
Return to play in professional baseball players following transforaminal endoscopic decompressive spine surgery under local anesthesia
Introduction
Endoscopic lumbar spine surgery has gained traction for the treatment of common lumbar spine disorders (1-4). Yeung popularized the single portal transforaminal endoscopic approach in 1992, then trademarked and published the technique known as YESS™ in 1998 (5-8). The skin incision is limited to 8 mm, and the surgery can be done under the light sedation and local anesthesia (9). Endoscopic surgery is considered the least invasive spine surgery due its minimally invasive approach that requires very minimal muscle dissection by dilation required to access the neuroforamen. Most surgery is performed under general anesthesia, but the transforaminal approach performed routinely under local anesthesia provides extra clinical surgical information of value to the operating surgeon.
Birkenmaier et al. (10) reviewed PUBMED listed publications on endoscopic discectomy including articles regarding full-endoscopic discectomy popularized by Ruetten et al. (11) corroborating the common knowledge of faster postoperative rehabilitation, shorter hospital stay, faster return to work compared to translaminar microsurgical techniques. Fujii et al. (12) recently reviewed 6 cases of physician that underwent the full-endoscopic spine surgery. One physician was able to return to their clinical duties within just two days postoperatively with a mean sick leave of 5.8 days after the surgery. The authors asserted that the endoscopic spine surgery under the local anesthesia was a valid alternative to open spine surgery, allowing for a quick return to their original preoperative activity. With the interlaminar approach, however, Ruetten et al. prefers using general anesthesia because retracting the traversing nerve is painful except at L5–S1 where retraction is not needed (11).
Regarding professional athletes, the ideal surgical intervention would be full-endoscopic surgery, since the damage of the back muscle is the minimum, using tubular retractors. Manabe et al. (13) and Sairyo et al. (14) reported the effectiveness of the endoscopic thermal pulsed radiofrequency annuloplasty in the professional athletes playing at the highest level using the YESS™ technique. However, limited information on how to treat these athletes with endoscopic surgery, regardless of anesthesia type, is available in the literature.
We have surgically treated five professional baseball players in these days. They underwent transforaminal endoscopic discectomy (5-8), thermal annuloplasty (13-15) and foraminoplasty (16-19) as previously described in the literature. They were able to return to the professional level play within three months after “full”-transforaminal endoscopic surgery. In this case report, we review the preoperative diagnostic work, surgical management, and outcomes in five professional baseball players.
Case presentation
Five professional baseball players were surgically treated with transforaminal endoscopic decompression. The transforaminal full-endoscopic surgery was conducted just after the season in three cases, and just before the season, in 2 cases (Table 1). The preoperative diagnosis was discogenic pain in 3 players, herniated nucleus pulposus (HNP) in 1, and foraminal stenosis in another player, respectively.
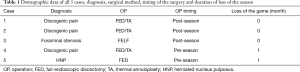
Full table
Transforaminal endoscopic surgery was conducted under local anesthesia and light sedation through an 8 mm skin incision. All endoscopic surgeries were performed under the local anesthesia. Surgical treatment included discectomy, thermal annuloplasty, and foraminoplasty (Table 1). The surgical procedure of the transforaminal selective endoscopic discectomy (SED™) with and without foraminoplasty has been described and trademarked by Yeung (5-8). The estimated blood loss was minimal in all five players. In the series, we did not encounter the surgery-related complications such as nerve root injury, hematoma, dural tear, surgical site infection, or others. The timing of post-operative rehabilitation, excessive training, a complete return to the professional level and duration of the missed season was recorded.
Since the transforaminal full-endoscopic surgery was successfully conducted, the rehabilitation schedule after the surgery was executed with the guidance of the athletic trainer in their team. Within four weeks, moderate exercise was allowed for the lumbar spine: i.e., isometric trunk stabilization. Furthermore, for the other adjacent joints such as thoracic spine and hip joint, mobilization exercise was performed. Between 4 to 6 weeks, more extreme training was allowed with stable lumbar spine condition (avoiding flexion and twisting motion). After six weeks, restrictions were lifted for returning to professional activity. With this customized rehabilitation program, all five players could perform original activity eight weeks after the surgery, and at about 12 months, they were able to play at an unrestricted competitive professional level.
Cases 1, 2, and 3 underwent surgery just after the season ended in November. Thus, they started their professional activities in the pre-season camping in February. These three players did not lose any days of playtime in the following season. The remaining two players (case 4 and case 5) underwent surgery about two months before the season started in February. Therefore, these two players missed about one month of the season. Clinical follow-up available at the time of the writing of this case report ranged from 6 to 20 months postoperatively. All five players were playing at a highly competitive professional level.
Case 1
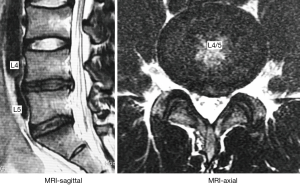
This case was a male player, and his position was an outfielder. He had been suffering from low back pain for two years. Thus, he, with the support of his team, decided to have surgery during the off-season. He was referred to us for minimally invasive full-endoscopic surgery. His symptom was only low back pain during lumbar flexion. Neurologically, there were no abnormalities, including motor, sensory, and reflexes.
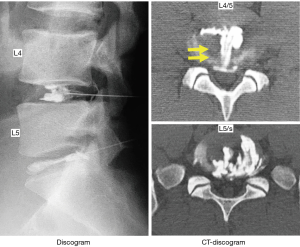
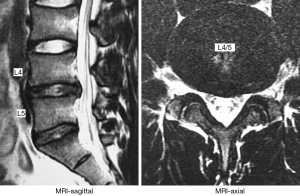
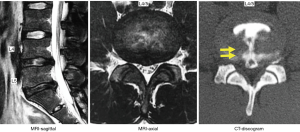
Figure 1 demonstrates MRIs taken before the surgery with slight degeneration of the L4/5 and L5/S1 disc with contained herniation and bulging of both discs. The patient underwent discography to aid in the diagnostic workup and to identify the pain generator (Figure 2). The patient reported strong concordant pain at L4/5 and moderate pain at L5/S1. The painful toxic annular tear was visible at L4/5 (yellow arrows in Figure 2, right panel). The L4/5 annular tear was deemed the main pain generator. A transforaminal endoscopic discectomy and thermal annuloplasty with pulsed radiofrequency was performed (13-15). After surgery, his low back pain completely vanished, and during the next season, he was able to play through all the games and recorded the highest-score play of his professional career. Figure 3 shows the player’s postoperative MRI scan one year after the index surgery. Although disc degeneration at L4/5 and L5/S1 persisted, disc bulging at L4/5 was reduced.
Case 2
This case was a male outfielder. He had been suffering from low back pain and decided to have surgery at the end of the season—Figure 4 demonstrates MRI and CT discogram before the surgery. The disc at L4/5 and L5/S1 show slight disc degeneration. Disc bulging was noted at L4/5. Discography and CT-discogram with a toxic annular tear is shown on the right panel of Figure 4. We performed transforaminal endoscopic discectomy and thermal annuloplasty for his discogenic pain. From the beginning of the following season, he actively showed the professional performance without low back pain.
Case 3
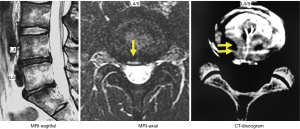
This case was a male infielder and very similar case as cases 1 and 2. He had been suffering from multiple episodes of the sudden onset of low back pain. Two months before the season, he had another sudden onset of low back pain, and decided to have surgery. Figure 5 demonstrates MRI and CT discogram before the surgery. The disc at L4/5 and L5/S1 show moderate disc degeneration with disc collapse. High signal intensity zone was noted at L4/5 as demonstrated by a single yellow arrow in the middle panel of Figure 5. A discography and CT-discogram revealed a painful toxic annular tear at L4/5 as demonstrated by the yellow arrows in the right panel of Figure 5. We performed transforaminal full-endoscopic discectomy and thermal annuloplasty for his discogenic pain. After the surgery, his low back pain disappeared. Two months after the surgery, the following season was started. About 2.5 months after the surgery, he returned to the 2nd professional league, and finally about three months after the surgery he attended the game in the 1st league. Thus, he just lost one month of the ongoing season.
Discussion
In this case report, we reviewed five professional baseball players who underwent transforaminal endoscopic lumbar surgery under the local anesthesia. In all five professional baseball players, the endoscopic surgery was successfully performed, and all of them returned to the game within three months postoperatively. Our case report indicates that transforaminal endoscopic lumbar surgery with thermal annuloplasty is suitable to treat professional athletes with minimal disruption of play and rapid postoperative recovery.
Initially, the transforaminal endoscopic surgery was indicated for herniated disc (5-8). The advancement of endoscopic surgical instruments, including surgical drills led to expanded indications for foraminoplasty. Annular tears and discogenic pain became treatable with the endoscopic platform by performing thermal annuloplasty with the use of pulsed bipolar radiofrequency specially adapted for spinal endoscopes (13-15). For foraminal stenosis, transforaminal lumbar foraminoplasty was established (16-20). Recently, it became due to the development of endoscopic burrs it became routinely possible to treat lateral recess stenosis endoscopically under direct vision with the transforaminal technique (8,16,18-20).
Ruetten et al. reviewed the return to original activity levels postoperatively for the endoscopic surgery and microsurgery (11). Patients returned twice quickly to work job with the endoscopic surgery when compared to microdiscectomy. Mahesha reviewed the first 100 cases of endoscopic lumbar discectomy and reported that patients could return to work as early as two days after an uneventful endoscopic surgery (21). Their report suggested that endoscopic surgery affords patients a quick return to their original life and professional activities. However, whether this applies to professional athletes is hitherto unknown, and the peer-reviewed literature is sparse on this subject.
In the literature, there is some information on the return to play (RTP) after the traditional discectomy. Watkins et al. (22) in 2003 reported the outcome of the surgical treatment of the HNP for 60 elite athletes, including professional and Olympic athletes. All of them underwent microscopic discectomy, and the average duration for RTP after the surgery was 5.2 months. It ranged from 1 to 15 months. Among the 60 athletes, seven could not return to the original competitive level. In 2012, Watkins et al. published a follow-up study on their 171 cases of professional athletes (23). Among them, 85 underwent microscopic discectomy for HNP. The average time for RTP was 5.8 months. About half of them returned within 3 months, and 72% within 6 months.
Earhart et al. reviewed 69 baseball players having HNP (24). Among them, 40 were surgically treated, and they needed 8.7 months to RTP after diagnosis. Roberts et al. surgically treated 20 major league pitchers with lumbar disc herniation and reported that they needed 7.3 months after diagnosis to RTP (25). These two papers reported the RTP after the diagnosis and not after the surgery. Thus, the RTP data reported by Earhart et al. and Roberts et al. may include the duration of the conservative treatment before the surgery.
In this case series of five professional baseball players, we demonstrate the effectiveness of the transforaminal endoscopic lumbar spine surgery under the local anesthesia. The endoscopic surgery was capable of eliminating the players’ pain generator successfully without any complications. All players started full-activity within two months after the surgery, and three months after the surgery, they showed RTP at the professional level. Three of them underwent surgery just after the season ended (around November), they could play without restrictions during the following season. The two remaining players underwent surgery two months before the start of the season (around February). Thus, they lost about only one month of active playtime during the following season.
Our group has previously reported on the efficacy of the transforaminal endoscopic lumbar discectomy and thermal annuloplasty under local anesthesia (14). That series included 12 athletes who underwent endoscopic thermal annuloplasty. Of these 12 athletes, two required additional surgery, and the duration of RTP for the remaining 10 was 2.8 months.
Conclusions
These case reports corroborate our previously published observations (12,14) with the transforaminal endoscopic lumbar surgery in professional athletes. As the least invasive spine surgery available today, transforaminal endoscopic decompression is suitable for high-class athletes for early and unimpeded RTP.
Acknowledgments
Koichi Sairyo, senior author studied transforaminal endoscopic under Dr. Anthony Yeung, using his Trademarked YESS™ technique
Footnote
Conflicts of Interest: The senior author, Professor Koichi Sairyo, has a donated fund laboratory for Senko Medical, and Nipro Inc. However, his affiliation with these companies does not conflict with the content of this manuscript. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Oral consent was obtained from the patients for publication of this manuscript and any accompanying images.
References
- Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years' experience. Clin Orthop Relat Res 1989.9-23. [Crossref] [PubMed]
- Kambin P, Schaffer JL. Percutaneous lumbar discectomy. Review of 100 patients and current practice. Clin Orthop Relat Res 1989.24-34. [Crossref] [PubMed]
- Kambin P. Arthroscopic microdiskectomy. Mt Sinai J Med 1991;58:159-64. [PubMed]
- Schreiber A, Leu H. Percutaneous nucleotomy: technique with discoscopy. Orthopedics 1991;14:439-44. [PubMed]
- Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. Mt Sinai J Med 2000;67:327-32. [PubMed]
- Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine 2002;27:722-31. [Crossref] [PubMed]
- Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am 2007;38:363-72. [Crossref] [PubMed]
- Yeung AT. The Yeung Percutaneous Endoscopic Lumbar Decompressive Technique (YESSTM). J Spine 2018;7:408. [Crossref]
- Sairyo K, Chikawa T, Nagamachi A. State-of-the-art transforaminal percutaneous endoscopic lumbar surgery under local anesthesia: Discectomy, foraminoplasty, and ventral facetectomy. J Orthop Sci 2018;23:229-36. [Crossref] [PubMed]
- Birkenmaier C, Komp M, Leu HF, et al. The current state of endoscopic disc surgery: review of controlled studies comparing full-endoscopic procedures for disc herniations to standard procedures. Pain Physician 2013;16:335-44. [PubMed]
- Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931-9. [Crossref] [PubMed]
- Fujii Y, Yamashita K, Sugiura K, et al. Early return to activity after minimally invasive full endoscopic decompression surgery in medical doctors. J Spine Surg 2020;6:S294-S299.
- Manabe H, Yamashita K, Tezuka F, et al. Thermal Annuloplasty Using Percutaneous Endoscopic Discectomy for Elite Athletes with Discogenic Low Back Pain. Neurol Med Chir (Tokyo) 2019;59:48-53. [Crossref] [PubMed]
- Sairyo K, Kitagawa Y, Dezawa A. Percutaneous endoscopic discectomy and thermal annuloplasty for professional athletes. Asian J Endosc Surg 2013;6:292-7. [Crossref] [PubMed]
- Tsou PM, Alan Yeung C, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J 2004;4:564-73. [Crossref] [PubMed]
- Lewandrowski KU. Endoscopic Transforaminal and Lateral Recess Decompression After Previous Spinal Surgery. Int J Spine Surg 2018;12:98-111. [Crossref] [PubMed]
- Lewandrowski KU. Incidence, Management, and Cost of Complications After Transforaminal Endoscopic Decompression Surgery for Lumbar Foraminal and Lateral Recess Stenosis: A Value Proposition for Outpatient Ambulatory Surgery. Int J Spine Surg 2019;13:53-67. [Crossref] [PubMed]
- Yeung A, Roberts A, Zhu L, et al. Treatment of Soft Tissue and Bony Spinal Stenosis by a Visualized Endoscopic Transforaminal Technique Under Local Anesthesia Neurospine 2019;16:52-62. [PubMed]
- Yamashita K, Higashino K, Sakai T, et al. Percutaneous full endoscopic lumbar foraminoplasty for adjacent level foraminal stenosis following vertebral intersegmental fusion in an awake and aware patient under local anesthesia: A case report. J Med Invest 2017;64:291-5. [Crossref] [PubMed]
- Sairyo K, Higashino K, Yamashita K, et al. A new concept of transforaminal ventral facetectomy including simultaneous decompression of foraminal and lateral recess stenosis: Technical considerations in a fresh cadaver model and a literature review. J Med Invest 2017;64:1-6. [Crossref] [PubMed]
- Mahesha K. Percutaneous endoscopic lumbar discectomy: Results of first 100 cases. Indian J Orthop 2017;51:36-42. [Crossref] [PubMed]
- Watkins RG 4th, Williams LA, Watkins RG 3rd. Microscopic lumbar discectomy results for 60 cases in professional and Olympic athletes. Spine J 2003;3:100-5. [Crossref] [PubMed]
- Watkins RG 4th, Hanna R, Chang D, et al. Return-to-play outcomes after microscopic lumbar diskectomy in professional athletes. Am J Sports Med 2012;40:2530-5. [Crossref] [PubMed]
- Earhart JS, Roberts D, Roc G, et al. Effects of lumbar disk herniation on the careers of professional baseball players. Orthopedics 2012;35:43-9. [Crossref] [PubMed]
- Roberts DW, Roc GJ, Hsu WK. Outcomes of cervical and lumbar disk herniations in Major League Baseball pitchers. Orthopedics 2011;34:602-9. [Crossref] [PubMed]


