
The University of Miami spine surgery ERAS protocol: a review of our journey
Enhanced recovery after surgery (ERAS) is a multidisciplinary concerted approach to optimizing post-operative recovery and reducing hospital length of stay. It was first conceived in Denmark for abdominal surgery (1,2). This initiative examined organ/system specific responses to surgical stress and factors compromising these pathophysiologic effects pre-operatively, intra-operatively, and post-operatively. Specific guidelines were developed to modify these stress responses for optimal homeostasis and thereby facilitate patient recovery and hospital discharge (2-5). These programs gained traction in the 1990s and have been widely implemented across the world in other surgical subspecialties (6-8). Although other musculoskeletal surgical disciplines, such as total joint arthroplasty, have generally adopted ERAS (9-12), spine surgery has been slow to embrace this methodology. Unlike total joint arthroplasty, where operations are stereotyped and standardized, the highly variable pathology and technical nature of spine surgeries can necessitate extensive operations requiring prolonged general anesthesia and extensive para-spinal muscle dissection and osteotomies with high blood loss. Consequently, this dramatic multi-organ system pathophysiologic insult to the patient can potentially overpower the smaller cumulative benefits of ERAS. Perhaps this is the primary reason for its slow acceptance in the field of spine surgery.
The core tenets of ERAS are (I) a focus on the patient’s journey through surgery; (II) a multidisciplinary and multimodal approach; (III) development, implementation, and refinement of novel techniques and technologies designed to reduce pain, morbidity, and recovery time; and (IV) data-driven iterative improvement processes (3-5,13). The first step to develop version 1.0 (Table 1) of the University of Miami ERAS protocol was entirely dedicated to improving the standard transforaminal technique for lumbar interbody fusion (TLIF) (5). Although minimally invasive (MIS) techniques have been popularized in degenerative lumbar disease, including the utilization of the mini-open paramedian Wiltse (14) intermuscular corridor as well as tubular muscle splitting retractors, these MIS techniques still require open incisions and muscle dissection (15-17). By leveraging a percutaneous spinal access system (Spineology) with an expandable interbody cage (Optimesh) and a percutaneous endoscopic visualization platform (Joimax), a novel technique for MIS TLIF was developed and will henceforth be referred to as the ERAS TLIF. Endoscopic visualization and decompression of traversing and exiting nerve roots can be achieved through an 8 mm outer diameter working channel. Discectomy and insertion of a 22 or 25 mm expandable mesh interbody cage can also be performed through the same access corridor. Arthrodesis is augmented by using 2.1 mg rhBMP-2 (Infuse, Medtronic) within the disc space to enhance fusion through such a narrow corridor. A percutaneous small caliber MIS pedicle screw system (Depuy Synthes Viper 2 or Viper Prime) is used for intersegmental fixation. Compared to traditional MIS TLIF, this “ultra-MIS” (18) technique is capable of accomplishing the same surgical goals of direct and indirect decompression, reduction of spondylolisthesis, and achievement of interbody fusion, but offers the advantage of minimizing soft tissue collateral trauma. This key advantage allows the synergistic use of liposomal bupivacaine (20 mL total diluted 1:2 with plain bupivacaine 0.25% for 40 mL total, distributed evenly between all pedicle screw tracts) (Exparel, Pacira Pharmaceuticals) along the percutaneous access tracts to promote lasting non-opioid local analgesia for up to 72 hours. In combination, these techniques enable us to perform a highly effective and versatile TLIF with the patient comfortably under conscious sedation using propofol and ketamine infusion (18). In alignment with ERAS core concepts, this effectively eliminates the cardiopulmonary, gastrointestinal, endocrine, and electrolyte disturbances concomitant with general anesthesia, during both the intra- and post-operative periods. Keeping the patient awake during surgery also allows intraoperative neuromonitoring with direct patient feedback. This can reduce the risk of injuring exiting nerve root dorsal ganglion. To date, our published case series of 100 initial patients using this technique demonstrates significant improvement of patient reported clinical outcome scores at 1 year follow up with no intraoperative complications, average blood loss of 65 and 75 mL, and average operative times of 85 and 128 minutes for one and two level fusions, respectively, with an overall average length of stay of 1.4 days (19).
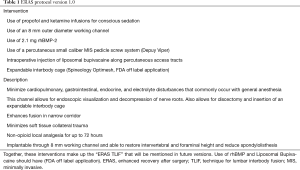
Full table
The successful ERAS TLIF became an important treatment option for our ERAS 2.0 protocol (Table 2), which is currently employed only for 1 to 3 level posterior lumbar fusions, both open and MIS. This second phase encompasses several nonsurgical ERAS components. These include pre-operative counseling by ERAS team members with an educational brochure and video about the concept and purpose of ERAS along with expectation management. More specifically, patients are advised on pre-operative nutritional optimization with increased protein and calorie intake and medical optimization of existing conditions (such as diabetes and hypertension) to weather the post-operative catabolic and insulin-resistant pathophysiologic state (1). Post-operative discharge destinations are explored, and inpatient rehab facilities are preselected. Endocrine and gastrointestinal optimization the day before surgery include a carbohydrate load as well as clear liquid diet or gentle bowel prep for insulin sensitization and avoidance of post-operative constipation and ileus, respectively. Our expectation of early post-operative bracing and mobilization with therapy services is communicated to the patient.

Full table
Peri-operative multimodal non-opioid analgesia is optimized with a 600 mg oral gabapentin load given in the pre-operative unit and an intravenous (IV) infusion of acetaminophen 1 g given immediately post-operatively. The combination of pre-operative health optimization and peri-operative multimodal analgesia has augmented the ability to utilize the endoscopic TLIF under conscious sedation via reductions in pathophysiologic disturbances typically encountered using general anesthesia. Thus, the surgeon is provided the enhanced direct patient feedback of pain generators intra-operatively without associated anesthetic concerns.
Post-operative ERAS rounds are carried out daily by team members to facilitate program compliance, help coordinate early mobilization, assess adequacy of analgesia, assist with acquisition of braces and walkers, and ensure timely hospital discharge (Figure 1).
Routine internal audits of quality derangements and data driven iterative refinement are critical to success of any ERAS protocol (Table 3). Four cases of the first 100 ERAS TLIF cases converted to general anesthesia. Of these four conversion cases, two were due to emesis, one was due to epistaxis, and the other was due to extreme anxiety. Given the aspiration risk secondary to emesis and epistaxis in the prone, semi-conscious, non-intubated patient, ondansetron, glycopyrrolate, and oxymetazoline nasal spray were added to the pre-operative anesthesia portion of the protocol. No further conversions due to emesis or epistaxis have since been noted. Intraoperative and post-operative pain control was inconsistent early on in the series. This was found to be secondary to injection of the liposomal bupivacaine into the soft tissue tract after instrumentation, and the solution does not diffuse readily without pressure. Once we began injecting the solution prior to creation of soft tissue tract and instrumentation, better delivery of anesthetic was achieved and post-operative analgesia was greatly improved. Two patients developed early infections in the interbody device within 2 months. A problem with central sterile processing of endoscopic equipment was audited and corrected. Vancomycin 1 g was also added to the endoscopic irrigation solution. Following these changes, no further infections have been noted. Two cases of early cage migration prompted more thorough end plate preparation evaluation with a radiopaque contrasted balloon expanded within the disc space under anteroposterior fluoroscopic visualization. If inadequate endplate preparation was discovered, further endoscopic discectomy was completed until bleeding endplate was directly visualized and properly prepared. No further cage migrations have been noted since the protocol was modified. Dissolution of the interbody cage was also noted early on, and in response the rhBMP sponge has since been implanted anterior to the cage rather than within the cage; the efficacy of this is still under investigation (5,19).

Full table
Implementation of our ERAS protocol into the practice of other spine surgeons within the department for 1 to 3 total level posterior lumbar fusions has shown statistically significant superiority in all metrics. Most notably, ERAS patients demonstrated decreases in-hospital length of stay, opioid consumption during the first 3 days after surgery, and an increase in distance ambulated with therapy services on all post-operative days when compared to pre-ERAS case matched controls (13). Given that the other participating surgeons do not perform the ERAS TLIF, this supports nonsurgical ERAS components as important contributors to enhanced recovery.
Based on favorable outcome measures of ERAS in decreased intraoperative surgical time, in-hospital morbidity, and hospital length of stay, cost comparison analysis between the ERAS TLIF and more traditional MIS TLIF was of obvious interest. Those patients in the MIS TLIF comparator cohort were also our senior author’s patients, and that procedure was performed using a more traditional unilateral opening and facetectomy. The same interbody cage and instrumentation are used, but the procedure was performed under general anesthesia, without liposomal bupivacaine, and without endoscopic decompression. Thirty-eight consecutive ERAS TLIF patients were compared to 15 medical comorbidity and body mass index (BMI) matched case controls. While both groups experienced equally excellent clinical outcomes by Oracle data integrator (ODI) change, the ERAS group incurred on average 68 vs. 231 mL of blood loss, length of stay 1.23 vs. 3.9 days, and a total cost savings of $3,444 (15.2%) per case ($4,330 when accounting for all readmissions and revisions between the two groups). Forty-four percent of this cost savings came from decreased operative suite time utilization. Thirty-two percent of overall savings represented decreased utilization of acute medical/intensive care unit (ICU) services for cardiopulmonary and other medical complications. The remaining 22% of the savings were achieved with shorter hospital stay (20).
Despite slow adoption in spine surgery, we have demonstrated the clinical and economic value of ERAS implementation within the field. Through the use of multimodal non-opioid peri-operative medications, long acting local anesthetic, and intraoperative conscious sedation, we have validated the feasibility of performing a versatile lumbar fusion procedure in an “ultra-MIS” fashion without compromising the surgical goal and obviating the need for general anesthesia and its attendant risks. Pre-operative psychological and physiological optimization and post-operative standardization of medications and therapy programs amplifies its benefits. With the ERAS program’s clinical outcome driven internal audit and continual iterative improvements, we are able to offer the patients the most optimal experience throughout their spine surgery journey.
ERAS in spine surgery has a demonstrable role in improving patient outcomes. Enhancing a patient’s recovery also concomitantly reduces resource expenditure, and in our evolving healthcare environment, presents a positive secondary effect and potential driver for more widespread adoption. Although our program has only been utilized in the inpatient setting, this protocol and its components can easily be translated to the outpatient setting. Further studies on ERAS implementation within inpatient and outpatient spine programs in the country are needed to support our findings and drive cost-effective innovation in peri-operative care.
Acknowledgments
None.
Footnote
Conflicts of Interest: MY Wang: Recipient of royalty payments from DePuy-Synthes Spine, Inc., Children’s Hospital of Los Angeles, Springer Publishing, and Quality Medical Publishing; consultant for DePuy-Synthes Spine, Inc., Stryker Spine, K2M, and Spineology; advisory board member for Vallum; stock in Spinicity and Innovative Surgical Devices; and Awardee of grants from the Department of Defense. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [Crossref] [PubMed]
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg 2002;183:630-41. [Crossref] [PubMed]
- Kahokehr A, Sammour T, Zargar-Shoshtari K, et al. Implementation of ERAS and how to overcome the barriers. Int J Surg 2009;7:16-9. [Crossref] [PubMed]
- Wainwright TW, Wang MY, Immins T, et al. Enhanced recovery after surgery (ERAS)—concepts, components, and application to spine surgery. Seminars in Spine Surgery 2018;30:104-10. [Crossref]
- Wang MY, Chang PY, Grossman J. Development of an Enhanced Recovery After Surgery (ERAS) approach for lumbar spinal fusion. J Neurosurg Spine 2017;26:411-8. [Crossref] [PubMed]
- Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: enhanced recovery after surgery (ERAS(®)) society recommendations. World J Surg 2013;37:259-84. [Crossref] [PubMed]
- Lassen K, Coolsen MM, Slim K, et al. Guidelines for perioperative care for pancreaticoduodenectomy: enhanced recovery after surgery (ERAS®) society recommendations. World J Surg 2013;37:240-58. [Crossref] [PubMed]
- Mortensen K, Nilsson M, Slim K, et al. Consensus guidelines for enhanced recovery after gastrectomy: enhanced recovery after surgery (ERAS®) society recommendations. Br J Surg 2014;101:1209-29. [Crossref] [PubMed]
- Soffin EM. YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth 2016;117:iii62-72. [Crossref] [PubMed]
- Soffin EM, Gibbons MM, Ko CY, et al. Evidence Review Conducted for the Agency for Healthcare Research and Quality Safety Program for Improving Surgical Care and Recovery: Focus on Anesthesiology for Total Hip Arthroplasty. Anesth Analg 2019;128:454-65. [Crossref] [PubMed]
- Soffin EM, Gibbons MM, Ko CY, et al. Evidence review conducted for the agency for healthcare research and quality safety program for improving surgical care and recovery: focus on anesthesiology for total knee arthroplasty. Anesth Analg 2019;128:441-53. [Crossref] [PubMed]
- Grosh T, Elkassabany NM. Enhanced recovery after shoulder arthroplasty. Anesthesiol Clin 2018;36:417-30. [Crossref] [PubMed]
- Brusko GD, Kolcun JPG, Heger JA, et al. Reductions in length of stay, narcotics use, and pain following implementation of an enhanced recovery after surgery program for 1- to 3-level lumbar fusion surgery. Neurosurg Focus 2019;46:E4. [Crossref] [PubMed]
- Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine (Phila Pa 1976) 1988;13:696-706. [Crossref] [PubMed]
- Peng CW, Yue WM, Poh SY, et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009;34:1385-9. [Crossref] [PubMed]
- Parker SL, Lerner J, McGirt MJ. Effect of minimally invasive technique on return to work and narcotic use following transforaminal lumbar inter-body fusion: a review. Prof Case Manag 2012;17:229-35. [Crossref] [PubMed]
- Wang MY, Cummock MD, Yu Y, et al. An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J Neurosurg Spine 2010;12:694-9. [Crossref] [PubMed]
- Wang MY, Grossman J. Endoscopic minimally invasive transforaminal interbody fusion without general anesthesia: initial clinical experience with 1-year follow-up. Neurosurg Focus 2016;40:E13. [Crossref] [PubMed]
- Kolcun JPG, Brusko GD, Basil GW, et al. Endoscopic transforaminal lumbar interbody fusion without general anesthesia: operative and clinical outcomes in 100 consecutive patients with a minimum 1-year follow-up. Neurosurg Focus 2019;46:E14. [Crossref] [PubMed]
- Wang MY, Chang HK, Grossman J. Reduced acute care costs with the ERAS® minimally invasive transforaminal lumbar interbody fusion compared with conventional minimally invasive transforaminal lumbar interbody fusion. Neurosurgery 2018;83:827-34. [Crossref] [PubMed]



