
A review of cervical spine alignment in the normal and degenerative spine
Introduction
With the emergence of modern technology and advanced surgical techniques, the importance of understanding global spine alignment has evolved as a critical pillar in determining severity of spinal pathology and operative decision-making. Novel innovations in surgical techniques, including segmental instrumentation, interbody cages, and a variety of osteotomy techniques have all been designed to help contribute to overall spinal stability and improved spine alignment. Similarly, improvements in bone graft substitutes such as bone morphogenetic protein and grafting materials have helped to improve fusion success rates once spinal alignment is optimized.
The Debousset theory (1) of the “conus of economy” stressed the importance of spinopelvic balance in providing a framework to maintain an upright posture and exert minimal effort/energy expenditure. While studies have predominantly focused on the lumbosacral-pelvic axis, recent interest in the field of cervical spine pathology/deformity has emphasized the importance of cervical sagittal alignment and its impact on symptomatology and surgical planning. Moreover, the recent literature has examined the relationship of cervical alignment to the alignment of the thoracolumbar spine and the importance of considering the entire spinal axis in surgical decision making. The aim of our review is to investigate the anatomic/physiologic variations of global spine alignment and its impact on cervical spine pathology, as well as patient-reported outcomes (PRO).
Cervical/global spine anatomy and biomechanics
The spine, or vertebral column, is a network of 33 bones, separated/cushioned by intervertebral discs, and stabilized by surrounding ligaments/musculature. While primarily functioning to protect the spinal cord from significant impact and injury, it also functions to support the weight-bearing forces of the body and aid in mobility/flexibility. Classically, the spine is separated into 5 regions consisting of: 7 cervical vertebrae, 12 thoracic vertebrae, 5 lumbar vertebrae, 5 fused sacral vertebrae, and the 4 fused bones of the coccyx. Each vertebra can be separated into three functional parts: the vertebral body/intervertebral discs, the spinal canal, and the transverse/spinous processes/facet joints (2). While these parts are common between each of the levels of the spine, unique properties emerge in specific regions creating variations in motion and predisposition to certain pathologies.
The superior craniocervical spine is comprised of the cranium, C1 (atlas), and C2 (axis). This region of the spine exhibits unique anatomy and biomechanics that differ from the subaxial cervical spine. When considering the placement of internal fixation into the occiput, particular attention must be given to the vertebral foramen and thickness of the keel of the occipital bone to avoid vascular/neurologic injury. C1 has no vertebral body (centrum) and articulates with odontoid process of C2 anteriorly (3). The rest of the cervical spine from C3 to C7 exhibits uniform properties with gradual enlargement of the vertebral bodies as one descends lower in the subaxial spine. The normal cervical alignment can vary from lordotic to neutral to kyphotic depending on a patient’s normal global spinal alignment. The more common cervical lordotic curve allows for greater distribution of weight-bearing forces brought upon by the weight of the head and leads to the distribution of forces throughout the lower cervical region. The cervicothoracic junction (CTJ) is a transition from cervical lordosis (CL) to thoracic kyphosis (TK) with a transitional C7 lateral mass which is generally smaller than the lateral masses of C3-C6.
The thoracic spine extends from T1 to T12. Normal TK ranges from 18° to 51°. This region of the spine is protected from blunt trauma due to the presence of a surrounding rib cage. The thoracolumbar junction (TLJ), often referring to the T12/L1 levels, is now often referred to as the thoracolumbar zone (TLZ) and describes the general region from approximately T9 down to L2. The transitional nature of the TLJ form the rigid thoracic region to the mobile lumbar region makes it more susceptible to injury from axial loading.
The lumbar spine extends from L1 to L5 followed below by the sacrum and then coccyx. This regions is characterized with larger vertebral bodies and resumption of a lordotic curve (42° to 74°) more conducive for axial loading and resistance to excess force (4,5). The facet joints are oriented more in the sagittal plane, allowing for flexion/extension and lateral bending, but limiting rotatory movement. The lumbosacral junction (LSJ) can have significant variations in curvature and in combination with the steep angle of the L5-S1 joint, this region is exposed to significant translational forces and shear stress.
Cervical/global spine parameters
Despite the regional anatomic differences outlined in section above, from the skull base to the pelvis, the spinal unit functions in a dynamic continuum both in the sagittal and coronal planes. Optimal spinal balance consists of the head overlying the pelvis with a sustained horizontal gaze, neck neutral, shoulders neutral or slightly flexed, elbows slightly flexed, and the hip/knees extended (6). Disruption in the functional alignment among these three components may lead to significant deformity and disability. With the advent of radiography and advanced imaging, physicians are now able to quantify the existing state of a patient’s spinal alignment with a myriad of different parametric measurements (both regionally and globally) of the cervical, thoracic, and lumbosacral spine.
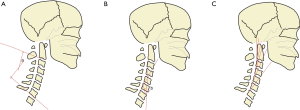
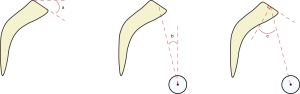
In the sagittal plane, the cervical spine has the most mobility of any other spinal segment, and must maintain a position that allows for horizontal gaze. Angular relationships are often described in the sagittal plane, with convention dictating a negative value for lordosis and positive value for kyphosis (7). Routine A/P and lateral radiographs are often used to help assess cervical alignment with either of three widely known techniques: the Cobb angle (CA, Figure 1A), Jackson physiologic stress lines (JPA, Figure 1B), and/or Harrison posterior angle (HPA, Figure 1C) (8). The CA, the most commonly utilized technique to measure sagittal alignment, can help assess the degree of lordosis (or kyphosis) of the cervical spine. Commonly, the C2–C7 CA (Figure 2A, angle d), also known as CL, is measured by drawing a line parallel to the inferior endplate of C2 and another line inferior to the endplate C7, drawing a perpendicular line to each of those two lines, and recording the angle of intersection. While commonly done between C2 and C7, some studies have utilized C1 as a starting point with a line drawn from the anterior C1 tubercle to the posterior ring of C1, however this has been known to overestimate CL. A recent study by Zhang et al. (9) revealed that a C2 to C6 measurement might be just as effective as C2 to C7, with a higher reliability because of more consistent visualization of C6 vs. C7. Less commonly used, the HPA method involves drawing parallel lines along the posterior aspect of the vertebral body walls of C2 to C7 and summing each segmental angle for a total CL angle, while the JPA lines method only uses lines tangent to the C2 and C7 posterior vertebral walls as an estimate for CL.
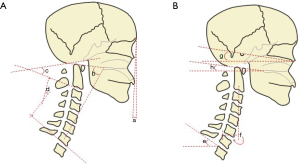
The Ocipput-C2 (Oc-C2) and C1-C2 CAs are two measurements that evaluate the alignment of the most cranial portion of the spine. The Oc-C2 angle (Figure 2A, angle c) is measured by the angle subtended by the McGregor line of sight (a line connecting the posterior edge of the hard palate to the most caudal point of the occiput) and a parallel line along the inferior endplate of C2, while the C1-C2 angle is measured using the previously mentioned C1 anterior tubercle-posterior C1 ring and C2 inferior endplate parallel line (10).
Horizontal gaze is an essential part of a human’s everyday interaction with his/her surrounding environment, while helping to regulate dynamic stability. As such, the chin-brow vertical angle (CBVA, Figure 2A, angle a) has been a commonly used tool to evaluate a patient’s horizontal gaze. It is measured as the angle formed from the line connecting the anterior edge of the forehead and chin to the vertical. However, the CBVA has not always been a reliable marker on cervical radiography due to the poor visibility of the anterior skull. Moses et al. (11) demonstrated that, in such cases, the McGregor line of slope (McGS, Figure 2B, angle h) and the slope of line of sight (SLS, Figure 2B, angle g) can act as a surrogate marker for assessment of horizontal gaze. McGS is the angle between the aforementioned Macgregor line and horizontal, while the SLS is the angle between the horizontal and Frankfort’s plane (a line connecting lower aspect of the orbit with the upper aspect of the external auditory canal). Additional measurements that are used to describe cervical alignment are the C7 and T1 slope (T1S, Figure 2B, angle e), measured from the superior endplate of the respective level to the horizontal. The C7 slope helps determine if the cervical spine is lordotic or kyphotic.
Craniocervical orientation can be assessed using the parameters of cranial and cervical tilt. Cervical tilt is measured as the angle between the perpendicular line from the center of the T1 upper endplate and the line from the center of the T1 upper endplate to the tip of the dens. Cranial tilt is measured as the angle between the line from the center of the T1 upper endplate to the dens and the vertical line through the center of the T1 upper endplate. The relationship between cranial and cervical tilt and T1S is described by the following formula: T1S = cervical tilt + cranial tilt (12).
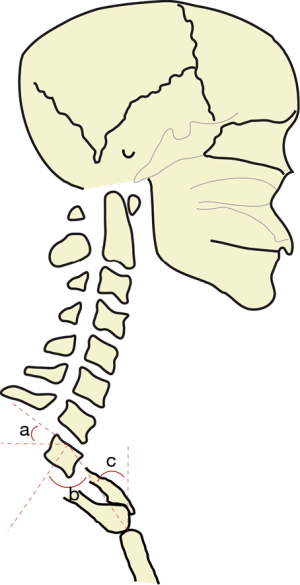
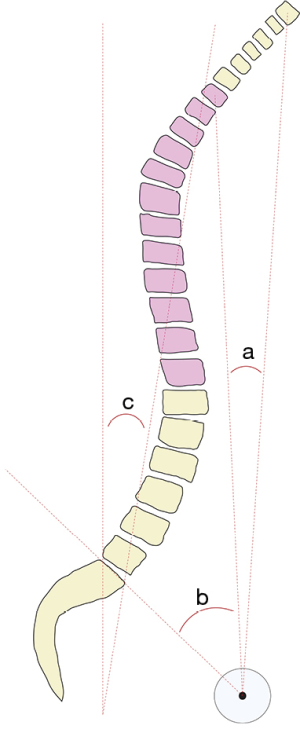
While inherent pathology (i.e., degenerative disease) of the cervical spine can lead to sagittal plain deformity, malalignment of the supporting thoracic inlet (composed of the T1 vertebral body, bilateral 1st ribs, and manubrium) can be a potential cause for cervical malalignment or compensation. Lee et al. (13) described this relationship using the formula: thoracic inlet angle (TIA) = neck tilt (NT) + T1S. The TIA (Figure 3, angle b) can be measured as the angle formed between a perpendicular line originating from the mid T1 endplate and a line extending from the center of the T1 upper endplate to the upper end of the sternum. The NT angle (Figure 3, angle c) is measured between the line extending from the center of the T1 upper endplate to the upper end of the sternum and a vertical line from the upper end of the sternum (14).
The sagittal vertical axis (SVA, Figure 4, distance c) is a common measure to help characterize global spine alignment with respect to the sacrum. It is defined as the distance between a vertical line extending from the centroid of C7 (the plumb line) to the posterior superior corner of S1 (14). For a more regional assessment of alignment, a similar approach can be used via the cervical sagittal vertical axis (cSVA, Figure 2B, distance f), which is a line drawn from the C2 plumb line to the posterior superior corner of C7. When used in combination with the T1S, the cSVA can provide a useful parameter to quantify subaxial CL for maintenance of cranial center-of-gravity and horizontal gaze (15). Recently, Goldschmidt et al. (16) established an empirical relationship between the T1S, CL, and cervical SVA using the formula:
|
| [1] |
where cervical height (CH) is the vertical distance from the anterior aspect of T1 to the upper endplate of C2.
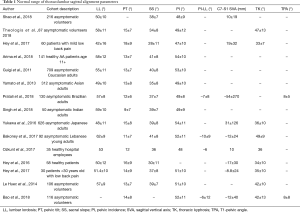
The thoracic spine is the least mobile segment of the functional spine, however parameters such as the T1-pelvic angle (TPA) can still provide insight into the global alignment over the pelvis. The TPA is often defined as the angle between the line travelling from the centroid of T1 to the center of the femoral head and a line from the femoral head to the centroid of the S1 endplate with a normative range of 17.3°±13.1° (further variations in TPA angle are noted in Table 1). In contrast to the SVA, the TPA does not vary upon pelvic retroversion when the patient is standing (17).
Full table
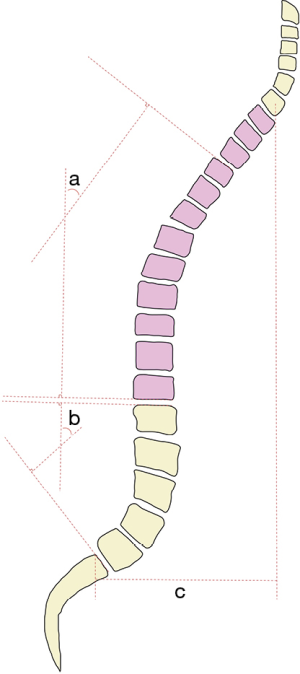
The lumbar spine directly works in concert with the sacrum and pelvis to support the body’s weight, thus highlighting the importance of pelvic morphology to lumbosacral alignment. Three common parameters of measurement to assess lumbosacral alignment are the pelvic incidence (PI, Figure 5, angle c), pelvic tilt (PT, Figure 5, angle b), and sacral slope (SS, Figure 5, angle a), following the formula: PI = PT + SS. PI is a morphological parameter (unaffected by age/position) to help assess the orientation of the sacrum within the pelvis. It is commonly measured by the angle between the line drawn from the center of the sacral endplate to the center of the femoral head axis and the line perpendicular to the sacral endplate (18). PT is a positional parameter that helps assess pelvic rotation in relation to the femoral head axis. It is measured as the angle between a line drawn from the center of the sacral endplate to the center of the femoral head axis and a vertical line drawn from the center of the femoral head axis. SS is also a positional parameter that helps assess the sacrum in relation the horizontal. It is measured as the angle between a line drawn along the sacral endplate and the horizontal measures from the posterior superior sacral endplate. It is important to differentiate a large PT angle which may be a normal physiologic variant versus a sign of compensation in a patient with a small PI. Yilgor et al. (19) proposed a solution by measuring the relative pelvic version (RPV) using the formula: RPV = SS – (0.59× PI) +9. This formula allows a more individualized measurement parameter for a wide variety of PI values. Lafage et al. (20) noted in her study of lumbopelvic sagittal parameters that T1-Spinopelvic inclination (TSPI) most correlated with patient outcomes, followed by SVA and PT. The consensus among surgeons is to strive to maintain an SVA <50 mm in adult spinal deformity (ASD) patients for improved healthcare-related quality of life (HRQOL). By doing so, the C7 plumb line is brought behind the femoral head axis to prevent the patient from falling forward. The correlation of spinopelvic alignment with patient outcomes allows physicians to make more effective decisions if surgical intervention is required and aim to achieve appropriate intraoperative thresholds during surgical planning.
Regional lordosis of the lumbar spine, called the lumbar lordosis (LL, Figure 4, angle b), is calculated as the angle between the lines subtending the superior endplate of L1 and inferior endplate of L5. In conjunction with the PI, LL provides a commonly utilized spinopelvic parameter to help predict recruitment of compensatory mechanisms through the PI-LL mismatch, calculated as the difference between the two angles. Similarly, TK (Figure 4, angle a) provides an evaluation of the regional alignment of thoracic spine, measured as the angle subtended by the line from the superior endplate of T4 and the inferior endplate of T12.
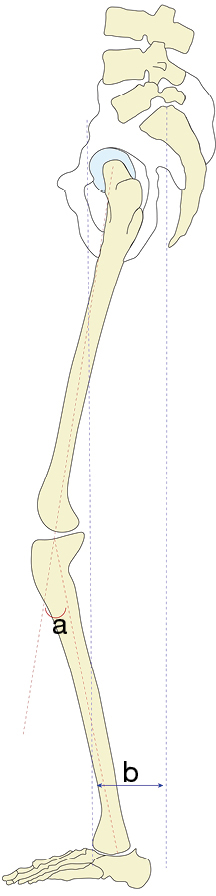
Below the spine and pelvis, knee flexion angle (KFA, Figure 6, angle a) and pelvic shift (PS, Figure 6, distance b) can be used to determine if a patient is compensating for sagittal imbalance with their lower limbs. Knee angle measures knee flexion while standing as the angle between the mechanical axes of the femur and tibia (21). PS is similar to SVA, measuring the horizontal distance between the S1 plum line and the anterior surface of the distal tibia.
While the importance of regional and global alignment parameters cannot be understated, the effect that they have on each other is of particular importance when considering ASD and its impact on cervical alignment. To assess such changes, several alignment parameters have been described (22-24): craniocervical angle (CCA, Figure 2B, angle b), cervico-thoracic pelvic angle (CTPA, Figure 7, angle a), TPA (Figure 7, angle b), C2 tilt (C2T, Figure 8, angle a), and C2-T1 PT (C2PT, Figure 8, angle b). The CCA allows for assessment of cervical alignment and upper cervical compensation, measured as the angle between McGregor’s line and the line from the centroid of C7 to the hard palate. CTPA is the angle between the line from the femoral head axis to centroid of T1 and the line from the femoral head axis to the centroid of C2. TPA, on the other hand, is the angle between the line drawn from the femoral head axis to the centroid of T1 and the line drawn from the femoral head axis to the superior sacral endplate. CTPA has been shown to correlate with the C2–C7 plumb line as a global analog of cervical sagittal balance, while both CTPA and TPA parameters have been shown to be relatively precise representations of cervical and thoracolumbar deformities, respectively. The C2T and C2PT provide radiographic measures of regional and global spinal deformity respectively. C2T is measured as the angle between the vertical and the line tangent to the posterior edge of C2. C2PT is measured as the angle subtended by the line tangent to the posterior edge of C2 and the line extending from the femoral head axis to the superior sacral endplate. Measurements such as these underscore the importance of a full length standing radiographic assessment for preoperative surgical planning.
Variations in cervical spine alignment/parameters
While the foundational anatomy of each human being is the same, there exist a wide variety of normal variants. These differences can exist depending on the time of day, postural changes due to aging, gender, ethnicity, weight, and much more.
One of the well-accepted sagittal alignment classification systems proposed over the last decade was the Roussouly classification (25). The author’s original study aimed to classify normal variations in sagittal alignment of the spine by categorizing them into one of four types based on the relationship between sacral orientation and LL:
Type 1: SS <35° and the apex of LL located at the center of L5. Consistent with significant kyphosis of the TLJ with a short arc of lordosis.
Type 2: SS <35° and the apex of LL located at the base of L4. The entire spine is hypolordotic and hypokyphotic.
Type 3: 35°< SS <45° and the apex of LL is located at the center of L4. This type is consistent with a well-balanced spine.
Type 4: SS >45° and the apex of LL located at the base of L3. This is consistent with significant lordosis and compensatory TK.
Their results showed that significant variability with regards to the sagittal alignment of the spine. They found that the mean PI was 51.91°±10.7, SS 39.9°±8.2, PT 11.9°±6.5, and LL 61.4°±9.7. Although the average lumbar inflection point was at the center of L1, the transition occurred as proximal as T10 and distally at L4 in some patients. Recently, Theologis et al. (26) expanded the study to explore the effect of thoracolumbar alignment on cervical compensation. Their group determined normative cervical parameters/variations according to the Roussouly classification. This included the following: CBVA –1° (±9°), Oc-C2 28° (±9°), C2-C7 CA 11° (±14°), cSVA 21 mm (±9 mm), T1S 25° (±9°), and C6-T4 kyphotic angle 4° (±8°). Between groups there was no significant difference noted in cervical alignment parameters, except the C2-C7 CA. The patient populations of both the Roussouly and Theologis study included normal, asymptomatic patients and, thus these measurements can be considered average values and deviations.
In patients with noted cervical kyphosis and symptoms of neurologic compromise or pain, recent studies have provided guidance on the consideration of alignment on surgical planning. The overall goal of surgery aims to relieve pain, preserve or improve neurologic function, and restore alignment. Thus, in addition to decompression of neural structures and adequate fusion, current literature (27,28) advocates restoration of patient specific optimum alignment with restoration of horizontal gaze, a subaxial CL less than 15°, C2-C7 SVA less than 40 mm, and an acceptable CBVA of –10° to +20°.
In addition, studies have shown that the male and female spine are subjected to differing biomechanical forces and loads that result in spinal alignments that may differ from one another. To date, no significant difference has been noted between genders in CL, TK, LL, or lumbosacral/pelvic parameters. Janssen et al. (29), however, revealed the female spine was significantly different from the male spine as a whole (i.e., T1-L5 sagittal spinal inclination) and regionally (high thoracic and TLJ) with a predisposed dorsal inclination (Figure 7, angle c). As such, these patients are subject to different biomechanical loading with decreased rotational stability in the high thoracic and TLJ regions.
In terms of body habitus, Jalai et al. (30) found that obese patients had similar regional spinal parameters as non-obese patients, but obesity did correlate with higher SVA, TK, and global sagittal angle (GSA). Biomechanically, the increased weight-bearing forces in obese patients can lead to greater use of lower limb compensatory mechanisms (31). Classically, increased posterior tilt is a common method of compensation for an increased SVA. A shift of the center of gravity in obese patients can lead to increased recruitment of the lower limb musculature to help reinforce compensatory pelvic retroversion. In addition, the study showed that the most relevant compensatory mechanisms were knee flexion and posterior PT which is often reflected in an increased PI-LL mismatch.
Although currently literature is limited on the demographic and longitudinal variations of cervical alignment, the relevancy and effect of variations in thoracolumbar-sacral-pelvic axis cannot be underemphasized. The human body aims to maintain a certain posture and cervical compensation may differ among patients depending on the time of day, ethnicity, spine flexibility, degenerative changes etc. For instance, in patients with a significant loss of LL and increased PI-LL mismatch, compensation occurs with either lordosis of mobile spine segments, change in PT, and/or recruitment of lower extremity adaptive changes. Certain cases, however, prevent sufficient pelvic or lower extremity compensation to allow for adequate restoration of global alignment, leading to changes in cervical alignment and the potential for a symptomatic cervical deformity (CD). Tables 1,2 describe the range of normal variations in cervical and thoracolumbar alignment parameters.
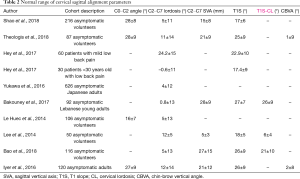
Full table
Age-related changes in cervical spine alignment
In understanding normal spinal alignment, it is important to consider the normative changes in spinal alignment with aging. This concept is important to review and understand to help distinguish normal vs. pathological variants in regional/global alignment. This information is extremely valuable in the diagnosis of spinal deformity and subsequent surgical treatment.
While age-based normative values of spine alignment have been well studied in the lumbosacral spine, few studies have focused on the cervical spine. In 1997, Hardacker et al. (32) were the first study to measure total segmental cervical alignment in asymptomatic individuals. While there was no stratification of the sample by age, it paved the way to an increased awareness of the importance of normative radiologic measures of the cervical spine. One of the most comprehensive studies recently to review cervical alignment in the North American population with increasing age was done by Iorio et al. (33). Their group conducted a retrospective study of 118 asymptomatic individuals who underwent biplanar imaging and measured parameters including C0-C2 CA, C2-C7 CL, C0-C7 CL, TS-CL mismatch, SLS/McGS, and more. Their results showed demonstrated a significant change in cervical sagittal parameters, such as C2–C7 CA, C0–C7 CL, and T1S angle with aging. The C0–C2 angle did not change with age or contribute significantly to total CL, attributing the increase in C0–C7 lordosis to an increase in the C2–C7 CA. T1S increased also with an increase in the C2–7 CA. While horizontal gaze parameters (CBVA, SLS, McGS) were significant different between age groups, there were no identifiable trends observed. Their results showed that the C2–C7 CL increased an average of 14° from an age <35 (–2.2°±13.8°) to ≥65 (11.8°±12.1°). In addition, the T1S increased by an average of 10.5° from an age <35 (22.0°±8.1°) to ≥65 (32.5°±11.5°). The global alignment parameter C7–S1 SVA showed an overall mean increase of 62.7 mm from <35 (–35.5±34.4 mm) to ≥65 (27.2±51.3 mm).
As such, the increased T1S with age represents a compensatory response to the increased cSVA and PI-LL mismatch in the setting of a relatively fixed TK. Increased C2-C7 SVA beyond 40 mm has been associated with poor patient outcomes, thus compensation via increased CL may be seen as a compensatory measure to prevent increased cervical sagittal offset (cSVA).
Park et al. (15) conducted a similar review of cervical parameters in asymptomatic patients in Korea, however they stratified their patients into two age groups: age 20–29 years and age >60 years. Although their analysis of cervical parameters was not comprehensive, it gave insight into two different age cohorts. In particular, their results showed a similar increase in NT and TIA with increasing age. With increasing T1S, the center of gravity of the head translates more anteriorly with reinforced cervical lordotic compensation. Thus, they showed that an increased T1S resulted in increased CL and an increased CL was associated with a decreased cSVA due to compensation.
Yukawa et al. (34) and Liu et al. (35) explored age-related values in asymptomatic Japanese and Chinese individuals, respectively finding similar increase in C2-7 CA with age. Liu et al. also found significant increases in NT, T1S, and TIA with age. A study by Gore et al. (36) showed that changes in CL differed between men and women. In particular, while CL increased in men and women during their 30 and 40 s, women experienced a decreased overall CL during this age range compared to men. Factors such as age, gender, BMI, baseline posture may all have a greater effect on cervical alignment than is realized, thus further investigation is necessary to investigate their role in surgical planning if necessary.
Tables 3,4 layout the range of normal variations in cervical and thoracolumbar alignment parameters stratified by age and sex.
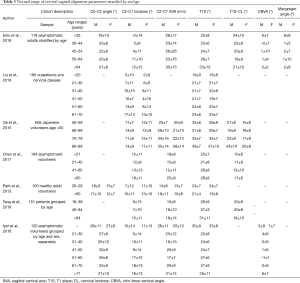
Full table
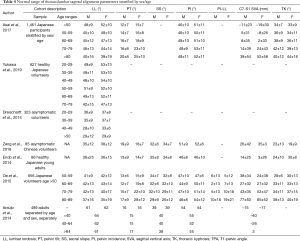
Full table
Pathological changes cervical spine alignment
Pathologic spinal sagittal alignment should be distinguished from normative variants. While one method would be to study normative values/variations and call any unexpected deviation a pathological anomaly, another method involves understanding the changes that occur in sagittal alignment as a natural progression of degenerative disease or deformity.
As previously described, the Roussouly classification aims to categorize normal spine balance based on SS and spinal shape. This allows for localization of high zones of shear stress; increased lordotic curvature correlates to increased contact forces on the posterior elements (facet joints), whereas a decreased lordotic curve correlates to increased contact forces on the anterior elements (vertebral body/disc). Degenerative disease however makes it difficult to predict the manner of compensation above, at, and below the level of degeneration.
One study by Sebaaly et al. (37) aimed to understand the possible evolution of sagittal alignment of the degenerative spine in the context of the Rousouly classification. The authors noted that with progressive spinal degeneration and increasing TK, each type of curve compensates differently:
- Roussouly type 1:
- Roussouly type 2:
- Roussouly type 3:
- Roussouly type 4:
Compensation can occur either below the lumbar spine (accentuated type 1) or compensation mechanisms are overcome and LL decreases (global kyphosis with low PI);
Compensation occurs with a small increase in LL (type 1 Roussouly) or no change in LL. If there is no change in LL, then either thoracic hypokyphosis compensation occurs (lumbar kyphosis) or no compensation (global kyphosis);
Compensation occurs in the caudal mobile segment with loss of TK (false retroverted type 2). If it is not mobile enough, then thoracic hypokyphosis occurs (false type 2 + TK), with compensation via pelvic retroversion (global kyphosis);
Compensation occurs with a decrease in LL (type 3) with subsequent changes similar to the type 3 spine above, ultimately ending in maximal pelvic retroversion (global kyphosis).
While this study provides valuable insight into the changes which occur with thoracolumbar sagittal alignment with degenerative disease, indirectly it also gives insight into the affect it has on the cervical spine by ultimately affecting global alignment.
Cervical spondylotic myelopathy (CSM) is the most common neurologic disorder to affect the adult population (38). The most commonly affected level of disc degeneration occurs at the level of C5–6, followed by C4–5 or C6–7. In the elderly population, however the more common location is C3–4. One study by Yoshida et al. (39) sough to compare spinal alignment in the context of CSM. They conducted a prospective study of 88 surgically treated patients with CSM divided into three groups based on SVA and CL: type 1a (SVA <50 mm, CL >0°), type 1b (SVA <50 mm, CL ≥0°), and type II (SVA >50 mm). Their results showed that C5–6 pathology occurred at an average age of 56 years, with a mean (± SD) SVA, CL, TK, and T1S of 9.17 mm (±30.0 mm), 12.1° (±7.3°), 36.4° (±10.7°), and 25.3° (±6.9°), respectively. Furthermore, C3–4 pathology correlated with an average age of 66 years and an SVA, CL, TK, and T1S of 52.1 mm (±37.1 mm), 9.4° (±7.3°), 45.2° (±13.8°), and 30.4° (±9.8°), respectively. C3–4 pathology was associated with an increased cranial lordosis ratio (C2–4/C5–7 angle). The study found that in patients with CSM, degenerative changes of the lower cervical segments lead to upper cervical compensation to maintain horizontal gaze and balance. Type II CSM patients were also older (66.2±10.2 years) with an increased T1S-CL (21.2°±7.4°) and C2–7 SVA (27.7±12.0 mm).
In CSM patients, surgical planning is guided by the location of neural compression, number of levels involved and spinal alignment. An anterior decompression and fusion is appropriate in the presence of anterior compression, a cervical kyphotic alignment, or compression in general at three levels or less. A posterior decompression is more appropriate for posterior compression, adequate CL, or more than three-level involvement in a straight or lordotic cervical spine. Yoshida et al. recommended that in patients with severe cervical compensation or false lordosis, the surgeon should avoid performing a posterior approach to prevent progressive malalignment and/or loss of horizontal gaze. Thus, global spine alignment should be considered when planning a surgical approach for CSM patients, giving careful consideration not only to cervical and cervicothoracic measurement parameters, but also to global spine alignment.
In patients with ankylosing spondylitis, a chin-on-chest deformity can be a disabling deformity that causes problems with chewing, swallowing, neck pain, and horizontal gaze. A study by Belanger et al. (40) showed that in patients with a chin-on-chest deformity, an extension osteotomy and cervicothoracic arthrodesis helped improve sagittal alignment by 38° with similar studies reporting sagittal corrections of up to 54°. Improvement in horizontal gaze also helped improve neck pain and neurologic symptoms.
Adult CD patients have been well documented to report poor HRQOL outcomes and experience negative health consequences. Previous studies (41) have established that in the presence of thoracolumbar deformity, a T1S-CL mismatch greater than 20° is associated with a cSVA greater than 40 mm, the threshold noted to denote CD. Protopsaltis et al. (23) conducted a prospective, multicenter study of 71 adult CD patients (45 with primary cervical and 26 with cervico-thoracic junction deformity). Their results showed that failure to correct cSVA was associated with predisposing factors such as the need for revision surgery, a worse preoperative C2PT angle, and the presence of a concurrent thoracolumbar deformity. Furthermore, failure to correct T1S-CL mismatch was associated with worse preoperative cervical kyphosis and C2PT, as well as worse postoperative C2 slope and C2PT. Their results demonstrated the inherent difficulty in improving CD in the revision setting. Successful correction of T1S-CL was associated with multi-level anterior fusions, and successful.
Cervical spine alignment and post-operative complications
Recently, there has been growing interest in the use of sagittal alignment parameters as predictors of post-operative complications, whether local to the site of the surgery or elsewhere in the spine. Information such as this could provide an additional point of evaluation when considering patients for operative management.
Adjacent segment pathology (ASP) has been a debated topic in the field spine surgery for years with some arguing that it as the result of the natural progression of the spine with age, while others claim it to be a result of surgical intervention. In either case, terminology has been used interchangeably between clinical adjacent segment disease (cASD) and radiographic adjacent segment degeneration (rASD), both encompassed under the term “adjacent segment pathology” (42). Radiographic ASD includes the presence of X-ray findings without clinical symptoms (i.e., pain/numbness/etc.), in contrast to clinical ASD which also presents with the presence of clinical symptoms. Current literature estimates the incidence of cervical rASD to range from 17.8–49.9% and cASD to range from 4.8–7.8%, while the incidence of lumbar rASD and cASD have been estimated to range from 21.3–31.9% and 6.4–10.3%, respectively (43).
Multiple cervical spine studies have looked at relationships between cervical alignment and ASP. Preoperatively, Song et al. (44) conducted a mid-term retrospective study of 1-level anterior cervical discectomy and fusion (ACDF) patients and found no significance related to CL and the development of ASP. In the postoperative setting, however, multiple studies have shown significant relationships between sagittal parameters and ASP. More than a decade ago, Katsuura et al. (45) conducted a retrospective study of 91 patients who underwent multi-level ACDF to determine the effect of postoperative cervical alignment on rASD. Their results showed that patients with a postoperative kyphotic or sigmoid cervical alignment were more likely to present radiographically with degenerative changes at adjacent levels. One theory behind this is that the decreased CL after fusion results in an abnormal distribution of stress on the adjacent segments. The lordotic curve of the cervical spine allows for load distribution to be divided between the posterior (articular processes and facet joints) and anterior cervical spine (64% vs. 36%). However, a decreased lordosis after surgery can shift the load predominantly onto the anterior spinal column and lead to ASP.
Recent studies (46) have shown that patients with an increased T1S and decreased CL/SL values are more predisposed to developing ASP. A study by Liu et al. (47) examined the effect cervical sagittal alignment on adjacent level ossification development (ALOD) in patients who underwent ACDF. Compared to patients with no complications, the patients with ALOD showed a decreased CL (8.8° vs. 13.0°), cervical tilt (18.3° vs. 22.3°), and T1S (21.9° vs. 26.2°). These findings showed that maintaining a lordotic cervical curve postoperatively was associated with a decreased risk of occurrence of ALOD. As such, recent studies on ASP have shown that postoperative malalignment can be a predictor of future ASD and complications.
In 2018, Park et al. (48) carried out a retrospective study of 614 patients who underwent 1-/multi-level ACDF surgery for degenerative disease to examine whether postoperative cervical sagittal alignment was a predictor of cASD and need for operative management. Their study showed that cASD was significantly associated with an increased proportion of Katsuura straight cervical spine curve patterns and decreased C7 and T1Ss. Furthermore, their results showed that cASD requiring surgery had no relationship with the fused segment or the overall cervical alignment. Faldini et al. (49) conducted a retrospective cohort study exploring postoperative sagittal alignment as a predictor of rASD. Their findings showed rASD was present in 61% of patients fused in neutral or kyphotic alignment versus 27% of patients fused in lordotic alignment.
Cervical spine alignment and PRO
Studies over the last several years on the subject of spinal alignment have given significant insight into the effects of alignment on HRQOL.
With respect to the cervical spine in the preoperative setting, studies (50,51) have shown that an increased CL, T1S, and T1-CL are generally predictors of poor HRQOL outcomes in patients undergoing future operative management. As T1 is the main segment that bears the weight of the cranium, increased stress over time can lead to greater T1 tilting to maintain horizontal gaze, with CL increasing as an additional compensatory mechanism. Another theory, however, argues that the increased T1S and CL may be more attributable to the increased TK that results with aging. Regardless, increases in these global and regional cervical parameters have been linked to poor outcomes in asymptomatic and myelopathic patients alike. Interestingly, Iyer et al. (52) also showed that outcomes in radiculopathy patients did not have significant correlations with sagittal parameters and there was a negative correlation between cSVA and neck disability index (NDI).
ACDF procedures are one of the most common surgeries conducted on patients with significant cervical degenerative disc disease. Siasios et al. (53) conducted a retrospective review of single level ACDF patients to assess the impact of cervical sagittal parameters on postoperative functionality. All patients reported better functionality scores, with a significant increase in upper CL (C1-2 angle). Previous studies (52,54) have shown that an ACDF can affect changes at the operative level, as well as cervical segments superior to the operative level. The resulting increase in C1-C2 lordosis and CL is related to improved patient outcomes. The use of lordotically shaped allografts did not increase cervical segmental alignment or improve PRO.
In post-operative multi-level ACDF patients at 6 months, Katsuura et al. (55) found a significant increase in CL and a weakly positive correlation of CL with an improvement in SVA. While further studies need to be conducted, an increasing SVA has been associated with poor clinical outcomes in multiple studies. Tang et al. (56) reported on a cohort of 113 patients who underwent posterior cervical decompression and fusions. A cSVA greater than 40 mm was found to be a predictor of poor outcomes.
In the case of multi-level cervical myelopathy, some studies have shown that an ACDF preserves or improves CL better than an open-door laminoplasty, while others claim no significant difference between the two surgeries. Liang et al. (57) prospectively investigated 60 patients who underwent either an ACDF or cervical laminoplasty. Their results showed that multi-level ACDF exhibited a poor lordosis-preserving ability compared to the laminoplasty group. If fact, on follow up, CL decreased over time in the ACDF group leading to similar PRO between the two groups. Passias et al. (58) conducted a retrospective review of 70 CD patients to determine whether accomplishing cervical alignment goals or clinical improvement was more predictive of postoperative status. Their results showed an association between clinical symptoms and 1-year patient-reported outcome measures (PROM), with no significant relationship between cervical sagittal parameters and PRO. The authors also found that C2-S1 SVA and C7-S1 SVA significantly correlated with multiple QOL outcomes demonstrating how global sagittal alignment, not just cervical alignment, is important in improving clinical outcomes. The NDI score also correlated with PT and horizontal gaze parameters (McGregors Slope, C0 slope, C1 slope).
Conclusions
Over the past decade, our understanding of regional and global spine alignment has continued to evolve. Different parameters outlined above have been developed to help guide effective surgical techniques. Cervical spine alignment is a critically important component of surgical planning. Understanding physiologic variations, age related changes and pathological malalignment is extremely important when managing a symptomatic patient with cervical degenerative disk disease. These parameters have an impact not only on radiographic outcomes, but more importantly on PROM. Surgical treatment of the cervical spine should take into account not only regional but global spinal alignment. Recommendations in the future will deal with the potential need for full body lateral imaging to completely understand spinal alignment. At this time a clear consensus on minimum radiographic imaging parameters have not been established in the routine management of cervical degenerative disk disease.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dubousset J. Three-dimensional analysis of the scoliotic deformity. Pediatr Spine Princ Pract 1994.
- Ganau M, Zewude R, Fehlings MG. Functional anatomy of the spinal cord. In: Kaiser MG, Haid RW, Shaffrey CI, et al. editors. Degenerative cervical myelopathy and radiculopathy. Cham: Springer International Publishing, 2019:3-12.
- Jun BY. Anatomic study for ideal and safe posterior C1-C2 transarticular screw fixation. Spine (Phila Pa 1976) 1998;23:1703-7. [Crossref] [PubMed]
- Bell GH, Dunbar O, Beck JS, et al. Variations in strength of vertebrae with age and their relation to osteoporosis. Calcif Tissue Res 1967;1:75-86. [Crossref] [PubMed]
- Macintosh JE, Bogduk N. The morphology of the lumbar erector spinae. Spine (Phila Pa 1976) 1987;12:658-68. [Crossref] [PubMed]
- Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024-29. [Crossref] [PubMed]
- Lee BS, Benzel EC. Cervical spine biomechanics. In: Kaiser MG, Haid RW, Shaffrey CI, et al. editors. Degenerative cervical myelopathy and radiculopathy. Cham: Springer International Publishing, 2019:13-28.
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59. [Crossref] [PubMed]
- Zhang J, Buser Z, Abedi A, et al. Can C2-6 Cobb angle replace C2-7 Cobb angle?: an analysis of cervical kinetic magnetic resonance images and X-rays. Spine (Phila Pa 1976) 2019;44:240-5. [Crossref] [PubMed]
- Diebo BG, Challier V, Henry JK, et al. Predicting cervical alignment required to maintain horizontal gaze based on global spinal alignment. Spine (Phila Pa 1976) 2016;41:1795-800. [Crossref] [PubMed]
- Moses MJ, Tishelman JC, Zhou PL, et al. McGregor’s slope and slope of line of sight: two surrogate markers for Chin-Brow vertical angle in the setting of cervical spine pathology. Spine J 2019;19:1512-7. [Crossref] [PubMed]
- Weng C, Wang J, Tuchman A, et al. Influence of T1 slope on the cervical sagittal balance in degenerative cervical spine: an analysis using kinematic MRI. Spine (Phila Pa 1976) 2016;41:185-90. [Crossref] [PubMed]
- Lee SH, Kim KT, Seo EM, et al. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech 2012;25:E41-7. [Crossref] [PubMed]
- Tuchman A, Higgins DMO. Cervical alignment and sagittal balance. In: Kaiser MG, Haid RW, Shaffrey CI, et al. editors. Degenerative cervical myelopathy and radiculopathy. Cham: Springer International Publishing, 2019:29-36.
- Park JH, Cho CB, Song JH, et al. T1 slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J Korean Neurosurg Soc 2013;53:356-9. [Crossref] [PubMed]
- Goldschmidt E, Angriman F, Agarwal N, et al. A new piece of the puzzle to understand cervical sagittal alignment: utilizing a novel angle δ to describe the relationship among T1 vertebral body slope, cervical lordosis, and cervical sagittal alignment. Neurosurgery 2020;86:446-51. [PubMed]
- Protopsaltis T, Schwab F, Bronsard N, et al. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am 2014;96:1631-40. [Crossref] [PubMed]
- Tormenti MJ, McLaughlin MR. An overview of various surgical approaches. In: Kaiser MG, Haid RW, Shaffrey CI, et al. editors. Degenerative cervical myelopathy and radiculopathy. Cham: Springer International Publishing, 2019:185-94.
- Yilgor C, Yavuz Y, Sogunmez N, et al. Relative pelvic version: an individualized pelvic incidence-based proportional parameter that quantifies pelvic version more precisely than pelvic tilt. Spine J 2018;18:1787-97. [Crossref] [PubMed]
- Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599-606. [Crossref] [PubMed]
- Lee CS, Park SJ, Chung SS, Lee KH. The effect of simulated knee flexion on sagittal spinal alignment: novel interpretation of spinopelvic alignment. Eur Spine J. 2013;22:1059-65. [Crossref] [PubMed]
- Protopsaltis T, Bronsard N, Soroceanu A, et al. Cervical sagittal deformity develops after PJK in adult thoracolumbar deformity correction: radiographic analysis utilizing a novel global sagittal angular parameter, the CTPA. Eur Spine J 2017;26:1111-20. [Crossref] [PubMed]
- Protopsaltis TS, Ramchandran S, Hamilton DK, et al. Analysis of successful versus failed radiographic outcomes after cervical deformity surgery. Spine (Phila Pa 1976) 2018;43:E773-81. [Crossref] [PubMed]
- Protopsaltis TS, Lafage R, Vira S, et al. Novel angular measures of cervical deformity account for upper cervical compensation and sagittal alignment. Clin Spine Surg 2017;30:E959-67. [Crossref] [PubMed]
- Roussouly P, Gollogly S, Berthonnaud E, et al. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346-53. [Crossref] [PubMed]
- Theologis AA, Iyer S, Lenke LG, et al. Cervical and cervicothoracic sagittal alignment according to roussouly thoracolumbar subtypes. Spine (Phila Pa 1976) 2019;44:E634-9. [Crossref] [PubMed]
- Iyer S, Lenke LG, Nemani VM, et al. Variations in occipitocervical and cervicothoracic alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976) 2016;41:1837-44. [Crossref] [PubMed]
- Song K, Su X, Zhang Y, et al. Optimal chin-brow vertical angle for sagittal visual fields in ankylosing spondylitis kyphosis. Eur Spine J 2016;25:2596-604. [Crossref] [PubMed]
- Janssen MM, Drevelle X, Humbert L, et al. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine (Phila Pa 1976) 2009;34:E826-32. [Crossref] [PubMed]
- Jalai CM, Diebo BG, Cruz DL, et al. The impact of obesity on compensatory mechanisms in response to progressive sagittal malalignment. Spine J 2017;17:681-8. [Crossref] [PubMed]
- Popovich JM, Welcher JB, Hedman TP, et al. Lumbar facet joint and intervertebral disc loading during simulated pelvic obliquity. Spine J 2013;13:1581-9. [Crossref] [PubMed]
- Hardacker JW, Shuford RF, Capicotto PN, et al. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 1997;22:1472-80. [Crossref] [PubMed]
- Iorio J, Lafage V, Lafage R, et al. The effect of aging on cervical parameters in a normative north American population. Global Spine J 2018;8:709-15. [Crossref] [PubMed]
- Yukawa Y, Kato F, Suda K, et al. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: radiographic data from over 1,200 asymptomatic subjects. Eur Spine J 2012;21:1492-8. [Crossref] [PubMed]
- Liu J, Liu P, Ma Z, et al. The effects of aging on the profile of the cervical spine. Medicine (Baltimore) 2019;98:e14425. [Crossref] [PubMed]
- Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976) 1986;11:521-4. [Crossref] [PubMed]
- Sebaaly A, Grobost P, Mallam L, et al. Description of the sagittal alignment of the degenerative human spine. Eur Spine J 2018;27:489-96. [Crossref] [PubMed]
- de Oliveira Vilaça C, Orsini M, Leite MA, et al. Cervical Spondylotic Myelopathy: What the Neurologist Should Know. Neurol Int 2016;8:6330. [PubMed]
- Yoshida G, Alzakri A, Pointillart V, et al. Global spinal alignment in patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2018;43:E154-62. [Crossref] [PubMed]
- Belanger TA, Milam RA, Roh JS, et al. Cervicothoracic extension osteotomy for chin-on-chest deformity in ankylosing spondylitis. J Bone Joint Surg Am 2005;87:1732-8. [PubMed]
- Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673-83. [Crossref] [PubMed]
- Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 2008;33:1701-7. [Crossref] [PubMed]
- Park P, Garton HJ, Gala VC, et al. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29:1938-44. [Crossref] [PubMed]
- Song KJ, Choi BW, Kim JK. Adjacent segment pathology following anterior decompression and fusion using cage and plate for the treatment of degenerative cervical spinal diseases. Asian Spine J 2014;8:720-8. [Crossref] [PubMed]
- Katsuura A, Hukuda S, Saruhashi Y, et al. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 2001;10:320-4. [Crossref] [PubMed]
- Yang P, Li Y, Li J, et al. Impact of T1 slope on surgical and adjacent segment degeneration after Bryan cervical disc arthroplasty. Ther Clin Risk Manag 2017;13:1119-25. [Crossref] [PubMed]
- Liu W, Rong Y, Chen J, et al. Cervical sagittal alignment as a predictor of adjacent-level ossification development. J Pain Res 2018;11:1359-66. [Crossref] [PubMed]
- Park MS, Kelly MP, Lee DH, et al. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J 2014;14:1228-34. [Crossref] [PubMed]
- Faldini C, Pagkrati S, Leonetti D, et al. Sagittal segmental alignment as predictor of adjacent-level degeneration after a cloward procedure. Clin Orthop Relat Res 2011;469:674-81. [Crossref] [PubMed]
- Bess S, Protopsaltis TS, Lafage V, et al. clinical and radiographic evaluation of adult spinal deformity. Clin Spine Surg 2016;29:6-16. [Crossref] [PubMed]
- Lee JS, Son DW, Lee SH, et al. The predictable factors of the postoperative kyphotic change of sagittal alignment of the cervical spine after the laminoplasty. J Korean Neurosurg Soc 2017;60:577-83. [Crossref] [PubMed]
- Iyer S, Nemani VM, Nguyen J, et al. Impact of cervical sagittal alignment parameters on neck disability. Spine (Phila Pa 1976) 2016;41:371-7. [Crossref] [PubMed]
- Siasios I, Winograd E, Khan A, et al. Cervical sagittal balance parameters after single-level anterior cervical discectomy and fusion: correlations with clinical and functional outcomes. J Craniovertebr Junction Spine 2018;9:56-62. [PubMed]
- Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 2011;68:1309-16; discussion 1316. [Crossref] [PubMed]
- Katsuura Y, Lemons A, Lorenz E, et al. Radiographic analysis of cervical and spinal alignment in multilevel ACDF with lordotic interbody device. Int J Spine Surg 2017;11:13. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012;71:662-9. [Crossref] [PubMed]
- Liang G, Liang C, Zheng X, et al. Sagittal alignment outcomes in lordotic cervical spine: does three-level anterior cervical discectomy and fusion outperform laminoplasty? Spine (Phila Pa 1976) 2019;44:E882-8. [Crossref] [PubMed]
- Passias PG, Bortz C, Horn S, et al. Drivers of cervical deformity have a strong influence on achieving optimal radiographic and clinical outcomes at 1 year after cervical deformity surgery. World Neurosurg 2018;112:e61-8. [Crossref] [PubMed]


