
Ultrasound guided paraspinal intrafascial plane blocks for postoperative analgesic on spine surgery
We had the pleasure of reading the article by Williams et al. (1), entitled “Are dorsal ramus nerve blocks the solution to postoperative lumbar spine surgery pain?” Your outcomes drew our attention as we believe we have some opposing evidence that there is in fact a benefit.
The dorsal ramus nerve block described had some variability in how it was administered which could lead to a discrepancy in analgesic effects. Anatomic variations exist and without the sensitivity of an ultrasound guided or nerve stimulator, it would be hard to account for minor variations amongst patients which could produce inconsistent results. One additional argument can be made that with a blind surgical infiltration technique, the reported analgesic effects may only be upwards of 2 h. It is worth noting that there may be a chance that some infiltration of the paraspinal intrafascial space did occur inadvertently which would potentially prolong this effect.
From a purely surgical perspective we know that exposure tends to be midline and requires the retraction of muscle and violation of fascial planes. As such, we believe there is a high probability of administered local anesthetic being evacuated from the space as a direct result of suctioning intraoperatively. For these reasons we feel that although the premise behind the study is a strong one, it is flawed.
We propose that local anesthetic injection can actually be greatly beneficial to this patient group. It is known that erector spinae plane (ESP) blocks have been of great interest and they specifically target dorsal rami. Although the nomenclature is different, the mechanism of action of both blocks (dorsal ramus block and ESP) is in essence the same. A concern with these blocks, however, is the high possibility of ventral spread, and although not fully understood, the possibility of spread into the paravertebral space (2). An additional concern, specific to laminectomy surgery, is the violation of the epidural space. With that in mind, it should be noted that spread into the epidural space is a possibility. This variable spread and potential for large volumes of anesthetics into the paravertebral and epidural space once again demonstrate that the risk far outweighs the benefit (3).
An area of great importance in neurosurgery is the ability to perform an immediate postoperative neurologic check. Given what we know about the dorsal ramus nerve block and erector spinae block, there is reason to believe that these neurovascular checks will be flawed. This in turn may lead to unnecessary patient testing, acquisition of imaging, admission to critical care units and in the worst case scenario, surgical reexploration if the concern is strong enough.
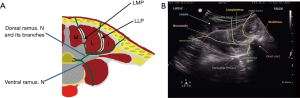
A subset of regional anesthesia technique that is still under investigation but that has very promising preliminary outcomes stem from older nomenclature. Ultrasound guided thoracolumbar interfascial plane block (TLIP), or lumbar multifidus plane (LMP) block, a member of paraspinal intrafascial plane (PIP) blocks family (4), It has been demonstrated that these blocks target the dorsal ramus of spinal nerve with particular benefit to patients for analgesic effects specifically for spine surgery (5). These blocks have been quite efficacious in helping patients undergoing laminectomy surgery. They are safe as their primary target is specific to the dorsal ramus nerve and its branches. It is considered an interfascial injection. We have started to refer to these as PIP blocks (Figure 1). The blocks are done under ultrasound and although there is violation of muscle and fascia, it is a relative easy block to perform and may be done in one of two locations safely (6). The LMP (also was called “TLIP”) and the lumbar longissimus plane (LLP, also was called “modified TLIP”) are both considered appropriate targets for this injection if one plane has more tissue edema and subsequently becomes more challenging to visualize.
While there is still more formal research to be done, in our subset of patients we have seen great benefit with little risk. We are optimistic that with reproducible and consistent results, the future of spine surgery can be transitioned to outpatient procedures with superior analgesic outcomes.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Williams MG, Rigney B, Wafai A, et al. Are dorsal ramus nerve blocks the solution to postoperative lumbar spine surgery pain? J Spine Surg 2019;5:245-50. [Crossref] [PubMed]
- Kot P, Rodriguez P, Granell M, et al. The erector spinae plane block: a narrative review. Korean J Anesthesiol 2019;72:209-20. [Crossref] [PubMed]
- Tseng V, Tara A, Hou J, et al. Erector spinae plane block unbound: Limits to safety in a patient with laminectomy. Saudi J Anaesth 2019;13:253-4. [Crossref] [PubMed]
- Xu JL, Tseng V. Proposal to standardize the nomenclature for paraspinal interfascial plane blocks. Reg Anesth Pain Med 2019;44:1106-7. [PubMed]
- Ueshima H, Hara E, Otake H. Thoracolumbar interfascial plane block provides effective perioperative pain relief for patients undergoing lumbar spinal surgery; a prospective, randomized and double blinded trial. J Clin Anesth 2019;58:12-7. [Crossref] [PubMed]
- Tseng V, Xu JL. Erector Spinae Plane Block For Postoperative Analgesia in Lumbar Spine Surgery: Is There a Better Option? J Neurosurg Anesthesiol 2019. [Epub ahead of print]. [Crossref] [PubMed]


