
Radiological outcomes following hyperlordotic cage insertion in anterior cervical discectomy and fusion
Introduction
Cervical alignment is associated with quality of life and myelopathy (1-3). Kyphosis correlates with increased neck pain and predicts less postoperative neurological improvement. Despite this indications and standards for surgical correction of cervical alignment are not well-defined.
Anterior cervical discectomy and fusion (ACDF) is a common operation performed for neural decompression and treatment or prevention of myelopathy. It involves removal of the degenerate disc at the pathological spinal level and replacing it with a parallel or angled plastic or titanium cage packaged with autologous or artificial bone graft. Most ACDFs performed globally use cages of no more than 10° lordosis. There is no published study examining the utilisation of 15° hyperlordotic cages. It is unknown whether these cages lead to a significant increase in device level lordosis or merely an increase in disc space height. It is also unknown whether these cages affect other clinically significant parameters of spinal alignment. If it can be shown that hyperlordotic cages result in consistently improved cervical alignment, their wider utilisation can be statistically justified, and their impact on disability scores and myelopathy outcomes further explored.
There are no standardised methods of measuring cervical alignment, nor universal definitions of threshold parameter values. The Cobb angle is a commonly reported measurement of cervical curvature from C1−7 or C2−7 (4). Cobb angles are easily obtained and have excellent inter- and intra-rater reliability. Normal cervical lordosis from C2 to C7 has been defined as approximately 9.6°, but can vary from 5° to >40°, generally increasing with age.
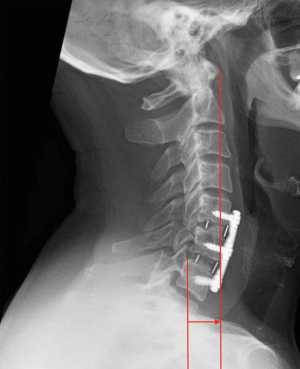
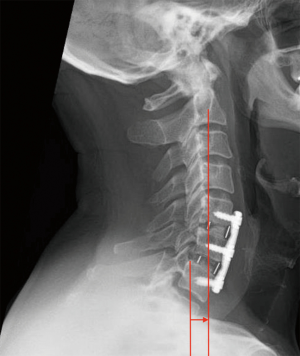
Sagittal plane translation as measured by the sagittal vertical axis (SVA) correlates with quality of life scores. The C2 to C7 SVA is the distance between one plumb line from the centre of the body of C2 and another plumb line from the posterosuperior angle of the C7 vertebral body. Variations include centre-of-gravity to C7 SVA and C1 to C7 SVA. C2 to C7 SVA appears particularly relevant, with a value of >40 mm significantly associated with worse neck disability index scores (5).
Methods
This is a two-part retrospective analysis of radiological cervical parameters in two groups of patients. The first group comprises of 40 consecutive patients who underwent ACDF with plate by the third author using hyperlordotic (15 degree) cages at Westmead Private Hospital in Sydney Australia between 2015 and 2017. The second group comprises 40 consecutive patients who underwent ACDF with plate supervised by the third author using standard lordosis cages at Westmead Public and Private Hospitals in Sydney Australia between 2013 to 2017. The maximum lordosis in the standard group was 8°. Radiographic images were collected from multiple privatised and public hospital picture archiving and communication systems (PACS).
Part one—comparison within groups
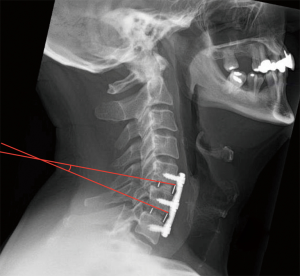
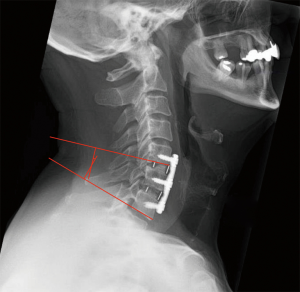
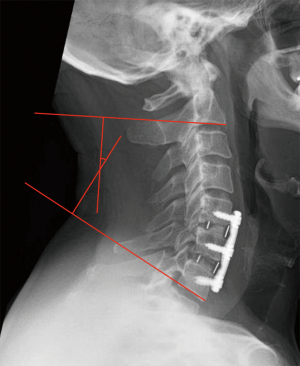
Within each patient group, the following pre and post-operative radiographical parameters were measured: device level Cobb angle at each operative level (Figure 1); accumulative segmental Cobb angle for two or more levels (Figure 2); Global C2−C7 Cobb angle (Figure 3); C1−C7 SVA (Figure 4); C2−C7 SVA (Figure 5). These measurements were acquired using the Surgimap™ program. The preoperative mean of each parameter was compared with the postoperative mean of the same parameter, and a paired t-test was used to test the change observed for each parameter, with an assigned 5% significance level.
Each group of patients was further dichotomized based on age (<65 vs. ≥65 yo) and preoperative global alignment (lordotic vs. kyphotic), and the postoperative changes in the mean of each parameter were compared between subgroups.
Part two—comparison between groups
Postoperative changes in the aforementioned cervical alignment parameters were compared between hyperlordotic cage patients and standard lordotic cage patients. The significance of those changes was analysed with a paired t-test with a 5% significance level. Subgroup analyses were conducted in (I) patients with preoperative global lordosis; (II) patients with preoperative global kyphosis; (III) patients <65 yo; and (IV) patients ≥65 yo. All data analysis was conducted through the SPSS software.
Results
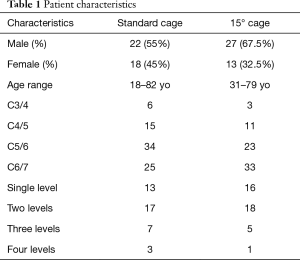
In the standard cage group, there were 18 females and 22 males. Patients were aged between 18 and 82 at time of operation. In the fifteen-degree group, there were 13 females and 27 males. Patients were aged between 31 to 79 at time of operation (Table 1). In this study kyphosis was designated a negative number and lordosis was designated a positive number.
Full table
Part one—comparison within groups
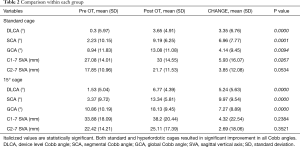
Within the standard cage group, preoperative device level Cobb angle ranged from −23.6° to 12.3°, with a mean of 0.3°. Postoperative device level Cobb angle ranged −14.2° to 16°, with a mean of 3.65°. There is a statistically significant improvement of 3.35° towards lordosis. Preoperative segmental Cobb angle for two or more levels ranged from −25° to 24.1°, with a mean of 2.23°. Postoperative segmental Cobb angle ranged from −10.9° to 21.5°, with a mean of 9.19°. There is a statistically significant improvement of 6.96° towards lordosis. Preoperative global Cobb angle ranged from −19.2° to 31.2°, with a mean of 8.94°. Post-operative global Cobb angle ranged from −16.7° to 29.6°, with a mean of 13.08°. There is a statistically significant improvement of 4.14° towards lordosis. Overall standard cages showed a significant increase in device level CA (P=0.000), segmental CA (P=0.0001), and global CA (P=0.0094) (Table 2).
Full table
Within the hyperlordotic cage group, preoperative device level Cobb angle ranged from −12.7° to 12.2°, with a mean of 1.53°. Postoperative device level Cobb angle ranged from −1.5° to 16.5°, with a mean of 6.77°. There is a statistically significant improvement of 5.24° towards lordosis. Preoperative segmental Cobb angle for two or more levels ranged from −14.8° to 27°, with a mean of 3.37°. Postoperative segmental Cobb angle ranged from −1.1° to 21.0°, with a mean of 13.34°. There is a statistically significant improvement of 9.97° towards lordosis. Preoperative global Cobb angle ranged from −11.5° to 34.3°, with a mean of 10.86°. Postoperative global Cobb angle ranged from 3.6° to 39.1°, with a mean 18.13°. There is a statistically significant improvement of 7.27° towards lordosis. Overall hyperlordotic cages showed a significant increase in device level CA (P=0.00), segmental CA (P=0.00), and global CA (P=0.00) (Table 2).
Within the standard cage group, preoperative C1-7 sagittal vertical axis ranged from 3 to 72.10 mm, with a mean of 27.08 mm. Postoperative C1-7 SVA ranged from 7 to 61 mm, with a mean of 33 mm. There is a statistically significant change of 5.93 mm (P=0.0267). Preoperative C2-7 SVA ranged from −3 to 52.4 mm, with a mean of 17.85 mm. Postoperative C2-7 SVA ranged from −1.4 to 42.4 mm, with a mean of 21.7 mm. There is a change of 3.85 mm but this did not reach statistical significance (P=0.0534) (Table 2).
Within the hyperlordotic group, C1-7 sagittal vertical axis ranged from 8.9 to 88.5 mm, with a mean of 33.88 mm. Postoperative C1-7 SVA ranged from −19 to 76.5 mm, with a mean of 38.2 mm. There is an average change of 4.32 mm, but this did not reach statistical significance (P=0.2384). Preoperative C2−C7 SVA ranged from −2.3 to 66.8 mm, with a mean of 22.24 mm. Postoperative C2-7 SVA ranged from −25.50 to 57.9 mm, with a mean of 25.11 mm. There is an average change of 2.69 mm but this did not reach statistical significance (P=0.3521) (Table 2).
Analysis of variance was conducted for each parameter at different cervical levels and for each number of operated levels. Within the standard cage group, 6 patients had cage insertion at C3/4, 15 at C4/5, 35 at C5/6, 25 at C6/7, and between those levels there was no significant difference for index level Cobb angle. Within the hyperlordotic cage group, 3 patients had cage insertion at C3/4, 11 at C4/5, 33 at C5/6, 23 at C6/7, and between those levels there was no significant difference for index level Cobb angle (standard group P=0.2423; hyperlordotic group P=0.1926).
In the standard cage group, 13 patients had one level, 17 had two levels, 7 had three levels, 3 had four levels. In the fifteen-degree group, 16 patients had 1 level, 18 had two levels, 5 three levels and 1 patient had four levels. There was no significant difference in segmental or global cobb angle, nor in C1-7 or C2-7 SVA, between the various numbers of operated levels in either the standard cage group or the hyperlordotic group.
Each group of patients were further stratified for age. Postoperative changes in device level, segmental level, and global level Cobb angle were compared between patients <65 yo and those ≥65 yo. Postoperative changes in C1-7 and C2-7 SVA were also compared between the two age groups. There was no statistically significant difference between the two groups in any cervical alignment parameters for either the standard or the hyperlordotic cages.
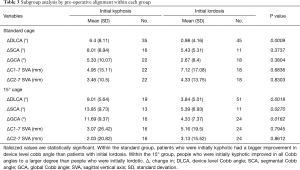
Each group of patients were also stratified for initial global alignment.
Within the standard cage group, patients who were globally kyphotic had a larger statistically significant improvement in device level Cobb angle than patients with initial lordosis (P=0.0009). Segmental and global Cobb angle changes were also larger in absolute values within the kyphotic group than those in the lordotic group, but these did not reach statistical significance (P=0.3737, P=0.3804).
In the hyperlordotic cage group, patients initially kyphotic improved in all angular parameters to a larger degree than people who were initially lordotic. Device level, segmental, and global Cobb angle change differences all reached statistical significance (P=0.0018, P=0.0270, P=0.0162) (Table 3).
Full table
Part two—comparison between groups
Within the standard cage group, changes in device level CA, segmental level CA, and global CA were 3.35°, 6.96°, and 4.14° respectively. Within the hyperlordotic group, those values were 5.24°, 9.97°, and 7.27° respectively. There is a larger absolute change in all Cobb angles in the hyperlordotic group, but these did not reach significance. Differences in SVA changes between the two groups did not reach any statistical or clinical significance (Table 4).
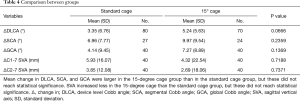
Full table
In the <65 yo group, the change in device level Cobb angle in patients with standard cage insertion ranged from −6.3° to 35°, with an average of 3.72°. The change in device level Cobb angle in patients with hyperlordotic cage insertion ranged from −2.5° to 18.9°, with a higher average of 6.11°. This showed a statistically significant larger change in device level Cobb angle postoperatively for the hyperlordotic group (P=0.0492). This pattern was repeated for segmental and global Cobb angles for the <65 yo patient group, as well as for all Cobb angles for the ≥65 yo group, but these did not reach statistical significance (Table 5).
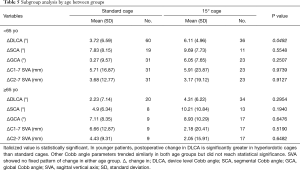
Full table
In initially lordotic patients, the change in device level Cobb angle in patients with standard cages ranged from −6.3° to 13.3°, with an average of 0.98°. The change in device level Cobb angle in patients with hyperlordotic cages ranged from −10° to 14.3°, with a mean of 3.84°. This showed a statistically significant larger change in device level Cobb angle post operatively for the hyperlordotic group (P=0.0033). This pattern was repeated for segmental and global Cobb angles for the preoperatively lordotic group, as well as for all Cobb angles for the preoperatively kyphotic group, but these did not reach statistical significance (Table 6).
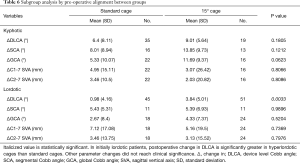
Full table
Discussion
The cervical spine is the most mobile segment of the spinal column, and cervical alignment is associated with myelopathy and quality of life (6). Cadaveric and animal studies indicate that kyphosis alone without necessary cord compression increases longitudinal cord tension and intramedullary pressure, leading to neuronal loss and demyelination likely due to vascular compromise (2,3). Clinical studies show that kyphosis is associated with increased neck pain before and after cervical operation (7). Restoration or enhancement of cervical lordosis is therefore as important a surgical goal as decompression of neural structures in ACDF. Quantitative evaluation of the impact of ACDF prosthesis lordosis on cervical alignment has not been widely reported in the literature. This study confirms that ACDF with plate immediately improves cervical lordosis, regardless of implant lordosis. Our data also shows a trend suggesting increased implant lordosis results in increased global lordosis, however this did not reach statistical significance.
Several study limitations are identified. The retrospective nature of this study generated inevitable bias. The standard cage group was heterogeneous, with implant lordosis ranging from 0° to 10°. The proceduralists, and specifically their levels of experience, could not be controlled, especially among the standard cage patient cohort who underwent surgery in a public teaching hospital.
Imaging modalities were inconsistent in and between patients. Imprecision is likely when measuring alignment between modalities. Cervical alignment in the upright position is most representative of daily living, so the validity of supine MRIs and CTs is debatable. The utility of this study in examining sagittal vertical axis was also severely limited by the supine nature of some comparison images. It is known that cervical alignment is intimately related to thoracolumbar alignment (8,9), and the optimal lordotic configuration of the cervical spine allows the centre of gravity of the head over the femoral heads at rest. Evaluation of sagittal vertical axis therefore should ideally be based on standing 3-foot X-rays. Upright X-rays would allow additional evaluation of chin-brow vertical angle, an important parameter associated with quality of life (10).
This study’s clinical applicability is limited by its timeframe. The surgical effect on alignment in the medium to long term would be relevant, especially upon completion of bony fusion. It may be argued, however, that immediate postoperative assessment would be more reflective of the prosthesis per se, whereas delayed radiological measurements are confounded by other factors such as patient healing and fusion integrity. The association between hyperlordotic cages and subsidence is an important area for exploration, and would require longer radiographical follow-up. It has been suggested, however, that cervical lordosis may be more important for long-term clinical outcome than cage subsidence (11).
The findings of this study indicate that hyperlordotic 15° cages are comparable to standard lordosis cages in improving cervical alignment, but do not statistically support hyperlordotic cages over standard ones. A prospective study involving a larger sample size with a comparison of graded and controlled cage lordosis will be of value, ensuring that all radiographs are acquired upright and modalities are consistent.
Conclusions
Hyperlordotic 15° and standard cages both significantly improve cervical lordosis locally and globally. Hyperlordotic cages tended to affect cervical lordosis to a larger degree than standard cages, but were not shown to be statistically superior to standard cages in this study.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The following study was approved by the Western Sydney Local Health District Research Governance Officer. HREC reference number: LNR/18/WMEAD/73, SSA reference number: LNRSSA/18/WMEAD/74.
References
- Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 2011;68:1309-16; discussion 1316. [Crossref] [PubMed]
- Farley CW, Curt BA, Pettigrew DB, et al. Spinal cord intramedullary pressure in thoracic kyphotic deformity: a cadaveric study. Spine (Phila Pa 1976) 2012;37:E224-30. [Crossref] [PubMed]
- Shimizu K, Nakamura M, Nishikawa Y, et al. Spinal kyphosis causes demyelination and neuronal loss in the spinal cord: a new model of kyphotic deformity using juvenile Japanese small game fowls. Spine (Phila Pa 1976) 2005;30:2388-92. [Crossref] [PubMed]
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2015;76 Suppl 1:S14-21; discussion S21.
- Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673-83. [Crossref] [PubMed]
- Koeppen D, Piepenbrock C, Kroppenstedt S, et al. The influence of sagittal profile alteration and final lordosis on the clinical outcome of cervical spondylotic myelopathy. A Delta-Omega-analysis. PLoS One 2017;12:e0174527. [Crossref] [PubMed]
- Protopsaltis TS, Scheer JK, Terran JS, et al. How the neck affects the back: changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine 2015;23:153-8. [Crossref] [PubMed]
- Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38:S149-60. [Crossref] [PubMed]
- Suk KS, Kim KT, Lee SH, et al. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine (Phila Pa 1976) 2003;28:2001-5. [Crossref] [PubMed]
- Wu WJ, Jiang LS, Liang Y, et al. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J 2012;21:1374-82. [Crossref] [PubMed]


