
Posterior cervical foraminotomy for cervical radiculopathy: should cervical alignment be considered?
Introduction
Since its initial description by Scoville and Frykholm, posterior cervical foraminotomy (PCF) has been used extensively for managing cervical radiculopathy (1,2). Despite an increasing trend for anterior approach, microsurgical and endoscopic advances have enabled excellent outcomes in up to 93–96% of patients by minimally invasive PCF, with motion preservation (3). Eccentrically located disc fragments are more accessible by PCF, as opposed to anterior entry, without risking postoperative dysphagia and hoarseness from esophageal and laryngeal nerve retraction. PCF is also effective for neuroforaminal stenosis due to bony structures, allowing direct decompression of affected cervical roots. On the other hand, the posterior approach inherently compromises posterior cervical column integrity, where roughly two-thirds of cervical load is transmitted (4). Hence, surgeons often avoid PCF in patients presenting with imaging evidence of kyphosis or straightening to prevent postoperative kyphotic deformity (5-7).
In this retrospective study, we reviewed interval change in cervical segmental angles after PCF, analyzing factors affecting cervical sagittal re-alignment in the immediate postoperative period and 6 months follow-up.
Methods
Study design
Retrospective case series.
Patient population
Institutional Review Board of our Hospital approved this retrospective study. Between January, 2007 and January, 2013, a total of 286 consecutive patients underwent key-hole PCF at our hospital for unilateral radiculopathy due to degenerative cervical disease (males, 197; females, 89; mean age, 51.2 years, range: 20–78 years). Patients with myelopathy, neoplasm, congenital deformity, fracture, or history of previous cervical spinal surgery were excluded, as were patients with focal instability at affected levels. Focal instability on dynamic radiograph was defined as a translation more than 3.5 mm and an angulation exceeding 11° in sagittal plane (8). Pathology predisposing to radiculopathy was softened disc (n=158), foraminal stenosis (n=112), or both (n=16). Table 1 shows patient demographic and levels required surgical intervention are summarized in Table 2. Among patients underwent two level surgery, no crossed-directional posterior foraminotomy was performed.
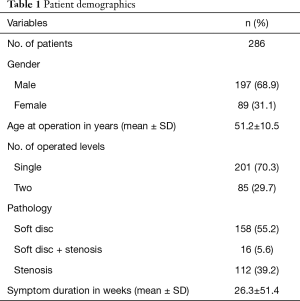
Full table
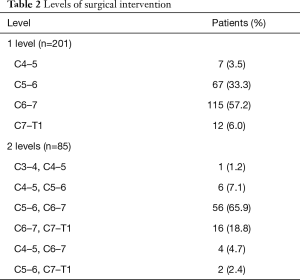
Full table
Surgical procedure
A standard key-hole PCF, as previously described, was performed in all instances (9). All patients underwent surgery in the prone position under general anesthesia. After the correct level was confirmed based on the lateral radiograph, a vertical skin incision below 3 cm on each level was made and routine muscular dissection performed to expose the lamina and facet to be operated. Retraction was performed using a self-retractor system (Papavero-Caspar speculum, B Braun, Germany), and the field was prepared. After a second confirmation of the target level, laminotomy and foraminotomy with partial (<50%) facetectomy were performed at that level under the operating microscope using high-speed drills. The mediolateral course of the nerve root was exposed. Extruded or ruptured disc material was removed using pituitary forceps with gentle retraction of the nerve root. In cases with foraminal stenosis, additional bony decompression of the proximal root or decompression of the facet was performed carefully, and the exiting root was freed with judicious drilling of the pedicle using a 3-mm diamond burr, small rongeurs, and dissectors.
Outcome measurements
On admission, prior to postoperative radiographs and 6 months after operation follow-up in outpatient, patients were routinely asked by doctor in charge to gauge levels of pain they feeling at that point in time by visual analogue scale (VAS) and it was recorded in medical chart.
Radiographic studies
The day before operation, patients were admitted and preoperative plain radiographs, including dynamic views, in standing and neutral positions were checked. Within 2 days and 6 months after surgery, each patient was subjected to lateral plain radiograph in same methods without neck collar. Radiographs were assessed for sagittal alignment by the method outlined by Katsumi and colleagues (7). To evaluate change in overall cervical sagittal alignment, two spinal neurosurgeons separately measured Cobb’s angle between C2 and C7, which defined as the angle formed by lines drawn at the base of axis and the superior endplate of the C7 vertebral body on lateral radiograph. Measurements were quantified using a picture archiving communication system (PACS) feature (PiViewSTAR, INFINITT Healthcare Co, Seoul, Korea). All angles were measured three times by each surgeon, and a mean angle was determined to accommodate investigator error in assessing margins of vertebral bodies. For each measurement, kyphotic alignment was indicated by a negative value and lordotic alignment by a positive value. Three categories were used to classify spinal alignment: kyphosis, straightening, and lordosis. Kyphotic or lordotic angulation <4° was defined as straight alignment.
Statistical analysis
Multiple regression analysis was used to evaluate the factors influencing interval change of sagittal alignment after PCF and relationship between VAS score and Cobb’s angle was examined with correlation analysis using Spearman’s rho correlation coefficient. Statistical analysis relied on standard software (SPSS v16.0 for Windows, SPSS, Inc., Chicago, IL, USA) was performed and statistical significance was set at P<0.05.
Results
Perioperative sagittal alignment changes
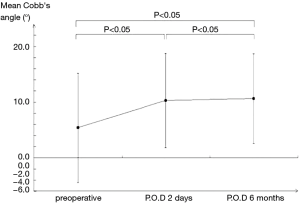
On preoperative plain radiographs, 46 patients (16.1%) displayed kyphosis and 81 patients (28.3%) showed straightening. In 2 days after PCF, 96 (75.6%) of 127 patients with loss of normal lordotic curvature preoperatively showed improvement in sagittal alignment, and 30 patients (23.6%) did not. Only five patients shifted to worse categories: one from straight to kyphotic alignment, and four from lordotic to straight alignment. On follow-up plain radiographs after 6 months, the improvement of sagittal alignment was well maintained, but rather more prominent: 7 patients shifted to better categories and no patient shifted to worse. Repeated-measured ANOVA was used to compare the Cobb’s angles at each point of time, and paired t-test with Bonferroni’s method was used for adjustment of multiple comparison. The mean Cobb’s angle on preoperative, 2 days after operative, and 6 months’ follow-up was 5.4±9.8°, 11.2±7.9°, and 11.5±7.5°. Angular improvements with PCF were statistically significant between them (P<0.05, Figure 1). Interval changes in cervical sagittal alignment with PCF after 2 days and 6 months are summarized in Tables 3 and 4.
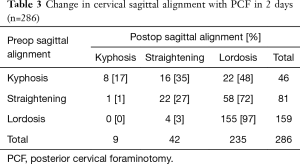
Full table
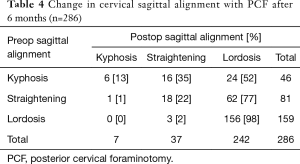
Full table
Factors related to interval change of sagittal alignment
In the present study, factors influencing interval change of sagittal alignment were not interrelated (1.077≤ variance inflation factor ≤1.287). Improvement in sagittal alignment was primarily seen when radiculopathy was due to softened discs, rather than stenosis (P<0.05, β=3.279), and with shorter symptom duration (P<0.05, β=−0.042). Patient age had no significant impact on outcomes (P=0.614) and count of affected levels (single or two) also did not (P=0.366).
VAS score and sagittal alignment
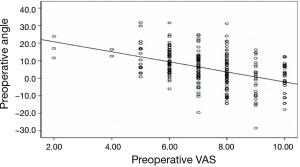
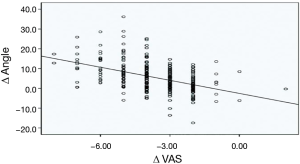
In patients with higher preoperative VAS score, Cobb’s angle was significantly lower (P<0.05, r=−0.460) (Figure 2). As perioperative VAS score declined, sagittal alignment improved significantly (P<0.05, r=−0.508) (Figure 3).
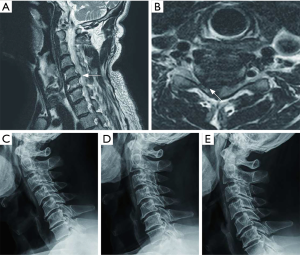
Case illustrations of definite interval change in sagittal alignment
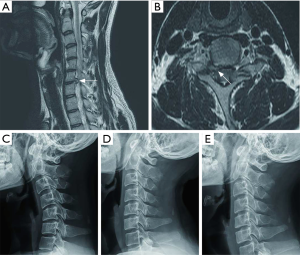
Patient 1
A 62-year-old male presented with severe neck and right arm pain of 3 months’ duration. On magnetic resonance imaging (MRI), a large, soft herniated disc was apparent to the right of C5–6, compressing the right C6 nerve root (Figure 4A,B), and straight sagittal alignment on plain films was estimated at −0.42° (Figure 4C). Right-sided PCF at C5–6 resulted in significant pain reduction (VAS 8→3). A plain radiograph (postsurgical day 2) showed reversal of sagittal alignment to lordotic curvature, estimated at +10.98° (Figure 4D). On 6 months follow-up, his clinical symptom was favorable (VAS 2) and cervical sagittal alignment was maintained, estimated at +13.24° (Figure 4E).
Patient 2
A 30-year-old male presented with severe right arm pain of 5 months’ duration. On MRI, a soft foraminal disc herniation was evident to the right of C6–7, compressing the right C7 nerve root (Figure 5A,B) and straight sagittal alignment estimated at −27.5° by plain radiograph (Figure 5C). Right-sided PCF at C6–7 resulted in significant pain reduction (VAS 8→2). A plain radiograph (postsurgical day 2) showed reversal of sagittal alignment to lordotic curvature, estimated +13.7° (Figure 5D). On 6 months follow-up, his clinical symptom was favorable (VAS 1) and cervical sagittal alignment was maintained, estimated at +9.6° (Figure 5E).
Discussion
Similar to the lumbar region, standard treatment of cervical radiculopathy was historically linked to disorders such as degenerative disc disease or neuroforaminal stenosis, where a posterior approach is generally used. However, posterior access has a difficulty for pathology located in medio-ventral to affected nerve roots, so techniques involving anterior access eventually developed. Smith and Robinson were the first to report procedures by anterior means (10), which others then adopted and modified, although recently, interest in treating paracentral and foraminal cervical disease via posterior approach has been renewed (11-13). This resurgence is attributable a series of reports detailing the excellent outcomes achieved through minimally invasive spinal surgery (14,15). With an anterior approach, adjacent segment disease may ensue, and greater depth of dissection is usually required to reach surgical targets (16,17).
Despite the clear advantages of PCF, particularly in patients with cervical radiculopathy, many neurosurgeons are reluctant to utilize a posterior approach if preoperative sagittal alignment is kyphotic or straight. Because the posterior neural arch, composed of articular processes and facets, is largely responsible for load transmission in the cervical spine, any significant compromise of integrity may cause instability (18,19). With loss of normal sagittal lordosis, the weight-bearing axis shifts anteriorly, ultimately leading to kyphosis (20).
A number of publications have implicated preexisting cervical deformity as a risk factor for cervical kyphosis after laminectomy (5-7). Kaptain et al. have indicated that up to 21% of patients may develop kyphosis after total laminectomy, but the risk doubles if preoperative radiologic studies demonstrate a straight spine (6). In key-hole PCF, Jagannathan et al. assessed 5-year outcomes of 162 patients undergoing single-level PCF. Although PCF is less invasive at posterior neural arch, they found that patients with preexisting loss of cervical lordosis, as well as elderly patients (>60 years of age) and those who have had previous posterior surgery, are at higher risk for postoperative kyphosis and thus merit closer follow-up (21). Regardless of these issues, more than two-third of the patients we studied presenting with kyphotic or straight curvature improved short-term following PCF, and it was maintained on follow-up radiographs.
Our study is not without limitation. We assumed that preoperative loss of lordotic curvature was secondary to pain-induced muscular spasm. Indeed, our results indicate that preoperative sagittal alignment and pain (as measured by VAS score) are related; and similarly, as postoperative VAS score declined, sagittal alignment improved significantly. However, this premise is still in debate. Various papers have documented that many factors, in addition to pain, have bearing on sagittal alignment of the cervical spine, including degenerative changes, pelvic tilt, standing position, and head position, all of which should be considered in radiographic evaluations (22-27). Thus, the fundamental process of determining spinal alignment is fraught with difficulty. Then again, the same individuals were compared in a relatively short period herein, so the effects of multiple variables could be minimized. Moreover, given a standard protocol administered at the same institute and all radiographs taken in the neutral position, positional differences were minimized in this study. Lastly, our study includes relatively short follow-up results. However, we interested in the immediate improvements in sagittal alignment after PCF in the clinical field. In this study, we hypothesized that preoperative loss of cervical lordosis can be a distorted reflection and focus on the short-term results.
Conclusions
As shown by postoperative plain radiographs, a significant proportion of our patients showed improvement in sagittal alignment short-term after PCF, and it was well maintained on follow-up. It was more dominant in radiculopathy due to disc herniation, without foraminal stenosis, and was associated with shorter duration of symptoms. Overall, our data suggest that loss of preoperative cervical lordotic curvature may be a distorted reflection due to pain. Particularly in acute-onset radiculopathies from softened discs, PCF is thus a valid surgical option, despite preoperative loss of normal lordotic sagittal alignment.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors hereby declare that all experiments have been examined and approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All authors declare that written informed consent was obtained from the approved parties for publication of this manuscript and accompanying images.
References
- Scoville WB, Whitcomb BB, McLaurin R. The cervical ruptured disc; report of 115 operative cases. Trans Am Neurol Assoc 1951;56:222-4. [PubMed]
- Frykholm R. Lower cervical nerve roots and their investments. Acta Chir Scand 1951;101:457-71. [PubMed]
- Coric D, Adamson T. Minimally invasive cervical microendoscopic laminoforaminotomy. Neurosurg Focus 2008;25:E2. [Crossref] [PubMed]
- Pal GP, Sherk HH. The vertical stability of the cervical spine. Spine 1988;13:447-9. [Crossref] [PubMed]
- Bell DF, Walker JL, O’Connor G, et al. Spinal deformity after multiple level cervical laminectomy in children. Spine 1994;19:406-11. [Crossref] [PubMed]
- Kaptain GJ, Simmons NE, Replogle RE, et al. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg 2000;93:199-204. [PubMed]
- Katsumi Y, Honma T, Nakamura T. Analysis of cervical instability resulting from laminectomies for removal of spinal cord tumor. Spine 1989;14:1171-6. [Crossref] [PubMed]
- White AA III, Johnson RM, Panjabi MM, et al. Biomechanical analysis of clinical stability in the cervical spine. Clin Orthop 1975.85-96. [Crossref] [PubMed]
- Scoville WB, Dohrmann GJ, Corkill G. Late results of cervical disc surgery. J Neurosurg 1976;45:203-10. [Crossref] [PubMed]
- Jöllenbeck B, Fernandez N, Firsching R. Titanium or polymethylmethacrylate in cervical disc surgery? A prospective study. Zentralbl Neurochir 2001;62:200-2. [Crossref] [PubMed]
- Matgé G. Cervical cage fusion with 5 different implants: 250 cases. Acta Neurochir (Wien) 2002;144:539-49. [Crossref] [PubMed]
- Senter HJ, Kortyna R, Kemp WR. Anterior cervical discectomy with hydroxylapatite fusion. Neurosurgery 1989;25:39-42. [Crossref] [PubMed]
- Smith GW, Robinson RA. The treatment of certain cervical spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607-24. [Crossref] [PubMed]
- Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery 2002;51:S37-45. [Crossref] [PubMed]
- Hilton DL Jr. Minimally invasive tubular access for posterior cervical foraminotomy with three-dimensional microscopic visualization and localization with anterior/posterior imagings. Spine J 2007;7:154-8. [Crossref] [PubMed]
- Kulkarni V, Rajshekhar V, Raghuram L. Accelerated spondylotic changes adjacent to the fused segment following central cervical corpectomy: magnetic resonance imaging study evidence. J Neurosurg 2004;100:2-6. [PubMed]
- Maiman DJ, Kumaresan S, Yoganandan N, et al. Biomechanical effect of anterior cervical spine fusion on adjacent segments. Biomed Mater Eng 1999;9:27-38. [PubMed]
- Raynor RB, Moskovich R, Zidel P, et al. Alterations in primary and coupled neck motions after facetectomy. Neurosurgery 1987;21:681-7. [Crossref] [PubMed]
- Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg 1985;63:278-82. [Crossref] [PubMed]
- Albert TJ, Vacarro A. Postlaminectomy kyphosis. Spine 1998;23:2738-45. [Crossref] [PubMed]
- Jagannathan J, Sherman JH, Szabo T, et al. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte diseases: a single surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine 2009;10:347-56. [Crossref] [PubMed]
- Fineman S, Borrelli FJ, Rubinstein BM, et al. The Cervical Spine: Transformation of the Normal Lordotic Pattern into a Linear Pattern in the Neutral Posture. J Bone Joint Surg Am 1963;45:1179-83. [Crossref] [PubMed]
- Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine 2001;26:2463-6. [Crossref] [PubMed]
- Harrison DD, Janik TJ, Troyanovich SJ, et al. Comparisons of lordotic cervical spine curvatures to a theoretical ideal model of the static sagittal cervical spine. Spine 1996;21:667-75. [Crossref] [PubMed]
- Helliwell PS, Evans PF, Wright V. The straight cervical spine: does it indicate muscle spasm? J Bone Joint Surg Br 1994;76:103-6. [Crossref] [PubMed]
- Kettner NW, Guebert GM. The radiology of cervical spine injury. J Manipulative Physiol Ther 1991;14:518-26. [PubMed]
- Kristjansson E, Jonsson H Jr. Is the sagittal configuration of the cervical spine changed in women with chronic whiplash syndrome? A comparative computer-assisted radiographic assessment. J Manipulative Physiol Ther 2002;25:550-5. [Crossref] [PubMed]


