
Risk factors predicting less favorable outcomes in endoscopic lumbar discectomies
Introduction
Minimally invasive spine surgery has shown many benefits when compared to open techniques. Shorter hospital stay (1), less blood loss with less frequent need for transfusion has also been demonstrated (2). With less soft tissue destruction and creation of smaller dead spaces, fewer infections are seen (3-8). These procedures help preserve lumbar musculature (9,10). The health care system and society benefit from minimally invasive spine surgery. There are cost savings compared to open procedures (11,12). Faster time to narcotic independence and less narcotic utilization has been demonstrated (13-18). More rapid return to the workforce is also seen (19-22).
The advent of tubular access retractor systems for fusion and decompression have made minimally invasive procedures more commonly performed. These procedures have been demonstrated to provide comparable outcomes without increased morbidity when compared to open surgeries (2,21). Endoscopic lumbar discectomy has been shown to offer the same advantages seen with other tubular minimally invasive techniques. Other benefits of endoscopic surgery are the ability to perform these procedures under local anesthesia in an outpatient setting with a very low incidence of epidural fibrosis and scarring (23). Safety and efficacy of these techniques have been demonstrated over 40 years (24). Although favorable outcomes can be anticipated in approximately 80% of cases (25-31), certain risk factors may contribute to a suboptimal outcome. The purpose of this study is to evaluate risk factors to assess their correlation to poor results from endoscopic spine surgery.
Methods
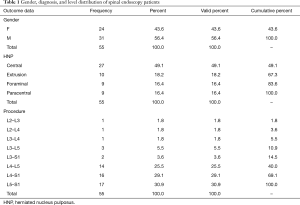
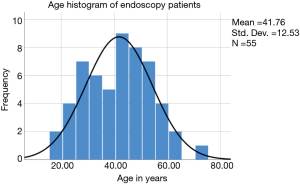
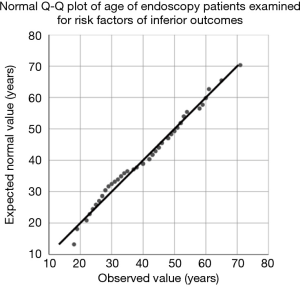
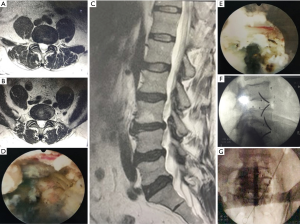
This is a retrospective analysis of 55 consecutive patients treated with endoscopic discectomy between June 2018 and March 2019 for symptomatic lumbar disc herniation refractory to conservative care. There were 31 males and 24 females with a normal age distribution (Table 1, Figures 1,2). Clinical assessment of herniated nucleus pulposus (HNP) was confirmed with magnetic resonance imaging (MRI). Outcome measures assessed included numeric rating of pre and postoperative visual analog score (VAS) for back and leg pain (32). Additionally, functional outcome was assessed using modified MacNab criteria (33) including return to work (RTW) and activities, with favorable result reaching preoperative work level. Time to narcotic independence was also evaluated. Restoring pre-injury work activity, reducing leg pain by 75% and back pain by 75%, with narcotic independence was required for excellent outcome. Patients were deemed to have a good outcome with a 50% reduction of back and leg pain, narcotic independence and return to preoperative or pre-injury occupation. Fair outcome patients had a less than 50% reduction of back and leg pain, and or work restrictions or need for narcotic medications. Patients unable to resume their preoperative or pre-injury employment activities were deemed to have at best a fair outcome irrespective of occupational work load. Patients requiring additional surgery at the index level were considered a failure of treatment. We tabulated the number of patients requiring injection therapy, but only assessed outcome after injections were completed. Several independent risk factors were studied and their effect on outcome was analyzed. These included obesity [body mass index (BMI) >30], tobacco use, psychiatric illness, extruded- or large lumbar disc herniations (greater than 10 mm), and facet arthropathy. Written informed consent was obtained from the patient for publication of this Original Study and any accompanying images.
Full table
Results
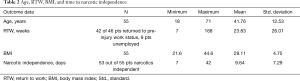
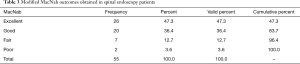
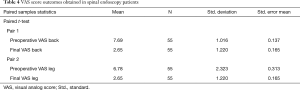
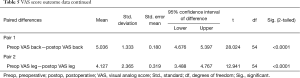
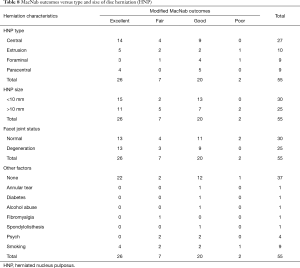
The patients’ mean age was 41.76±12.53 ranging from 18 to 71 years old (Table 2). Most of the herniations were contained herniations (49.1%) followed by extruded herniations (18.2%; Table 1). Follow-up was at least 6 months in duration and ranged from 6–18 months. The surgical levels are listed in Table 1, with most surgeries having been performed at the L5–S1 level (30.9%), followed by surgery at L4–S1 (29.1%) and L4–5 (25.5%). The mean RTW was 23.83±26.01 weeks. The average BMI was 29.11±4.75. Patients with a BMI of over 30 were considered obese. The average time for narcotic independence was 9.64±7.29 days (Table 2). MacNab outcomes showed that 47.3% (26/55) had excellent, 36.4% good (20/55), 12.7% fair (7/55), and 3.6% had poor (2/55), respectively (Table 3). The VAS scores for the back (7.69 to 2.65) and leg (6.78 to 2.65) pain reduced significantly (two-tailed paired t-test P<0.0001; Tables 4,5).
Full table
Full table
Full table
Full table
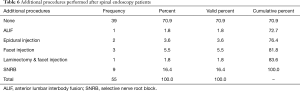
The endoscopic decompression procedure was successful in the majority of patients (83.6%; 46/55) and 39 of the 55 study patients did not require any additional treatment. Most additional aftercare consisted of injections: 9 selective nerve root blocks (SNRBs) for irritation of the dorsal root ganglion, two interlaminar epidural steroid injections, and four facet injections, one of which also underwent subsequent laminectomy. Ultimately, one patient underwent an anterior lumbar interbody fusion (ALIF) to control recurrent back and leg pain (Table 6). In his busy endoscopic spine practice, the author empirically identified several risk factors associated with the failure of the endoscopic transforaminal decompression procedure (Table 7). Smoking was associated with fair and poor MacNab outcomes at a statistically significant level (P=0.048). Preserved disc height greater than 10 mm, facet disease, obesity (BMI >30), diabetes, and alcohol abuse also were associated with less favorable clinical outcomes (Table 8). However, this associated did not reach statistical significance on chi-square testing. However, the four patients with a history of psychiatric disease had less favorable clinical outcomes at a statistically significant level (P=0.029).
Full table
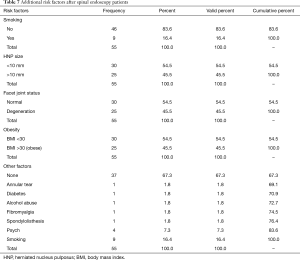
Full table
Full table
Four patients (7%) were unable to return to the pre-injury or preoperative work and activity level. Narcotic independence was not obtained in 2 patients (4%) at the 6-month follow-up, 45 patients (83%) were off narcotics within 1 week. Seven patients (13.0%) required several weeks of narcotic therapy.
Using a threshold of a herniation greater than 10 mm vs. smaller than 10 mm, we noted 22 patients (40.0%) had at least one herniated disc greater than 10 mm. The subset of patients with a large herniation had averaged postoperative VAS pain score of 3 for back pain and leg pain of 1.72. Massive herniations had more unsatisfactory results for back and leg pain. When isolating the 9 cases with extrusions (16.4%), postoperative back pain VAS scores averaged 3.1, again not as good as non-extruded discs. Leg pain relief was comparable to non-extrusion cases with a VAS score of 1. There were 8 cases with large extruded herniations (14.5%). These patients were among the most symptomatic preoperatively with VAS scores of 7.6 for back pain and 7 for leg pain. Postoperative back and leg pain again as were the case with smaller extrusion improved to VAS of 3 and 1 respectively. Massive herniations (larger than 10 mm) 16 cases (29.1%) without extrusion exhibited the worst preoperative pain with VAS scores of 7.8 for back pain and 7.6 for leg pain. Back pain lessened to 2.9 postoperatively. Leg pain score was 1.8, not quite as good as other herniations.
The 4 patients (7.3%) with a psychiatric history had suboptimal outcomes with back pain VAS of 3.8 and leg pain 2.8 in spite of comparable preoperative pain scores of 8 for back pain, and 8 for leg pain. The 9 patients (16.4%) who used tobacco regularly with preoperative VAS scores of 8.1 for back pain, and 7.4 for leg pain improved to level 1 pain for leg pain postoperatively but still had level 3.2 back pain. Considering obesity, 17 patients (30.9%) had a BMI over 30. Their preoperative back pain, VAS 7.6, and leg pain 6.8 improved to 2.7 for back pain, and 1.6 for leg pain. The two patients who abused alcohol did poorly. One had only 50% relief of back and leg pain, and the other required a fusion at the index level.
Isolated facet joint degeneration at an adjacent level or other levels was very prevalent in our series, 10 patients (18.2%). Preoperative VAS pain scores of 8 for back pain, 7 for leg pain improved to 2.5 for back pain, 1.2 for leg pain. Bulging discs at other levels were seen in 11 patients (20.0%). These patients had less postoperative pain than those with facet degeneration with VAS scores of 2 for back pain, and 0.3 for leg pain. Those patients with bulging discs and facet disease at adjacent levels with operative preoperative VAS scores of 7.3 for back pain and 5.7 for leg pain still had acceptable results with back pain of 2.3 and leg pain of 1.3. Patients having annular tears or herniations at adjacent levels without a concordant pain pattern did not have these levels treated surgically (Figure 3). These cases (11%) with preoperative back and leg scores of 8.2 and 8 respectively still had good outcomes with VAS scores of 2.7 for back pain, and 0.7 for leg pain. The two patients with instability (3.6%) continued to have axial pain, average VAS of 4. Leg pain however improved to 1.
Discussion
The high success rate for relief of radicular pain from lumbar disc herniation with microdiscectomy has arguably made this procedure the “gold standard”, for treating disc injury (34). Endoscopic discectomy results do compare favorably. There is an 85% improvement in leg radicular complaints after these procedures. Back pain improves as well by 65%. Return to gainful employment is among the most critical indicators of functional outcome. Our 93% success rate with this parameter is an exceptional outcome compared to traditional spinal decompression techniques.
Minimally invasive procedures lower the incidence of narcotic dependence. Only 3% of our patients were not off narcotics within 6 months of their procedure. Narcotic independence was achieved in 82% of cases within 1 week.
In spite of high success rates with endoscopic lumbar discectomy, there are risk factors that predict suboptimal pain relief. Large disc herniation has been shown to have a higher incidence of postoperative recurrence, and persistence of pain compared to small ones (20). This outcome is also seen after endoscopic discectomy. Relief of back pain is not as good with large herniations with postoperative VAS scores of 1.72 vs. 1. There was also slightly less relief of leg pain, VAS 3 vs. 2.7. Patients with a known psychiatric history did not have surgical outcomes as good as the control population. Improvement of radicular pain was only 3.8 points compared to 5.7 in patients without a psychiatric history. Back pain relief was also reduced compared to controls with a 3.8-point improvement versus 6.1-point improvement in the control group. Obesity compromises the results of leg pain relief with a VAS of 1.6 compared to 1 in the control group. Back pain relief was comparable to controls. Patients with instability, while having good relief of leg pain, had only a 50% relief of back pain. This was the most mediocre result for axial pain relief.
Other variables that were evaluated with a pre-study expectation of leading to poor outcomes were determined not to. While regular users of tobacco had higher preoperative back and leg pain, the postoperative score for leg pain of one was equal to controls. Relief of back pain was only 5% less with VAS of 3.2 rather than 2.7. Patients with adjacent level facet degeneration had comparable relief of low back pain and only slightly less relief of radiculopathy with VAS of 1.2 compared to 1. Annular tears or herniated discs at other levels not deemed to be primary pain generator and as such, left untreated did not produce adverse results; nor did bulging discs at adjacent levels. If bulges at adjacent levels were accompanied by facet degeneration back pain relief was comparable to controls but leg pain relief not as complete with VAS scores of 1.3 compared to 1. Extruded herniations, irrespective of size, once removed produced comparable outcomes for relief of back and leg pain.
When evaluating the 3% of patients with failed outcomes, requiring additional surgery at the index level, both had large herniations. One of the two cases used tobacco, abused alcohol, and had multilevel facet degeneration. The other had no comorbidities. Further study of the patients with fair results (7 cases) showed two patients had a psychiatric history and another abused alcohol. The others all had facet degeneration. One patient had instability and fibromyalgia.
The outcomes of this study support the efficacy of endoscopic discectomy for relief of radiculopathy and axial pain from symptomatic lumbar disc herniation. Relief of axial pain may not be complete, as other pain generators may be present, such as facet pathology. As is the case with other discectomy techniques, larger herniations do not fare as well as smaller ones. Large annular defects do not heal completely and remain visible on subsequent MRI. Patients with a known psychiatric history should be counseled preoperatively that complete pain relief may be an unrealistic expectation. These patients are less likely to rejoin the workforce.
This retrospective study has limitations. The sample size is small, precluding it from sophisticated statistical analysis because of lack of power. Preoperative images were performed at different institutions, and their respective reports were of variable quality. Lastly, our follow up for these cases is only 6–18 months. At least in part, some of these limitations are a result of societal pressure. Patients seeking an endoscopic, minimally invasive solution to intractable pain will not allow randomization to an open procedure. Often even in the presence of instability, authorization for fusion might not be forthcoming. Many patients with instability will prefer an attempt at pain relief with discectomy because of the stigma associated with spinal fusion, and its potential failure and a long convalescence. The concepts presented herein should be validated on a larger patient sample.
Conclusions
Endoscopic discectomy safely and reliably reduces axial pain and radiculopathy from lumbar disc herniation. Risk factors predictive of less favorable outcomes include advanced degenerative changes of the intervertebral disc and the facet joint complex, large herniations, psychiatric history, obesity, instability, and tobacco use. The presence of persistent axial pain in patients with instability suggests a need for additional study for techniques to lessen this symptom. The merits of adding fusion to the endoscopic spine surgery needs to be evaluated further to see if this can help this subset of patients. We typically advise them that fusion surgery may be required for more reliable pain relief. Follow up diagnostic work-up for vertical instability may be demonstrated by progressive disc space collapse. The risk factors shown to contribute to poor outcomes, at a minimum, need to generate discussion with patients preoperatively to advise them that incomplete pain relief is a possibility as is the need for additional surgery. Follow-up studies with larger patient numbers will need to validate the concepts presented herein with statistical power.
Acknowledgments
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. IRB approval was obtained for this study (CEIFUS 106-19). Written informed consent was obtained from the patient for publication of this Original Study and any accompanying images.
References
- Skovrlj B, Gilligan J, Cutler HS, et al. Minimally invasive procedures on the lumbar spine. World J Clin Cases 2015;3:1-9. [Crossref] [PubMed]
- Patel AA, Zfass-Mendez M, Lebwohl NH, et al. Minimally invasive versus open lumbar fusion: a comparison of blood loss, surgical complications, and hospital course. Iowa Orthop J 2015;35:130-4. [PubMed]
- Smith JS, Shaffrey CI, Sansur CA, et al. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2011;36:556-63. [Crossref] [PubMed]
- Rosen DS, O'Toole JE, Eichholz KM, et al. Minimally invasive lumbar spinal decompression in the elderly: outcomes of 50 patients aged 75 years and older. Neurosurgery 2007;60:503-9; discussion 509-10. [Crossref] [PubMed]
- O'Toole JE, Eichholz KM, Fessler RG. Surgical site infection rates after minimally invasive spinal surgery. J Neurosurg Spine 2009;11:471-6. [Crossref] [PubMed]
- O'Toole JE, Eichholz KM, Fessler RG. Minimally invasive far lateral microendoscopic discectomy for extraforaminal disc herniation at the lumbosacral junction: cadaveric dissection and technical case report. Spine J 2007;7:414-21. [Crossref] [PubMed]
- O'Toole JE, Eichholz KM, Fessler RG. Minimally invasive approaches to vertebral column and spinal cord tumors. Neurosurg Clin N Am 2006;17:491-506. [Crossref] [PubMed]
- Fessler RG, O'Toole JE, Eichholz KM, et al. The development of minimally invasive spine surgery. Neurosurg Clin N Am 2006;17:401-9. [Crossref] [PubMed]
- Pishnamaz M, Schemmann U, Herren C, et al. Muscular changes after minimally invasive versus open spinal stabilization of thoracolumbar fractures: a literature review. J Musculoskelet Neuronal Interact 2018;18:62-70. [PubMed]
- Kim CW. Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Spine (Phila Pa 1976) 2010;35:S281-6. [Crossref] [PubMed]
- Hofstetter CP, Hofer AS, Wang MY. Economic impact of minimally invasive lumbar surgery. World J Orthop 2015;6:190-201. [Crossref] [PubMed]
- Al-Khouja LT, Baron EM, Johnson JP, et al. Cost-effectiveness analysis in minimally invasive spine surgery. Neurosurg Focus 2014;36:E4. [Crossref] [PubMed]
- Savarese JJ, Tabler NG Jr. Multimodal analgesia as an alternative to the risks of opioid monotherapy in surgical pain management. J Healthc Risk Manag 2017;37:24-30. [Crossref] [PubMed]
- Brubaker L, Kendall L, Reina E. Multimodal analgesia: a systematic review of local NSAIDs for non-ophthalmologic postoperative pain management. Int J Surg 2016;32:158-66. [Crossref] [PubMed]
- Singhal NR, Jones J, Semenova J, et al. Multimodal anesthesia with the addition of methadone is superior to epidural analgesia: a retrospective comparison of intraoperative anesthetic techniques and pain management for 124 pediatric patients undergoing the Nuss procedure. J Pediatr Surg 2016;51:612-6. [Crossref] [PubMed]
- de Leon-Casasola OA. Multimodal approaches to the management of neuropathic pain: the role of topical analgesia. J Pain Symptom Manage 2007;33:356-64. [Crossref] [PubMed]
- Nicholson T, Maltenfort M, Getz C, et al. Multimodal pain management protocol versus patient controlled narcotic analgesia for postoperative pain control after shoulder arthroplasty. Arch Bone Jt Surg 2018;6:196-202. [PubMed]
- Skovrlj B, Belton P, Zarzour H, et al. Perioperative outcomes in minimally invasive lumbar spine surgery: a systematic review. World J Orthop 2015;6:996-1005. [Crossref] [PubMed]
- Goldstein CL, Phillips FM, Rampersaud YR. Comparative effectiveness and economic evaluations of open versus minimally invasive posterior or transforaminal lumbar interbody fusion: a systematic review. Spine (Phila Pa 1976) 2016;41 Suppl 8:S74-89. [PubMed]
- Adogwa O, Parker SL, Bydon A, et al. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech 2011;24:479-84. [PubMed]
- Parker SL, Mendenhall SK, Shau DN, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg 2014;82:230-8. [Crossref] [PubMed]
- Wang X, Borgman B, Vertuani S, et al. A systematic literature review of time to return to work and narcotic use after lumbar spinal fusion using minimal invasive and open surgery techniques. BMC Health Serv Res 2017;17:446. [Crossref] [PubMed]
- Choi G, Pophale CS, Patel B, et al. Endoscopic Spine Surgery. J Korean Neurosurg Soc 2017;60:485-97. [Crossref] [PubMed]
- Hammer M. Safety of spinal endoscopy is contingent on basic image interpretation. Reg Anesth Pain Med 2002;27:621; author reply 621-2. [Crossref] [PubMed]
- Tsou PM, Alan Yeung C, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J 2004;4:564-73. [Crossref] [PubMed]
- Tsou PM, Yeung AT. Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: outcome and technique. Spine J 2002;2:41-8. [Crossref] [PubMed]
- Yeung A, Kotheeranurak V. Transforaminal endoscopic decompression of the lumbar spine for stable isthmic spondylolisthesis as the least invasive surgical treatment using the YESS surgery technique. Int J Spine Surg 2018;12:408-14. [Crossref] [PubMed]
- Yeung AT, Gore S. In-vivo endoscopic visualization of patho-anatomy in symptomatic degenerative conditions of the lumbar spine II: intradiscal, foraminal, and central canal decompression. Surg Technol Int 2011;21:299-319. [PubMed]
- Yeung AT, Yeung CA. Advances in endoscopic disc and spine surgery: foraminal approach. Surg Technol Int 2003;11:255-63. [PubMed]
- Yeung AT, Yeung CA. In-vivo endoscopic visualization of patho-anatomy in painful degenerative conditions of the lumbar spine. Surg Technol Int 2006;15:243-56. [PubMed]
- Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am 2007;38:363-72. abstract vi. [Crossref] [PubMed]
- Erçalık T, Gencer Atalay K, Şanal Toprak C, et al. Outcome measurement in patients with low back pain undergoing epidural steroid injection. Turk J Phys Med Rehabil 2019;65:154-9. [Crossref] [PubMed]
- Macnab I. The surgery of lumbar disc degeneration. Surg Annu 1976;8:447-80. [PubMed]
- Parker SL, Mendenhall SK, Godil SS, et al. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res 2015;473:1988-99. [Crossref] [PubMed]


