
Full-endoscopic spine surgery for radiculopathy after osteoporotic vertebral compression fractures: a case report
Introduction
Percutaneous vertebroplasty (PVP) and balloon kyphoplasty (BKP) are minimally invasive operative procedures for the treatment of osteoporotic vertebral compression fractures (OVCFs). As the population in Japan is aging rapidly, BKP has become one of the most popular and widely used operative procedures. BKP is effective for back and radicular pain (1). Polymethylmethacrylate (PMMA) leakage, the most frequent complication, can occur into paravertebral soft tissue, veins, the intervertebral disc space, or the spinal canal (epidural space or vertebral foramen) (2,3). Subsequently, leakage to the vertebral foramen can cause newly developing radiculopathy (4). Even after conservative therapy for OVCFs (bed rest at the acute phase, medication, and external fixation by a corset), delated onset of radiculopathy is observed in some cases due to advanced vertebral collapse. Interbody fusion surgery is a reasonable treatment for vertebral fracture, but such surgery is invasive for elderly patients and the complications are not rare. As OVCFs occur based on osteoporosis, subsequent adjacent vertebral fractures frequently occur even at screwed vertebrae.
In contrast, the recently developed full-endoscopic spine surgery (FESS) is one of the most sophisticated operative procedures for the treatment of lumbar disc herniation (LDH). FESS can be used to treat LDH (5,6) as well as foraminal stenosis using a high-speed drill (7). We have used FESS to treat radiculopathy after OVCFs. In this case report, we summarize our experience and demonstrate the technical FESS-related tips for the treatment of radiculopathy after OVCFs.
Case presentation
Between October 2018 and April 2019, three consecutive patients with radiculopathy after OVCFs underwent FESS with a 7-mm diameter spinal full-endoscopic system (Richard Wolf GmbH, Knittlingen, Germany). All patients had severe unilateral radiculopathy that was resistant to medical treatment, epidural steroid injection, and/or nerve block. To focus on foraminal stenosis after OVCFs, we excluded a patient who received FESS for lateral recesses stenosis after OVCFs.
For all patients, FESS was conducted at only one vertebral level by a single surgeon (Hisashi Koga). Neurological examination, electrophysiological examination, and preoperative magnetic resonance imaging (MRI) and computed tomography (CT) were used to diagnose foraminal stenosis after OVCFs. Each patient’s leg pain was evaluated using the numerical rating scale (NRS) score.
Surgical technique
The patients were carefully log-rolled into a prone position. The surgery was performed under general anesthesia and simultaneous motor-evoked potential monitoring. During the operation, a fluoroscope was placed across the center of the operating table to ensure appropriate positioning. Eight-millimeter ipsilateral skin and fascial incisions were made on the corresponding vertebral level 6–7 cm lateral from midline. The basic operative procedures for LDH [full-endoscopic discectomy (FED)-transforaminal approach (TFA)] (8) and for foraminoplasty [(FED-posterolateral approach (PLA)] (5) were performed as described previously.
Three female patients were registered in this study. The mean patient age was 81.7 years (range, 80–83 years), significantly higher than that of our previous case series of FESS (5-8). BKP was previously performed on one patient in another hospital. The average period between onset of OVCFs and FESS was 8 months (range, 7–9 months) (Table 1).

Full table
The detailed disease states are described in Table 1; the operative findings revealed that all patients had foraminal stenosis and LDH. The presence of extraforaminal stenosis was also suspected by impingement of osteophytes on the nerve root; thus, removal of the osteophytes along a vertebral endplate was also performed in all cases (Figure 1). The mean operative time was 60.7 min (range, 53–72 min); the mean blood loss was negligible in all patients. We observed no operative complications, and all patients were discharged from the hospital the day after the FESS. Immediately after the FESS, leg pain stemming from radiculopathy after OVCFs improved in all cases. The NRS scores improved in all cases from a mean of 9 to a mean of 2.3 (Table 1).
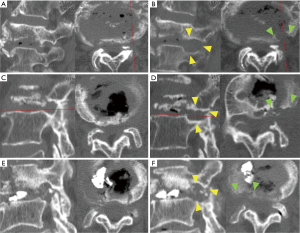
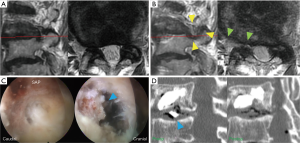
The MRI and intraoperative endoscopy findings of a representative case (No. 3) are shown in Figure 2. This 83-year-old woman presented with lower back pain and right leg pain (L3 dermatomes) that started 7 months after L3 OVCF. Despite undergoing BKP in another hospital, her pain did not improve. She visited our outpatient clinic in a wheelchair. A neurological examination revealed a positive straight leg raise on the right side (40+/80) and moderate muscle weakness (iliopsoas muscle: 3/5; quadriceps muscle: 4/5). Lumbar MRI revealed L3 OVCF and foraminal stenosis of the right L3 nerve root (Figure 2A). In addition to decreasing foraminal length and width due to OVCF (Figure 1E), CT demonstrated PMMA leakage into the intervertebral disc space (Figure 2D, left, blue arrowhead). During the operation, the superior article process was removed first, followed by the osteophyte and extruded disc material (Figure 2C). Immediately postoperative, the patient’s leg pain improved and the leaked PMMA disappeared (Figure 2D, right). At 2 months postoperative, the patient’s muscle weakness had also improved, allowing her to walk with a cane. Postoperative MRI (Figure 2B) and CT (Figure 1F) images revealed enlargement of the intervertebral foramen.
Discussion
The frequency of OVCFs is increasing as the elderly population grows. Although the major symptom of OVCFs is back pain, neurological symptoms such as myelopathy, cauda equina syndrome, and radiculopathy also occur. The incidence of radiculopathy with severe pain is not rare. Sasaki et al. observed severe pain in 10 of 66 OVCF patients (15.2%), while Kim et al. reported a 25% (15/59) rate (1,9). It was also reported that OVCFs at the lower lumbar spine occasionally induce radiculopathy (10).
Myelopathy and cauda equina syndrome combined with bladder and rectal disturbances require rapid surgical treatment, whereas radiculopathy after OVCFs without severe motor dysfunction is frequently treated conservatively. Prolonged radiculopathy must be treated surgically; however, posterior decompression may be insufficient and additional intervertebral fusion is frequently required. Interbody fusion surgery is effective for radiculopathy after OVCFs but is invasive and high-risk for elderly patients with osteoporosis. The advent of a less invasive surgical treatment would allow surgical intervention at the early stage of radiculopathy. PVP and BKP have the potential to be such treatments, but they may also cause radiculopathy via PMMA leakage (4).
Enlargement of collapsed vertebral foramen (foraminoplasty) is the core principle of FESS treatment. Lumbar disc degeneration is correlated with OVCFs (11), as evidenced by LDH in all cases. FESS seems to be an appropriate strategy in terms of the possibility of discectomy. The participation of osteophytes for radiculopathy after OVCFs was previously reported by Kim et al. (1). In this report, radiculopathy was significantly observed in inferior-type fractures, in that the fracture line was located along the caudal endplate of the collapsed vertebral body. The mechanism was as follows: bony fragments (= osteophytes) from the collapsed body invade the foraminal space, directly compressing the root. Therefore, osteophyte removal seems to also be a reasonable treatment for radiculopathy after OVCFs. The combination of FESS and a high-speed drill could show good performance in such situations.
Few studies have reported the use of the FESS technique for treatment of radiculopathy after OVCFs. Wagner et al. reported a case of a 72-year-old woman who presented with L2 radiculopathy after a kyphoplasty procedure. CT imaging showed leakage of the kyphoplasty cement into the vertebral foramen; the TFA was used to remove it and decompress the L2 nerve (12). Şenturk et al. reported the case of a 44-year-old woman who presented with L4 radiculopathy after a kyphoplasty procedure and was treated using a translaminar approach (13). The advantage of FESS for removing osteophytes has been also reported. Telfeian et al. treated a patient with L4 radiculopathy caused by osteophytes at the right L4/5 vertebral foramen using a combination of the TFA and high-speed drill (14). Although we presented only three cases of radiculopathy after OVCFs treated by FESS and could find few studies like ours, the FESS technique is a potential alternative treatment for radiculopathy after OVCFs.
“Take-away” lesson
The preliminary results obtained from only three patients show that FESS is feasible for the treatment of radiculopathy after OVCFs. The combination of foraminoplasty, discectomy, and osteophyte removal is a key in the FESS technique.
Acknowledgments
We thank the operating room staff for their technical assistance and the medical records clerks who helped to collect the patient data. We also thank the radiological department staff for recording the CT and MRI data.
Funding: This work was partly supported by a grant from the Iwai Medical Foundation.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Hisashi Koga and Alf Giese) for the series “Full-endoscopic Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss.2019.10.11). The series “Full-endoscopic Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. HK served as the unpaid Guest Editor of the series and serves as an unpaid editorial member of Journal of Spine Surgery from October 2018 to October 2020. The other authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patients for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim DE, Kim HS, Kim SW, et al. Clinical analysis of acute radiculopathy after osteoporotic lumbar compression fracture. J Korean Neurosurg Soc 2015;57:32-5. [Crossref] [PubMed]
- Zhan Y, Jiang J, Liao H, et al. Risk Factors for Cement Leakage After Vertebroplasty or Kyphoplasty: A Meta-Analysis of Published Evidence. World Neurosurg 2017;101:633-42. [Crossref] [PubMed]
- Xiao H, Yang J, Feng X, et al. Comparing complications of vertebroplasty and kyphoplasty for treating osteoporotic vertebral compression fractures: a meta-analysis of the randomized and non-randomized controlled studies. Eur J Orthop Surg Traumatol 2015;25:77-85. [Crossref] [PubMed]
- Wu CC, Lin MH, Yang SH, et al. Surgical removal of extravasated epidural and neuroforaminal polymethylmethacrylate after percutaneous vertebroplasty in the thoracic spine. Eur Spine J 2007;16 Suppl 3:326-31. [Crossref] [PubMed]
- Fujita M, Kawano H, Kitagawa T, et al. Preoperative Design for the Posterolateral Approach in Full-Endoscopic Spine Surgery for the Treatment of L5/S1 Lumbar Disc Herniation. Neurospine 2019;16:105-12. [Crossref] [PubMed]
- Tonosu J, Oshima Y, Shiboi R, et al. Consideration of proper operative route for interlaminar approach for percutaneous endoscopic lumbar discectomy. J Spine Surg 2016;2:281-8. [Crossref] [PubMed]
- Ishibashi K, Oshima Y, Inoue H, et al. A less invasive surgery using a full-endoscopic system for L5 nerve root compression caused by lumbar foraminal stenosis. J Spine Surg 2018;4:594-601. [Crossref] [PubMed]
- Yokosuka J, Oshima Y, Kaneko T, et al. Advantages and disadvantages of posterolateral approach for percutaneous endoscopic lumbar discectomy. J Spine Surg 2016;2:158-66. [Crossref] [PubMed]
- Sasaki M, Aoki M, Nishioka K, et al. Radiculopathy caused by osteoporotic vertebral fractures in the lumbar spine. Neurol Med Chir (Tokyo) 2011;51:484-9. [Crossref] [PubMed]
- Chung SK, Lee SH, Kim DY, et al. Treatment of lower lumbar radiculopathy caused by osteoporotic compression fracture: the role of vertebroplasty. J Spinal Disord Tech 2002;15:461-8. [Crossref] [PubMed]
- Castaño-Betancourt MC, Oei L, Rivadeneira F, et al. Association of lumbar disc degeneration with osteoporotic fractures; the Rotterdam study and meta-analysis from systematic review. Bone 2013;57:284-9. [Crossref] [PubMed]
- Wagner R, Telfeian AE, Iprenburg M, et al. Transforaminal Endoscopic Solution to a Kyphoplasty Complication: Technical Note. World Neurosurg 2016;91:195-8. [Crossref] [PubMed]
- Şenturk S, Akyoldas G, Ünsal ÜÜ, et al. Minimally Invasive Translaminar Endoscopic Approach to Percutaneous Vertebroplasty Cement Leakage: Technical Note. World Neurosurg 2018;117:15-9. [Crossref] [PubMed]
- Telfeian AE. An awake, minimally-invasive, fully-endoscopic surgical technique for treating lumbar radiculopathy secondary to heterotopic foraminal bone formation after a minimally invasive transforaminal lumbar interbody fusion with BMP: technical note. J Spine Surg 2018;4:162-6. [Crossref] [PubMed]


