The clinical and radiological outcomes of multilevel posterior lumbar interbody fusion in the treatment of degenerative scoliosis: a consecutive case series with minimum 2 years follow up
Introduction
Adult scoliosis is a common condition affecting the older population (1,2), a section of our society which is continuing to grow rapidly (3,4). The global burden of adult spinal deformity (ASD) is large compared with other self-reported chronic conditions in the general population (5-7). It is well recognized that the restoration of a harmonious coronal and sagittal spinopelvic alignment (8,9) is the main goal of the surgical treatment in adult spinal deformity.
The availability of progressively more sophisticated surgical techniques and improved medical support strategies have made attempts at comprehensive reconstruction of complex structural deformities with neurologic manifestations more feasible (10). The surgical treatment of adult deformities is complicated by the host of medical co-morbidities that are frequently encountered in this patient group. A recent prospective study showed a mortality rate of 0.6% within six weeks and reported 469 complications (207 minor; 262 major) in a patient population of 346. The mean number of complications per patient was 1.61 and 69.8% of patients experiencing at least one complication at some point during the perioperative time or a minimum two-year follow-up (11).
In our institution, we routinely employ multilevel posterior interbody fusion (MPLIF) for the treatment of severe or moderate but flexible curves. Patients whose deformity demonstrates >30% correction on bending radiographs do not require osteotomies, because they are considered flexible (8). Cloward (12) introduced the technique of posterior interbody fusion in 1953. This method has the advantage of achieving direct and indirect decompression of neural elements, restoration of disc height and spinal alignment (8) and 360-degree arthrodesis, all from a single, posterior approach. This classic surgical procedure has been further refined and has correction capabilities similar to that of a pedicle subtraction osteotomy (PSO) or anterior column realignment (ACR) (13-15).
In this study, we analyzed the mortality and morbidity of MPLIF for the treatment of degenerative scoliosis. There is limited information available in the literature on the mortality and morbidity rate following MPLIF for adult degenerative scoliosis (ADS). The secondary aim of the study was to analyze the clinical and radiological outcomes of MPLIF for adult deformities, and patients’ satisfaction with surgery.
Methods
This is a retrospective review of prospectively collected demographic, radiographic, surgical and clinical outcomes from a specialized center for deformity surgery. All patients with the diagnosis of degenerative scoliosis that had surgery consisting of multilevel posterior interbody fusion (MPLIF) between 2009–2015 were included in the study. We defined as degenerative scoliosis any spinal deformity in a skeletally mature patient with a Cobb angle of more than 20° in the coronal plane (2,5), 11 degrees mismatch between lumbar lordosis (LL) and pelvic incidence (PI) (9), and a pelvic tilt larger than 25 degrees (5,7). This definition is in line with the work published by Schwab (2), European Spine Study Group (ESSG) (5) and International Spine Study Group (ISSG) (7). All patients with pre-existent multilevel fusion (> two instrumented levels), known diagnosis of ankylosing spondylitis or any other inflammatory conditions, posttraumatic or post infectious deformities were excluded from this study. Research approval was not required, as this study was conducted for ‘service evaluation’ as per our Hospital’s guidelines.
Surgical data
The surgical details recorded were the number of interbody fusions performed, the number of instrumented levels, and whether fusion to the pelvis was performed at the index procedure. The cell saver device and the multimodal intraoperative monitoring (Natus Neuro Xltek Protektor 32 IOM) (somatosensory-evoked potentials: SSEP/transcranial motor-evoked potentials: TCe-MEP/Free running electromyography Fr-EMG) were used for every patient. Data on intra-operative or postoperative blood transfusion was also recorded. We further noted the length of the hospital stay and the number of days spent in the neurosurgical high dependency unit (NHDU).
Clinical outcomes
Data on clinical outcomes were collected pre-operatively, at 6, 12 and 24 months after surgery. Patients were requested to complete the Core Outcome Measures Index (COMI) (16) and EuroQol-5D (17) questionnaire. The COMI is a self-administered multidimensional instrument that consists of seven items to assess the extent of the patient’s back pain and leg pain, difficulties with functioning in everyday life, symptom-specific well-being, general quality of life, and social and work disability (16). The EuroQol-5D measures 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each has 3 levels: no problems, some problems, extreme problems (17).
The postoperative follow-up form included two questions pertaining to patients’ satisfaction: “how much did the operation help your back problem?” and “how satisfied were you with your overall medical care?” (17).
This process was carried out completely independent of the surgical team by clerks who collect outcome data for all spinal surgeries undertaken at our center.
Complication recording and analysis
All complications were recorded prospectively, and patient reported complications retrospectively recorded. These were reviewed in regular morbidity and mortality meetings. Reoperations reported by the patients and recorded in Spine Tango were cross-checked against our in-house outcomes database, and further enquired about if there were discrepancies. Complications were classified as major or minor according to Glassman’s criteria (18).
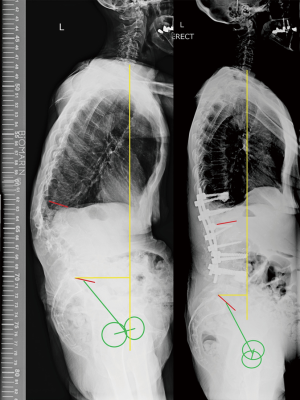
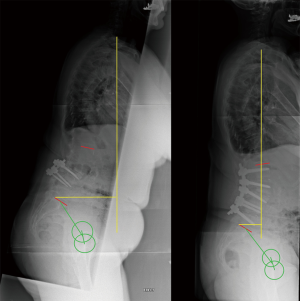
Radiographical data
All patients were assessed radiologically with standardized whole spine standing X-rays. The radiological parameters assessed were LL (angle between superior endplate of L-1 and superior endplate of S-1); sagittal vertical axis (SVA) (the linear offset of C7 in regard to the posterosuperior corner of S1); thoracic kyphosis (TK) (the angle between the superior endplate of the highest measurable thoracic vertebra (usually T2 or T4) and the lower endplate of T12) and PI (angle between the perpendicular to the sacral plate at its midpoint and the line connecting this point to the femoral head axis). Coronal plane deformity was assessed by measuring the Cobb angle of the major curve. Two independent observers performed the measurements on preoperative, immediate postoperative and 2-year follow up X-rays.
Statistical analysis
Inter-observer reliability was assessed for both pre- and post-operative measurements by calculation of the intra-class correlation coefficient (ICC). Subject to high levels of reliability being observed, the means of the measurements recorded by each surgeon were used in subsequent calculations. Distribution of variables was presented as a mean and standard deviation (+/−). All data were analyzed statistically using ANOVA, a paired or unpaired t-test as appropriate. The level of significance for all tests was defined as P<0.05 (JMP version 13, SAS Institute).
Results
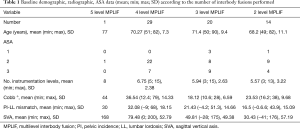
Demographic and surgical data (Table 1)
Full table
Our study involved 13 males and 51 females with a mean age of 70.26 (range, 49–90, SD 8.9). The mean radiological and re-operation follow-up was 5 years and 4 months (min 3 years, max 9 years). Preoperative ASA grade was one in three patients, two in 40 patients, three in 21 patients. The average BMI was 27.13 (range 19.7–36.2, SD 4.52). Thirty-seven patients (57.81%) had no co-morbidities, 21 (32.81%) had one co-morbidity and 6 (9.3%) had two or more co-morbidities. Fourteen (21.87%) of the patients had previous lumbar spine surgery, either discectomy or decompression, while five of the patients had previous 1 level fusion. The mean length of hospital stay was 13 days (min 4, max 31, SD 7.98) while the mean length of postoperative stay in the neurosurgical high dependency unit (NHDU) (level 2 care) was 1.95 days (min 1, max 10, SD 1.83).
The average number of instrumented levels was 6.31 (min 3, max 15, SD 2.649). Fifty-nine patients (92.18%) had the lowest instrumented vertebra (LIV) as L5, whereas 5 patients (7.81%) required fusion to pelvis during the index procedure. The fusion to pelvis was performed by utilizing pelvic bolts and side connectors. MPLIF was performed at five levels in 1 patient (1.56%), four levels in 29 patients (45.31%), three levels in 20 patients (31.25%), and two levels in 14 patients (21.85%). Thirteen (20.31%) patients required delayed extension to pelvis. At all levels a bilateral approach was performed, with pedicle screw placement (Stryker XIA) and 8 degrees PEEK lordotic cages were inserted (Stryker OIC) (Figures 1 and 2). The bilateral approach allows adequate release of the facet joints and insertion of asymmetrical cages which facilitates the correction in the coronal plane. We prefer to position the lordotic cages in the posterior third of the disc. This reduces the risk of iatrogenic foraminal narrowing and helps with the increase of the LL, particularly with a 360 release.
No patients were lost to surgical and radiological follow-up. Of the 64 patients we had pre-operative and post-operative clinical outcomes available for 53 patients (83%).
Radiological findings (Table 2)

Full table
The mean preoperative Cobb angle was 30.52° (min 20.8°, max 79°, SD 6.58°), whereas the mean postoperative Cobb angle was 8.95° range (min 0°, max 26°, SD 7.08°). Preoperative LL was 28.05° (min −21°, max 57.7°, SD 18.21°) preoperatively, while postoperatively it was 41.4° (min 11.5°, max 63.2°, SD 10.86°). The PI-LL mismatch decreased from 25.35° (min 11, max 68°, SD 17.32°) to 9.81° (min −18°, max 38°, SD 13.58°) at 2 years follow-up. The average preoperative SVA was 60.86 mm (min −41 mm, max 200 mm, SD 56.88°) with 14 (21%) patients presenting an SVA >100 mm, and 16 (25%) patients demonstrating an SVA >50 mm. Mean postoperative SVA was 45.86 (min −60, max 158, SD 41.48). At 2 year follow up the mean SVA was 49.60 (min −42, max 142, SD 38.21).
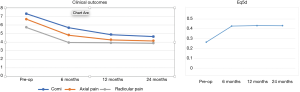
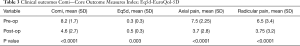
Clinical outcomes (Table 3 and Figure 3)
Full table
The preoperative Eq5D average was 0.3 (SD 0.3). The postoperative Eq5D was 0.5 (SD 0.3) at a mean follow-up of 2 years. The preoperative COMI score was 8.2 (SD 1.7). The final COMI score at a mean of 2 years follow-up was 4.6 (SD 2.7) There were statistically significant improvements in COMI (P<0.0001) and Eq5D scores postoperatively (P=0.003). Sixty-seven percent of patients achieved the minimum clinically important difference in COMI score of 2.2 points post-operatively (19).
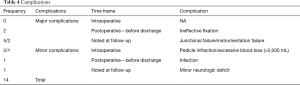
Complications (Table 4)
Full table
A total of five patients developed proximal junctional kyphosis that required surgical intervention at various intervals following the initial surgery. One patient presented prolonged wound discharge post procedure which responded well to repeated wound washouts, antibiotic therapy and negative pressure wound therapy. There were no vascular injuries. One patient developed a delayed L5/S1 disc prolapse with symptoms of S1 radiculopathy and required decompression and revision fusion to the pelvis. There were no mortalities related to the surgery.
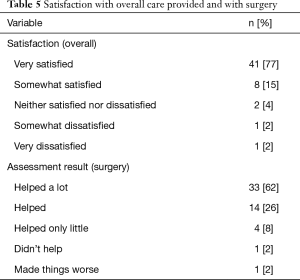
Patient’ satisfaction (Table 5)
Full table
Forty-one (77%) patients were extremely satisfied with overall care provided, eight (15%) patients were somewhat satisfied whereas two (4%) patients were dissatisfied. Thirty-three (62%) patients felt that the surgery helped a lot, 14 (26%) patients felt that the surgery helped, four (8%) patients felt that surgery helped just a little whereas only one (2%) patient reported no improvement after the surgery. None of the patients included in this study reported a deterioration in their overall function post-surgery.
Discussion
In this paper we present our experience with the use of multilevel posterior interbody fusion in the treatment of degenerative scoliosis. Surgical treatment for adult degenerative deformities aims to restore the sagittal balance, decompress the neural elements to minimize complication and pain, and improve quality of life (20). Despite significant technical advances, there is an ongoing debate about the safety of surgical treatment for degenerative scoliosis in elderly patients, and the most appropriate surgical approach.
Proponents of newer techniques such as minimally invasive surgery, lateral-, oblique- or anterior-based techniques argue that classic open techniques, particularly in elderly patients, have a significant risk of complications (21-23). Certainly, three-column osteotomies have been associated with significant blood loss and neurologic complication (24-26). Elderly patients are particularly at risk, given their comorbidities and poor healing potential (27). Recently, Bae published a study on the clinical and radiological results of anterior interbody fusion plus posterior spinal fixation (ALIF + PSF), lateral interbody fusion (LLIF) + PSF and PSF-only in the treatment of adult deformities. On average their patients were 5 years younger than the patients included in this paper. The study showed that the infection rate of all patients was 18.6%. Furthermore, 12.7% of all patients required revision due to PJK and 25.3% required revision due to non-PJK, with a total revision rate of 38% at a mean follow-up of 34 months. In this study the average increase in LL was only 11.2° for LLIF and 8.4° for ALIF. Despite a staged anterior-posterior surgical interventions and high complication rate, all HRQoL scores were significantly improved at a mean of 34 months follow-up (28). As an alternative, a posterior disc-based procedure in the form of multilevel posterior interbody fusion can result is satisfactory correction of the sagittal and coronal plane deformity (13,15,29,30) in cases where a posterior fusion mass is not present. Furthermore, a posterior approach allows simultaneous access to anterior and posterior columns of the spine. In cases of degenerative changes to the disc and facet joints, combined with spinal stenosis, the spine becomes rigid and difficult to mobilize. A posterior interbody fusion can provide a 360-degree release that includes the disc, the facet joint, and the osteophytes all from a posterior approach (13,30). Furthermore, by releasing the anterior longitudinal ligament and the annulus, significantly more correction per level can be achieved, and the amount of correction can be titrated, so that a physiological lordosis can be achieved (13-15). This is in contrast with anterior- or lateral-based procedures, where a separate approach for posterior release and instrumentation is required. It is our practice to instrument only to the lumbar or the lower thoracic spine. The number of interbody fusions performed is based on the amount of lordosis required, as determined during the pre-operative planning. Our results suggest that even in elderly patients with multiple comorbidities and severe deformities, open techniques do not necessarily result in increased mortality or morbidity.
Primary fusion to the pelvis using either S1 screws or sacroiliac fixation risks intraoperative complications because of increased blood loss and length of operation and generates a particular set of postoperative problems. Iliac screws will not guarantee a fusion across L5/S1 even when supplemented with anterior support and a substantial percentage of iliac screws will loosen, break, or show some disconnect between the S1 and iliac screws at ultimate follow-up (31-33). Also, it has been shown that delayed fusion to the pelvis does result in similar clinical outcomes as compared with primary fusion to the pelvis (34). It is our routine practice to use L5 as our LIV and subsequently extend our fusion to the pelvis as a staged procedure if required. A primary fusion to pelvis is only considered in the presence of L5/S1 central, lateral recess or foraminal stenosis with concomitant radicular symptoms.
Our study has several limitations. We performed a retrospective review of prospectively collected data. Our study includes only patients from a single center and lacks a comparative group. As this was real world data, we were able to obtain complete clinical outcomes for only 83% of our patients. However, the clinical results were collected prospectively and independently of the surgical team. We have demonstrated statistically significant improvement in COMI, Eq5D, axial pain and radicular pain postoperatively. Our hospital stay was longer that what is currently reported in the literature. However, our cohort of patients was in average 5 years older than in most reported series and did not benefit from the early rehabilitation protocols which we recently implemented (35).
We have also demonstrated a lower complication rate than reported in literature. In our opinion, by performing a disc-based procedure with a 360 release and avoiding a primary fusion to pelvis, degenerative deformity surgery can be performed with an acceptable risk of complications. A large percentage of our patients were extremely satisfied with the outcome of the surgery and noticed a significant improvement in their quality of life. The MPLIF technique was further refined to include a segmental annular and anterior longitudinal release, and we found increased segmental correction capabilities in cases of adult deformity and high-grade spondylolisthesis (14,15). Potential future work in this area that we plan to carry out is establishing whether the ALL release plus MPLIF can restore the physiological lordosis, and thus reduce the risk of PJK or eliminate the need for a lumbopelvic fusion.
Conclusions
Multilevel interbody fusion is a safe procedure, and in selected cases can result in good clinical and radiological outcomes and improvement in patient quality of life.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. NHS Rec approval not required for this service evaluation. Written consent gained from all patients to use collected data.
References
- Urrutia J, Diaz-Ledezma C, Espinosa J, et al. Lumbar scoliosis in postmenopausal women: prevalence and relationship with bone density, age, and body mass index. Spine 2011;36:737-40. [Crossref] [PubMed]
- Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine 2005;30:1082-5. [Crossref] [PubMed]
- Fehlings MG, Tetreault L, Nater A, et al. The Aging of the Global Population: The Changing Epidemiology of Disease and Spinal Disorders. Neurosurgery 2015;77 Suppl 4:S1-5. [Crossref] [PubMed]
- Szpalski M, Gunzburg R, Melot C, et al. The aging of the population: a growing concern for spine care in the twenty-first century. Eur Spine J 2003;12 Suppl 2:S81-3. [Crossref] [PubMed]
- Pellisé F, Vila-Casademunt A, Ferrer M, et al. Impact on health-related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 2015;24:3-11. [Crossref] [PubMed]
- Schwab F, Dubey A, Pagala M, et al. Adult scoliosis: a health assessment analysis by SF-36. Spine 2003;28:602-6. [Crossref] [PubMed]
- Bess S, Line B, Fu KM, et al. The Health Impact of Symptomatic Adult Spinal Deformity: Comparison of Deformity Types to United States Population Norms and Chronic Diseases. Spine 2016;41:224-33. [Crossref] [PubMed]
- Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurgical focus 2010;28:E1. [Crossref] [PubMed]
- Smith JS, Klineberg E, Schwab F, et al. Change in classification grade by the SRS- Schwab Adult Spinal Deformity Classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine 2013;38:1663-71. [Crossref] [PubMed]
- Howe CR, Agel J, Lee MJ, et al. The morbidity and mortality of fusions from the thoracic spine to the pelvis in the adult population. Spine 2011;36:1397-401. [Crossref] [PubMed]
- Smith JS, Klineberg E, Lafage V, et al. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. Journal of neurosurgery Spine 2016;25:1-14. [Crossref] [PubMed]
- Cloward RB. The treatment of ruptured lumbar intervertebral discs; criteria for spinal fusion. Am J Surg 1953;86:145-51. [Crossref] [PubMed]
- Sweet FA, Sweet A. Transforaminal Anterior Release for the Treatment of Fixed Sagittal Imbalance and Segmental Kyphosis, Minimum 2-Year Follow-Up Study. Spine Deformity 2015;3:502-11. [Crossref] [PubMed]
- Shrijit Panikkar SS, Siddique I, Verma R, et al. Reduction of high-grade spondylolisthesis through a posterior approach and restoration of the pelvic parameters. Spine J 2016;16:S66. [Crossref]
- Silviu Sabou SP, Siddique I, Verma R, et al. Circumferential annular and anterior longitudinal ligament release from a posterior approach in the treatment of adult degenerative scoliosis. Spine J 2017;17:S4. [Crossref]
- Mannion AF, Vila-Casademunt A, Domingo-Sabat M, et al. The Core Outcome Measures Index (COMI) is a responsive instrument for assessing the outcome of treatment for adult spinal deformity. Eur Spine J 2016;25:2638-48. [Crossref] [PubMed]
- Mueller B, Carreon LY, Glassman SD. Comparison of the EuroQol-5D with the Oswestry disability index, back and leg pain scores in patients with degenerative lumbar spine pathology. Spine (Phila Pa 1976) 2013;38:757-61. [Crossref] [PubMed]
- Glassman SD, Hamill CL, Bridwell KH, et al. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine 2007;32:2764-70. [Crossref] [PubMed]
- Mannion AF, Porchet F, Kleinstück FS, et al. The quality of spine surgery from the patient's perspective: part 2. Minimal clinically important difference for improvement and deterioration as measured with the Core Outcome Measures Index. Eur Spine J 2009;18 Suppl 3:374-9. [Crossref] [PubMed]
- Oskouian RJ Jr, Shaffrey CI. Degenerative lumbar scoliosis. Neurosurg Clin N Am 2006;17:299-315. vii. [Crossref] [PubMed]
- Wang MY, Mummaneni PV. Minimally invasive surgery for thoracolumbar spinal deformity: initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus 2010;28:E9. [Crossref] [PubMed]
- Anand N, Baron EM, Khandehroo B, et al. Long-term 2- to 5-year clinical and functional outcomes of minimally invasive surgery for adult scoliosis. Spine 2013;38:1566-75. [Crossref] [PubMed]
- Leveque JC, Yanamadala V, Buchlak QD, et al. Correction of severe spinopelvic mismatch: decreased blood loss with lateral hyperlordotic interbody grafts as compared with pedicle subtraction osteotomy. Neurosurg Focus 2017;43:E15. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine 2007;32:2189-97. [Crossref] [PubMed]
- Buchowski JM, Bridwell KH, Lenke LG, et al. Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine 2007;32:2245-52. [Crossref] [PubMed]
- Cho SK, Bridwell KH, Lenke LG, et al. Major complications in revision adult deformity surgery: risk factors and clinical outcomes with 2- to 7-year follow-up. Spine 2012;37:489-500. [Crossref] [PubMed]
- Hassanzadeh H, Jain A, El Dafrawy MH, et al. Three-column osteotomies in the treatment of spinal deformity in adult patients 60 years old and older: outcome and complications. Spine 2013;38:726-31. [Crossref] [PubMed]
- Bae J, Theologis AA, Berven S, et al. Comparative analysis of 3 surgical strategies for adult spinal deformity with mild to moderate sagittal imbalance. J Neurosurg Spine 2018;28:40-9. [Crossref] [PubMed]
- Sabou S, Tseng TH, Stephenson J, et al. Correction of sagittal plane deformity and predictive factors for a favourable radiological outcome following multilevel posterior lumbar interbody fusion for mild degenerative scoliosis. Eur Spine J 2016;25:2520-6. [Crossref] [PubMed]
- Matsumura A, Namikawa T, Kato M, et al. Posterior corrective surgery with a multilevel transforaminal lumbar interbody fusion and a rod rotation maneuver for patients with degenerative lumbar kyphoscoliosis. J Neurosurg Spine 2017;26:150-7. [Crossref] [PubMed]
- Cho W, Mason JR, Smith JS, et al. Failure of lumbopelvic fixation after long construct fusions in patients with adult spinal deformity: clinical and radiographic risk factors: clinical article. J Neurosurg Spine 2013;19:445-53. [Crossref] [PubMed]
- Weistroffer JK, Perra JH, Lonstein JE, et al. Complications in long fusions to the sacrum for adult scoliosis: minimum five-year analysis of fifty patients. Spine 2008;33:1478-83. [Crossref] [PubMed]
- Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine 2006;31:2329-36. [Crossref] [PubMed]
- Fu KM, Smith JS, Burton DC, et al. Revision extension to the pelvis versus primary spinopelvic instrumentation in adult deformity: comparison of clinical outcomes and complications. World Neurosurg 2014;82:e547-52. [Crossref] [PubMed]
- Angus M, Jackson K, Smurthwaite G, et al. The implementation of enhanced recovery after surgery (ERAS) in complex spinal surgery. J Spine Surg 2019;5:116-23. [Crossref] [PubMed]