Motion During Dynamic Flexion, Extension, and Rotation After Single-level Anterior Arthrodesis. Spine (Phila Pa 1976) 2016;41:E1319-27. [Crossref] [PubMed]
- Komura S, Miyamoto K, Hosoe H, et al. Lower incidence of adjacent segment degeneration after anterior cervical fusion found with those fusing C5-6 and C6-7 than those leaving C5-6 or C6-7 as an adjacent level. J Spinal Disord Tech 2012;25:23-9. [Crossref] [PubMed]
- Ebraheim NA, Reader D, Xu R, et al. The location of the spinal nerve root on plain radiographs of the cervical spine. Orthopedics 1998;21:333-5. [PubMed]
- Humphreys SC, Hodges SD, Patwardhan A, et al. The natural history of the cervical foramen in symptomatic and asymptomatic individuals aged 20-60 years as measured by magnetic resonance imaging. A descriptive approach. Spine (Phila Pa 1976) 1998;23:2180-4. [Crossref] [PubMed]
- Won SJ, Kim BJ, Park KS, et al. Measurement of cross-sectional area of cervical roots and brachial plexus trunks. Muscle Nerve 2012;46:711-6. [Crossref] [PubMed]
- Sugimoto T, Ochi K, Hosomi N, et al. Ultrasonographic reference sizes of the median and ulnar nerves and the cervical nerve roots in healthy Japanese adults. Ultrasound Med Biol 2013;39:1560-70. [Crossref] [PubMed]
- Takeuchi M, Wakao N, Kamiya M, et al. Morphological distinction of cervical nerve roots associated with motor function in 219 healthy volunteers: a multicenter prospective study. Spine (Phila Pa 1976) 2014;39:E944-9. [Crossref] [PubMed]


