Pullout force of minimally invasive surgical and open pedicle screws—a biomechanical cadaveric study
Introduction
The spine is exposed to forces of compression, shear bending, and torsion/axial rotation. The function of the pedicle is to transmit tension and bending forces from the posterior elements to the vertebral bodies; this results in unique vectors and forces upon the pedicle (1).
Pedicle screw and rod fixation is an effective method for stabilisation of the spine. The stability of the construct relies mainly on the mechanical properties of the bone-screw interface (2,3). Finite element analysis of screw-bone interactions has shown the greatest physiological forces along the pedicle screw is during flexion, and least in extension (4,5). During flexion, the pedicle screw is subjected to an axial loading force from the affixed rod resisting the motion (6).
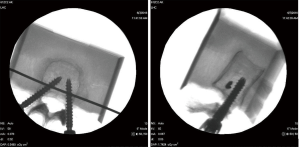
Traditionally, pedicle screws are inserted in an open procedure (7). In an effort to reduce tissue morbidity and improve patient recovery times, minimally invasive surgical (MIS) techniques have been developed, which utilise a different insertion site and screw trajectory as a result of the surgical access (8) (Figure 1). The traditional Open surgical placement abuts the facet joint, with the screw traversing sclerotic cortical bone. In contrast, the MIS insertion site is at the junction of the transverse process and facet, which has less cortical bone. The biomechanical implications of the altered pedicle screw placement are not well defined. Previous investigations show conflicting results, with some evidence favouring a more medial entry and straighter trajectory, while other research supports increased stability with increased convergence of the screws (10,11).
The role of the pedicle screw is to secure posterior fixation systems to the vertebrae. Postoperative failure can occur, with loosening of hardware or fracture of the bony elements occurring in approximately 5% of patients having undergone lumbar fusion (12). Pedicle screw failure leads to failure of fusion, resulting in pain and eventually revision surgery. Mechanical factors that influence failure include the size of the screw in relation to the pedicle diameter, screw length and amount of bony purchase, the character of the thread, the entry site and trajectory of the screw. Patient factors are multiple, with bone mineral density of most consistent significance.
Fusion rates are comparable between MIS and Open lumbar fusion, although failure rates and subsequent revision have been shown to be increased in minimally invasive lumbar spinal fusion surgery (12).
In this study we hypothesise that the more frequent failure of the pedicle screws inserted with MIS technique may be due to the difference in applied forces as a result of the differences in bone quality between the insertion sites or along the trajectory of the pedicle screw. This study aims to contribute to this knowledge by comparing the pull-out force and other biomechanical properties of pedicle screws inserted using MIS and Open lumbar fusion techniques.
Methods
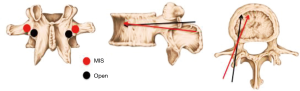
Intact lumbar spines (L1–L5) were dissected from five fresh cadavers (mean age 76 years, SD 14 years) and DEXA scans were obtained to determine bone mineral density (BMD). All 25 vertebrae were individually dissected and cleaned of all soft tissue before being potted in a rectangular plastic tube using polymethyl methacrylate (PMMA) cement (Figure 2). Care was taken to not embed the pedicles, so as to avoid the PMMA contributing to the forces experienced between the pedicle and screw. Screw length and diameter were individualised for each vertebra, but was consistent between the tests on either side acting as internal control (Table 1).


Full table
The spines were instrumented using two different techniques: MIS and Open. The MIS technique places the insertion site lateral to that of the Open screw, at the junction of the transverse process and facet at the mid-point of the transverse process. In the Open technique, the pedicle screw entry point is at the lateral border of superior articular process at the lower margin of the transverse process. Given the more lateral entry point, the MIS screw has a more triangulated trajectory (Figure 1). Each vertebra was cannulated with one MIS and one Open pedicle screw (Figure 2) and the MIS/Open arrangement was alternated in adjacent vertebrae. The same type of screw was used for both techniques.
C-arm (Fluoroscan Insight, Hologic, MA, USA) images were captured after the insertion of the pedicle screws to confirm correct placement and alignment (Figure 3). X-ray images (Practix 160, Philips, NSW, Australia) were also captured prior to testing, as these images allowed for reliable scaling of geometrical measurements of the screw positions for each specimen.
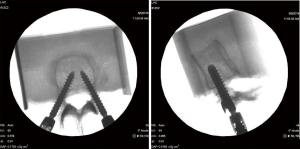
A K-wire was placed through the potting cement and the specimen, in order to add rigidity to the construct and decrease the chances of the specimen pulling out of the cement. Hologic, MA, USA) was used to confirm that the K-wire did not interfere with screws (Figure 4).
The potted vertebrae were fixed to the base of an Instron E10000 mechanical tester (Instron, Illinois, USA) using a vice with 3 degrees of rotational freedom. The screw being tested was aligned coaxially with the linear actuator and the head of the screw connected to the load cell with a custom fixture (Figure 5). A direct load-to-fail test was conducted at a constant displacement rate of 5 mm/min [as per protocols adapted from (7,13,14)].

Images were captured using high definition cameras (JAI ltd, Japan, CB-200GE) to monitor the failure mode of each construct.
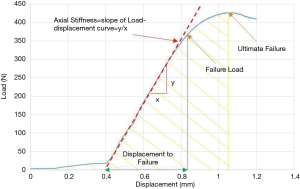
Load and displacement data were collected using Instron WaveMatrix™ (Illinois, USA) data acquisition software at a frequency of 100 Hz and the failure load, displacement to failure and the ultimate failure load of each construct determined. The axial stiffness and work to ultimate failure were calculated based on the captured data. Axial stiffness was defined as the slope of the linear elastic portion of the load-displacement curve, and work to ultimate failure as the area under the curve up to the ultimate failure load (Figure 6).
Paired t-tests were used to compare the results for the two groups. In addition, Pearson’s correlation coefficients (PCC) were calculated between each mechanical property and the remaining mechanical properties as well as with other specimen specific parameters including BMD, donor age, and geometric measurements (Figure 4).
Results
There was no significant difference between any of the mechanical properties considered in this study.
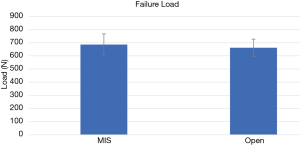
The mean failure loads were: 685±399 N for MIS vs. 661±323 N for open (P=0.75) (Figure 7).
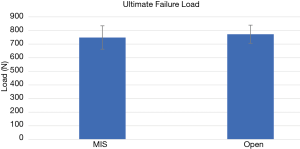
The average Ultimate Failure loads were: 748±421 N for MIS vs. 772±326 N for open (P=0.74) (Figure 8).
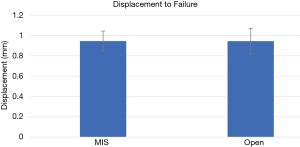
The displacement to failure were: 0.95±0.49 mm for MIS vs. 0.95±0.62 mm for open (P=0.996) (Figure 9).
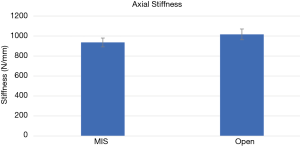
The axial stiffness values were: 936±217 N/mm for MIS vs. 1,016±263 N/mm for open (P=0.19) (Figure 10).
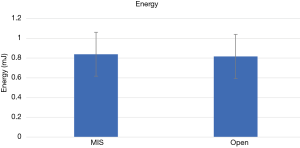
The energy expenditure to ultimate failure was: 0.84±1.09 J for MIS vs. 0.82±1.05 J for open (P=0.94) (Figure 11).
Data were also grouped by donor and by vertebral level, to assess for differences between MIS and Open techniques specific to the patient or vertebral level. There was no statistically significant difference between the two techniques for any of the above properties.
Pearson’s correlation coefficients were determined between each mechanical property and all other mechanical properties (Table 2), as well as all mechanical properties and the specimen-specific parameters of BMD, donor age, and screw position (Table 3). Failure load, ultimate failure load, displacement to failure, and energy to ultimate failure all correlated strongly with each other (R>0.6) (Table 2). In contrast, axial stiffness displayed weak or very weak correlation with all other mechanical properties (R<0.4) (Table 2). BMD, donor age, and geometrical position of the screw showed little evidence of correlation with any mechanical property (R<0.5) (Table 3).
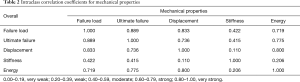
Full table
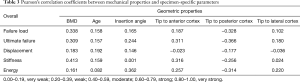
Full table
Testing was completed when the pedicle screw failed, either via the screw pulling out of the bone, or breaking of the pedicle. There was no difference between MIS and open groups—each technique had five pedicles snap and 20 screws pull out. Broken pedicles were not dependent on whether the tested pedicle was first or second to the actuator.
Discussion
No difference was seen in the forces required for pedicle screw failure in the open as compared to MIS placement. This implies that the insertion site bone purchase and screw trajectory do not contribute to a difference in failure of fusion.
The failure load, ultimate failure, and energy to failure are consistent with previously reported values (14). The displacement to failure, however, was less than in other similarly designed studies. In this study, average displacement to failure was 0.95 mm for both groups, with average displacements in comparable studies reporting values around 2.5 mm (14,15). This could be related to a discrepancy in measurement technique, with regards to the inherent lag in the system. In our study, we determined the start point of displacement to be the initial inflection point of the load-displacement curve. This results in the shortest possible determination of the displacement value. Alternatively, the shorter displacement with similar force to failure may be indicative of increased brittleness of bone.
Degree of brittleness is quantified by axial stiffness. Expectedly, the axial stiffness that we have reported is greater than that observed by other groups. We reported an axial stiffness of 936 N/mm for MIS and 1,016 N/mm for the Open technique, as compared to 380 N/mm reported by Koller et al. and 160 N/mm by Mehta et al. although of note, these studies were not designed to compare different insertion points (13,14). Again, it is unclear whether this is reflective of a discrepancy in measurement of displacement, or representative of differences in bony characteristics such as bone mineral density. The average BMD in our study is 0.98±0.23 g/cm2, which is higher than those reported in Koller et al. (14) and Mehta et al. (13) of 0.67±0.19 g/cm2 and 0.514±0.06 g/cm2, respectively. The higher BMD would likely result in a higher axial stiffness, which in turn would impact the displacement results.
Albeit not significant, our results showed a trend towards increased axial stiffness in the open group. If a true finding, this is possibly attributable to the difference in entry point of the two methods. The open technique traverses the superior articular process and thus is embedded in sclerotic cortical bone, which is more rigid than cancellous bone. The difference in axial stiffness did not correlate with an increased failure load, however.
This study was designed to assess how the biomechanical properties differ in an open versus MIS placement. In order to isolate the variable of screw placement, a single vector of force was applied to the screw. We acknowledge that a direct coaxial force, in isolation of other vectors, is not a situation that is likely translatable to the in vivo setting. Cyclic toggling of the screw, as described by Inceoğlu et al. (8), helps provide more realistic loading on the screw. It would be of interest to compare the effect of cyclic toggling versus direct axial loading on each group. Furthermore, the same vector of force was performed on both the MIS and Open groups. However, it is expected that these screw placements would be subjected to different components of force in the clinical setting given they have different entry points and different triangulation angles.
Additionally, in each individual vertebral body studied, the MIS and Open screws were of the same diameter, thread character, and length, thus inserted to the same depth, to impose consistency and isolate the entry point as a variable. In reality though, due to the angle of insertion you can have greater length and therefore greater purchase with MIS, which would possibly affect the pullout force. Likewise, the bone mineral density and age of the patient was controlled for, which may not replicate clinical application.
Interestingly, the ultimate failure load is dependent on the displacement rate of the load-to-fail test (8,15,16), which is an important consideration in study design. Given our displacement rate was consistent with that of other groups, our results are able to be compared with theirs. Extrapolation to the clinical setting is less clear, however, given there would not be a standard or even consistent displacement rate or loading condition.
Lastly, while a cadaveric model is the most authentic representation of the clinical scenario when compared with the artificial materials used by other groups, we acknowledge that disarticulated specimen isolated from adjacent joint support and soft tissue fails to perfectly replicate the physiological environment to the applied stresses. Given the preservation of soft tissue structures is a significant advantage of MIS surgery, the disarticulated model may not accurately represent the transmission of forces experienced by the construct following MIS as compared to Open surgery.
Conclusions
With a coaxial pullout test, there is no statistical difference between the mechanical properties of the pedicle screws for the MIS and Open entry point and trajectory. A larger study could be performed to determine if the trend in axial stiffness is a true difference between MIS and Open groups. However, this did not impact the failure load, ultimate failure load, or energy to failure, so is not likely to result in a clinically significant difference under the loading conditions of this study.
Future studies could be designed to replicate the in vivo environment and assess whether this results in a difference between MIS and Open pedicle screw biomechanical properties. Cyclical toggling prior to coaxial force, or a non-coaxial force designed to simulate the rod placement, may reveal a difference between the two techniques.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The protocol for the research has been approved by the Macquarie University Human Research Ethics Committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rathore M, Sharma DK, Sinha MB, et al. A focused review – Thoracolumbar spine: anatomy, biomechanics, and clinical significance. Indian J Clin Anat Physiol 2014;1:41-7.
- Inceoglu S, Ferrara L, McLain RF. Pedicle screw fixation strength: pullout versus insertional torque. Spine J 2004;4:513-8. [Crossref] [PubMed]
- Abshire BB, McLain RF, Valdevit A, et al. Characteristics of pullout failure in conical and cylindrical pedicle screws after full insertion and back-out. Spine J 2001;1:408-14. [Crossref] [PubMed]
- La Barbera L, Ottardi C, Villa T. Comparative analysis of international standards for the fatigue testing of posterior spinal fixation systems: the importance of preload in ISO 12189. Spine J 2015;15:2290-6. [Crossref] [PubMed]
- Xu M, Yang J, Lieberman IH, et al. Finite element method-based study of pedicle screw-bone connection in pullout test and physiological spinal loads. Med Eng Phys 2019;67:11-21. [Crossref] [PubMed]
- La Barbera L, Galbusera F, Wilke HJ, et al. Preclinical evaluation of posterior spine stabilization devices: can the current standards represent basic everyday life activities? Eur Spine J 2016;25:2909-18. [Crossref] [PubMed]
- Becker S, Chavanne A, Spitaler R, et al. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur Spine J 2008;17:1462-9. [Crossref] [PubMed]
- Inceoğlu S, Montgomery WH Jr, St Clair S, et al. Pedicle screw insertion angle and pullout strength: comparison of 2 proposed strategies. J Neurosurg Spine 2011;14:670-6. [Crossref] [PubMed]
- Image adapted under license. Available online: stihii/Shutterstock.com
- Sterba W, Kim DG, Fyhrie DP, et al. Biomechanical analysis of differing pedicle screw insertion angles. Clin Biomech (Bristol, Avon) 2007;22:385-91. [Crossref] [PubMed]
- Vcelak J, Tichy P, Bouda T, et al. Pedicle screw convergence impact on the stability of transpedicular fixation spine model in cyclic loading: biomechanical study. J Mech Med Biol 2015;15:1550078. [Crossref]
- Jin-Tao Q, Yu T, Mei W, et al. Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: a meta-analysis. Eur Spine J 2015;24:1058-65. [Crossref] [PubMed]
- Mehta H, Santos E, Ledonio C, et al. Biomechanical analysis of pedicle screw thread differential design in an osteoporotic cadaver model. Clin Biomech (Bristol, Avon) 2012;27:234-40. [Crossref] [PubMed]
- Koller H, Zenner J, Hitzl W, et al. The impact of a distal expansion mechanism added to a standard pedicle screw on pullout resistance. A biomechanical study. Spine J 2013;13:532-41. [Crossref] [PubMed]
- Jacob AT, Ingalhalikar AV, Morgan JH, et al. Biomechanical comparison of single- and dual-lead pedicle screws in cadaveric spine: Laboratory investigation. J Neurosurg Spine 2008;8:52-7. [Crossref] [PubMed]
- Paik H, Dmitriev AE, Lehman RA Jr, et al. The biomechanical effect of pedicle screw hubbing on pullout resistance in the thoracic spine. Spine J 2012;12:417-24. [Crossref] [PubMed]