
Posterior osteotomy techniques for rigid cervical deformity correction
Introduction
Posterior-based cervical osteotomies are powerful techniques for the correction of rigid cervical deformity. The major types include Smith-Peterson osteotomy (SPO) and pedicle subtraction osteotomy (PSO). The SPO was originally described for restoration of lumbar lordosis and involves resection of the posterior elements including spinous process, lamina, ligamentum flavum, and bilateral facet joints including bilateral foraminotomies to skeletonize the exiting nerve roots (1). Meticulous central and foraminal decompression are essential to prevent compression of neural elements during closure of the osteotomy site. The original SPO technique was first applied to the cervical spine as an “opening wedge” osteotomy (OWO) at C7 (2). This differs from an SPO in that an osteoclastic fracture is creating during osteotomy closure to lengthen the anterior spinal column. Early variations of this technique were used to treat cervical kyphosis in patients with ankylosing spondylitis and performed in the sitting position with halo traction and local anesthesia (3,4).
The cervical PSO is a more recent technique that involves removal of similar posterior elements as an SPO as well as the pedicles, wedge of vertebral body, and posterolateral vertebral walls. This allows for a more angular correction and improved fusion due to the lack of a gap in the anterior column seen in an OWO, thus the PSO is often referred to as a “closing wedge” osteotomy (CWO). Early reports utilized PSO at C7, however it can also be performed in the upper thoracic spine to avoid compression of the C8 nerve root (5-8). Ames et al. proposed a standardized nomenclature for cervical spine soft-tissue release and osteotomy for spinal deformity correction (Figure 1) (9). Among the seven Ames osteotomy grades, only grade 1 (partial facet joint resection), grade 2 (complete facet joint/Ponte osteotomy), grade 5 (OWO), and 6 (CWO) are typically considered posterior osteotomies. This article will summarize posterior osteotomy techniques for rigid cervical deformity.

Preoperative evaluation
The preoperative evaluation begins with a detailed history and physical exam with special care to identify any neurologic deficits and signs of myelopathy. Preoperative imaging should include anteroposterior (AP)/lateral and dynamic cervical X-rays, scoliosis films, computed tomography (CT), and magnetic resonance imaging (MRI) of the cervical spine. Special attention must be given to the vertebral artery to identify aberrant anatomy with a low threshold to obtain formal vascular imaging in the form of a CT angiogram (CTA) or magnetic resonance angiogram (MRA). Each imaging modality provides unique information that guides the surgical plan. Cervical X-rays can assess the severity of deformity, flexibility, apex location, and sites of foraminal stenosis. Scoliosis films provide information on global balance and may reveal underlying thoracolumbar deformities that may be contributing to a given patient’s cervical deformity. Important radiographic parameters include cervical lordosis, C2–C7 sagittal vertical axis, T1 slope, and chin-brow vertical angle (10). CT allows careful evaluation of the vertebral body, disc spaces, and facet joints to assess for fusion. Compression of the spinal cord and nerve roots should be noted with decompressions incorporated into the surgical plan as needed.
Surgical techniques
Positioning
The surgery and anesthesia teams should evaluate the patient’s airway, degree of spinal cord compression, and potential instability to determine the safest approach for endotracheal intubation, which in complex cases may require awake fiber intubation. Cervical deformity cases utilizing an osteotomy should be performed with intraoperative neuromonitoring and appropriate vascular access. In cases with spinal cord compression or instability, baseline should be obtained prior to manipulating the head and neck for final positioning. In patients with spinal cord compression, the mean arterial pressure (MAP) should be maintained above 80 mmHg during intubation and throughout the operation. Patients are positioned prone on an open Jackson table with the head secured in a Mayfield head frame, halo ring, or dual-vector traction system with Gardner-Wells tongs. The table should be positioning in reverse Trendelenburg to minimize blood loss by reducing venous pressures and offset the patient’s cervicothoracic kyphosis so that the operative field is relatively horizontal.
Exposure and instrumentation
The spine is exposed using standard techniques in a subperiosteal fashion. Exposure should be carried out laterally to visualize the lateral masses of the cervical spine and transverse processes of the thoracic spine to ensure accurate placement of lateral mass screws and pedicle screws, respectively. In general, the occipitoatlantal and atlantoaxial joins should be preserved since they account for over 50% of the range of motion in the cervical spine. However, if the spine is completely ankylosed as in ankylosing spondylitis, instrumentation should extend to the occiput to maximize the strength of bony fixation. In general, the surgical plan should include fixation 3–4 levels above the osteotomy site. Therefore, for the tradition C7 OWO, lateral mass screws are placed bilaterally from C3–C5, pedicle screws from T2–T4, and either pedicle, pars, or translaminar screws at C2. Screws can be placed at either C6 or T1 depending on whether fixation is needed proximal or distal to the osteotomy. If a T1 pedicle screw is placed then the C6 lateral mass screw can be left out, or vice versa. There is rarely enough room to include both C6 and T1 screws. Screws should be placed in a straight line to minimize the need for additional rod contouring. Accessory rods can be secured across the osteotomy site to provide increased strength and minimize the risk of rod fracture.
Partial facet joint resection
Grade 1 cervical osteotomy includes facet capsule resection or partial facet resection. Although this osteotomy provides limited lordosis, it can be applied over multiple levels to provide a cumulative effect. Removal of the facet and associated cartilage also provides a bony surface for fusion. An important prerequisite for effective grade 1 osteotomies is mobility of the anterior column. In practicality grade 1 osteotomies are rarely used in isolation but rather to supplement higher grade osteotomies.
Complete facet joint resection
Grade 2 cervical osteotomy involves complete facet resection at a specific level, as well as soft-tissue and bony elements including spinous process, lamina, and ligamentum flavum. Like grade 1 osteotomies, grade 2 osteotomies require mobility of the anterior column and can be performed across multiple segments for a cumulative correction. Historically, grade 2 osteotomies were referred to as SPOs when performed across fused facets or Chevron and extension osteotomy in unfused segments (9,11,12). Similarly, the polysegmental and Ponte osteotomies are also classified as grade 2 (13,14).
OWO
The traditional OWO is performed at C7 and starts with a complete laminectomy with partial laminectomies of C6 and T1 to prevent compression of the spinal cord after osteotomy closure. We recommend leaving the spinous processes of C6 and T1 intact if possible. The C7–T1 facet joints (inferior articular process of C7 and superior articular process of T1) are removed using a combination of Leksell rongeur and high-speed burr. It is important to ensure complete removal of the T1 superior articular process so that the exposure is flush down to the T1 pedicles. The C7 pedicle is completely removed down to the vertebral body using a high-speed burr and Leksell. Both of these maneuvers ensure complete visualization of the C8 nerve root and prevent compression during osteotomy closure. This osteotomy utilizes a fulcrum of rotation in the middle column with shortening of the posterior column and lengthening of the anterior column.
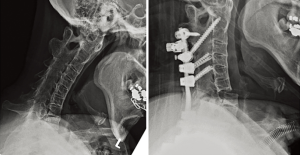
The rod is bent into the desired contour and secured to the thoracic pedicle screws. A member of the surgical team then uses the Mayfield clamp, halo ring, or Gardner-Wells tongs to slowly and carefully extend the neck into the desired position. Following this extension maneuver and osteoclastic fracture, the C7 and C8 nerve roots must be carefully inspected to ensure there is no new impingement. Neuromonitoring can provide valuable information during this critical step but there is no substitute for direct visualization of the nerve roots with additional bony removal as needed. A temporary rod can also be used across the osteotomy site to prevent subluxation or premature osteotomy closure. As the head is extended to the final desired orientation, the rod should be secured to the cervical screws above the osteotomy site. In some cases, a hinged rod can be used across the osteotomy site to facilitate closure and fixation. Once the head is in final position, neuromonitoring signals are checked to confirm stability. Fluoroscopy is used to assess the correction and overall alignment. Attention is then turned to arthrodesis using a combination of local autograft. The spinous process of C7 can be split in the sagittal plane and placed between the decorticated C6 and T1 spinous process and secured with a cable. The gap between the C6 and T1 lateral masses can be filled with autograft from upper thoracic spinous processes. Preoperative and postoperative X-rays for an OWO are shown in Figure 2.
CWO
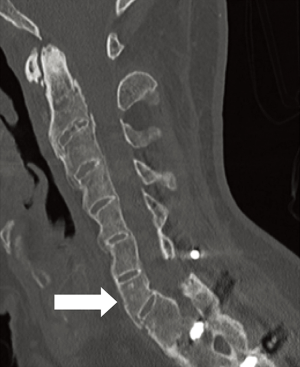
The CWO is similar to the OWO with additional removal of a wedge of bone in the vertebral body using either a high-speed drill or osteotomes. This osteotomy is typically performed at C7 or T1 below the level of the vertebral artery, but can also be performed at T2 or T3. Performing the osteotomy at any of the thoracic levels involves additional dissection and removal of the associated rib heads to complete the osteotomy, which increases the difficulty and complexity of the case. The OWO involves lengthening the anterior column, which has been associated with vascular, neurologic, tracheal, and esophageal complications and thus the CWO is theoretically safer in this respect. Like the OWO, the C8 nerve roots must be widely decompressed prior to closure of the osteotomy. The CWO utilizes a fulcrum of rotation in the middle column with shortening of the posterior column to provide additional lordosis. Preoperative and postoperative X-rays for a CWO are shown in Figure 3.
Postoperative management
After cervical deformity correction patients are observed in the intensive care unit overnight with hourly neurologic exams. For long-segment fusions, labs should be checked at least every 6 hours with aggressive transfusion protocols for cases with significant blood loss. Our typical practice is to maintain the MAP above 80 mmHg overnight to avoid episodes of hypotension overnight. We also maintain patients in a rigid cervical collar for at least 6 weeks. Patients with OWO or CWO may be kept intubated overnight if there is concern for airway edema. Furthermore, patients with significant correction after OWO may require formal speech evaluation before advancing their diet.
Limitations
Posterior osteotomies are powerful tools for the correction of rigid cervical deformity. There are important limitations to these techniques. During the OWO, translation can occur during osteoclasis which makes it inherently less stable than a CWO. Biomechanical studies have confirmed that the CWO provides increased stiffness across the osteotomy site compared to OWO (15). One strategy is to perform an additional anterior cervical interbody fusion to minimize the risk of pseudarthrosis, however this may not be necessary in all patients, particularly those with ankylosing spondylitis who often fuse well with posterior-only constructs. However, anterior column support may minimize the risk of rod fracture prior to bony fusion. It is also important to recognize that in patients with both cervical and thoracic kyphosis, additional osteotomies in the thoracolumbar spine may be needed to achieve the appropriate deformity correction.
Conclusions
Posterior cervical osteotomies should be a component of every deformity surgeon’s armamentarium for the treatment of rigid cervical kyphosis. These include low-grade osteotomies such as partial or complete facetectomies and higher-grade OWOs and CWOs. For high-grade osteotomies special care must be taken to ensure adequate decompression of the adjacent cervical nerve roots, particularly C8, so that there is no impingement during osteotomy closure. OWOs lengthen the anterior column and carry a slightly higher risk of vascular, neurologic, tracheal, and esophageal complications. Appropriate patient selection, meticulous technique, and careful perioperative care are essential for successful patient outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. LAT serves as the unpaid editorial board member of Journal of Spine Surgery from Jan. 2019 to Jan. 2021. LAT served as the unpaid Guest Editor of the series. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res 1969.6-9. [PubMed]
- Urist MR. Osteotomy of the cervical spine; report of a case of ankylosing rheumatoid spondylitis. J Bone Joint Surg Am 1958;40-A:833-43. [Crossref] [PubMed]
- Simmons ED, DiStefano RJ, Zheng Y, et al. Thirty-six years experience of cervical extension osteotomy in ankylosing spondylitis: techniques and outcomes. Spine (Phila Pa 1976) 2006;31:3006-12. [Crossref] [PubMed]
- Simmons EH. The surgical correction of flexion deformity of the cervical spine in ankylosing spondylitis. Clin Orthop Relat Res 1972.132-43. [Crossref] [PubMed]
- Deviren V, Scheer JK, Ames CP. Technique of cervicothoracic junction pedicle subtraction osteotomy for cervical sagittal imbalance: report of 11 cases. J Neurosurg Spine 2011;15:174-81. [Crossref] [PubMed]
- Khan SN, Braaksma B, An HS. Cervical pedicle subtraction osteotomy for fixed flexion deformities. Orthopedics 2012;35:484-9. [Crossref] [PubMed]
- Tokala DP, Lam KS, Freeman BJ, et al. C7 decancellisation closing wedge osteotomy for the correction of fixed cervico-thoracic kyphosis. Eur Spine J 2007;16:1471-8. [Crossref] [PubMed]
- Wollowick AL, Kelly MP, Riew KD. Pedicle subtraction osteotomy in the cervical spine. Spine (Phila Pa 1976) 2012;37:E342-8. [Crossref] [PubMed]
- Ames CP, Smith JS, Scheer JK, et al. A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: clinical article. J Neurosurg Spine 2013;19:269-78. [Crossref] [PubMed]
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59. [Crossref] [PubMed]
- Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31:S171-8. [Crossref] [PubMed]
- Lu DC, Chou D. Flatback syndrome. Neurosurg Clin N Am 2007;18:289-94. [Crossref] [PubMed]
- Sansur CA, Fu KM, Oskouian RJ Jr, et al. Surgical management of global sagittal deformity in ankylosing spondylitis. Neurosurg Focus 2008;24:E8. [Crossref] [PubMed]
- Geck MJ, Macagno A, Ponte A, et al. The Ponte procedure: posterior only treatment of Scheuermann's kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech 2007;20:586-93. [Crossref] [PubMed]
- Scheer JK, Tang JA, Buckley JM, et al. Biomechanical analysis of osteotomy type and rod diameter for treatment of cervicothoracic kyphosis. Spine (Phila Pa 1976) 2011;36:E519-23. [Crossref] [PubMed]


