A protective method to reduce radiation exposure to the surgeon during endoscopic lumbar spine surgery
Introduction
Endoscopic lumbar spine surgery is a minimally invasive surgery (MIS) that is less invasive than conventional open lumbar spine surgery (1,2). This surgery has emerged through refinement of surgical techniques, detailed understanding of local anatomy, and development of surgical instruments. However, MIS uses intraoperative fluoroscopy, which causes higher ionizing radiation exposure to the surgeon during endoscopic lumbar spine surgery compared to open surgery (3). This exposure is much less than that in occupational guidelines of the National Council on Radiation Protection & Measurements, but the surgeon must be protected against radiation as much as possible, based on the linear no-threshold risk model (4). In this model, the stochastic effect of radiation exposure, which is different from the deterministic effect, has no threshold and the risk of death increases with radiation dosage.
To reduce the risk of radiation-induced morbidities among surgeons, we developed a new protective method to reduce radiation exposure during endoscopic lumbar spine surgery. The hypothesis in this study is that radiation exposure to the surgeon using the new method will be much less than that using the conventional method.
Methods
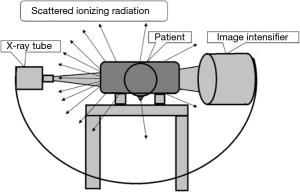
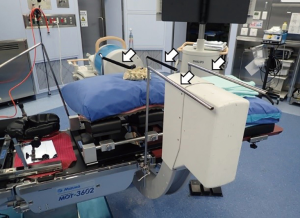
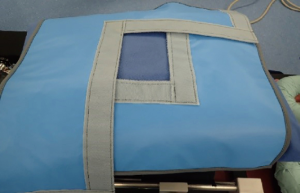
In using fluoroscopy during spine surgery, surgeons and other persons in the operating room are exposed to scattered ionizing radiation from the patient’s body (Figure 1). The core concept of the protective method used in this study is to separate two spaces using a lead protector: one space contains the patient, operation table, X-ray tube and image intensifier, and the other space is the rest of the operation room. This separation allows the operator to perform the operative procedure through a hole in the lead radiation protector with little radiation exposure. Less scattered X-rays may reach the surgeon by covering the patient with a specially designed lead radiation protector and setting up a special frame to sheet the X-ray tube and image intensifier with a lead radiation protector between the fluoroscope and the operating table (Figures 2,3). These lead radiation protectors were not anchored to the patients, but just placed on the patients. The frame was made of iron and set up not to interfere directly with the beam from the X-ray tube (Figure 4). This frame is patent pending (Application No./Patent No.15843463.9-1666 PCT/JP2015/004772). We named the radiation protection method, which includes the frame, as the Separation between Two Spaces (STS) method. The STS method is non-sterile; however, since the entire STS is completely covered with surgical sterile sheets, the surgical field is guaranteed to be aseptic.
We performed a prospective interventional study to determine the effectiveness of the new radiation protection method during endoscopic lumbar spine surgery. The primary outcome was radiation exposure to the surgeon [Sievert (Sv)] per case, while the intervention was use of the new method or the conventional method during surgery. After approval by the Institutional Review Board at our institution (Number of the Ethic Approval 20140213-1), 18 adult patients scheduled for single or two level endoscopic lumbar spine surgery, including microendoscopic discectomy (MED) and microendoscopic laminectomy (MEL), were enrolled in the study. This was a prospective study and all surgeries were performed by one doctor between March 2014 and August 2015. The inclusion criterion was patients aged >18. The exclusion criterion was a history of previous surgery at the same level and side. Of the 18 patients, 9 each underwent surgery with the new method and the conventional method randomly at the discretion of the doctor.
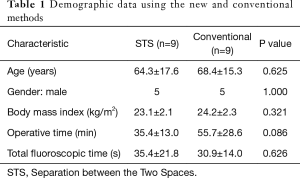
Demographic data for patient age, gender, and body mass index (BMI) were collected, and the surgical time and total fluoroscopy time in each surgery were recorded. The patients treated with the new method were 5 males and 4 females of average age 64.3±17.6 years, and those treated with the conventional method were five males and four females of average age 68.4±15.3 years. The average BMIs in STS group was 23.1±2.1 kg/m2 and those in conventional group was 24.2±2.3 kg/m2, the operative times were 35.4±13.0 and 55.7±28.6 min, and the total fluoroscopy times were 35.4±21.8 and 30.9±14.0 s, respectively. The small differences in background between the two groups are unlikely to influence the radiation exposure results (Table 1). The surgeon always stood at the X-ray tube side but not at the image intensifier side in all 18 cases.
Full table
Exposure of the surgeon to radiation was measured using three radiation badges (MYDOSE mini x, Hitachi, Japan) placed outside the lead apron and thyroid shield of the surgeon (Figure 5) at the levels of the neck, chest, and abdomen. These badges displayed radiation exposure instantly and the value was recorded when the surgery was completed.

MED and MEL were typically performed as described previously (5,6). The patient was placed on a radiolucent operating table. The fluoroscope (BV Endura, Philips, The Netherland), which is a single plane image intensifier, was used to confirm the surgical level and site in the lateral view during surgery. It was positioned in advance by a radiation technologist and was not moved during surgery. X-rays were beamed in the lateral direction of the patient from the side where the surgeon stood to the opposite side.
An independent statistician performed statistical analysis using SPSS (SPSS, Inc.). An unpaired Student t-test was used to compare differences between the two groups for demographic data, except for gender and surgical side, which were evaluated by Fisher exact test. A significant difference was accepted at P<0.05.
Results
Radiation exposures to the surgeon with STS and conventional methods are shown in Table 2. The average radiation exposures to the neck, chest, and abdomen were 1.0, 0.8 and 0.7 µSv, respectively, with STS, and 3.2, 10.8, and 10.2 µSv, respectively, with the conventional method. The effective doses (HEE) calculated by the formula, HEE =0.08Ha + 0.44Hb + 0.45Hc + 0.03Hm (Ha: neck, Hb: chest, Hc: abdominal, Hm: maximum value among the former 3 values) with STS and conventional methods were 0.8 and 10.0 µSv, respectively (Table 3) (7). The differences in radiation exposure at the neck, chest, and abdomen, and that in HEE between the two groups were all significant (P=0.013, P<0.001, P<0.001, P<0.001, respectively).
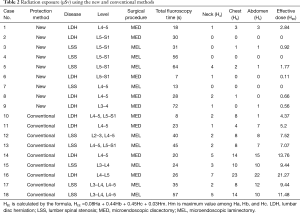
Full table
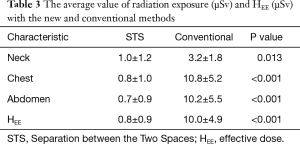
Full table
Exposure of the surgeon to radiation using the conventional method was far lower than the limit of 20,000 µSv in the 1990 International Commission on Radiological Protection (ICRP) guidelines (7). This value is equivalent to 2,000 endoscopic surgeries using the conventional method in 1 year. However, STS reduced the exposure effective dose equivalent to approximately 8% of that with the conventional method.
Discussion
Minimally invasive (MI) endoscopic spine surgery was established in the 1990’s and has developed through improvements in technology and procedures. This surgery has advantages of reductions in surgical time, bleeding, postoperative pain medication, hospital stay, and return-to-work time, and has good outcomes compared to conventional open spine surgery (6,8-12). However, exposure of the surgeon to radiation during MI endoscopic spine surgery is greater than that during open surgery since ionizing radiation is generally used during MI endoscopic spine surgery to localize the surgical site. In MI lumbar microdiscectomy, Mariscalco et al. found that the surgeon is more exposed to radiation than in open microdiscectomy (13).
Ionizing radiation causes hazards to human health, including radiation-induced complications such as cataract, skin erythema, thyroid cancer, and other cancers (4). In procedures that use X-rays during surgery, surgeons should recognize the risk and try to reduce exposure of radiation for all operating room staff. A lead apron and lead collar can reduce exposure to radiation by 96.9% and 94.2%, respectively, compared to their non-use (14), and facing 90 degrees from the operating table during use of X-rays reduces radiation exposure to the surgeon’s eyes (3). A surgeon positioned on the X-ray tube side is exposed to more scatter radiation from the patient, compared to the image intensifier side (3) (Figure 1). Therefore, the surgeon should not stand on the X-ray tube side, if possible. However, the positioning of the surgeon in this study was on the tube side, and this may have caused greater radiation exposure. The X-ray tube should be placed as close to the patient as possible because this reduces scatter radiation (3). One-shot radiation causes less exposure than continuous radiation (3), and surgeons should be aware of the location of the fluoroscope.
STS reduced the radiation exposure to 8% of the conventional exposure in this study. This method shields scattering radiation reflected on or passing through or near the patient so that the surgeon and all persons in the operation room have reduced radiation exposure. This is important because the surgeon is not entirely shielded by a lead apron or lead collar. Moreover, STS is available for full endoscopic lumber discectomy (FELD) or percutaneous pedicle screw fixation (PPSF) because of the unique design.
The lead radiation protector in STS should not be placed in the X-ray field during surgery since this might increase X-ray beams due to the fluoroscopy automatic exposure control mode, which can then increase the scattered ionizing radiation. The limitations of this study are the small number of cases and selection bias due to non-random design. A further study in more cases and with randomized controls is required to validate the results. The primary surgeon, Hirohiko Inanami has a patent for this system. However, possession of patents has no influence on the scientific nature of this study.
In this study, radiation exposure at the hand was not measured. Funao et al. measured the radiation dose to the unshielded finger, thyroid, chest, and genitals in minimally invasive transforaminal lumber interbody fusion (MIS-TLIF), and found that the finger was significantly more exposed than the other body regions (15). Although STS reduces exposure of scattered ionizing radiation, the finger might be exposed to direct ionizing radiation. Hence, care should be taken to avoid direct radiation exposure of the surgeon’s finger.
We did not measure the radiation exposure of the patients. However, scattered X-rays reflected on the lead shield should be unlikely to increase patient exposure, because X-ray shielding by lead is mainly done by converting that energy into thermal energy.
In conclusion, STS developed to reduce exposure of the surgeon to ionizing radiation during MI endoscopic lumbar spine surgery was significantly more effective than the conventional approach. The protective method reduced the effective dose equivalent to approximately 8% of that with the conventional method.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Institutional Review Board approval (No. 20140213-1) and necessary patient consents were obtained for this study.
References
- Phan K, Mobbs RJ. Minimally Invasive Versus Open Laminectomy for Lumbar Stenosis: A Systematic Review and Meta-Analysis. Spine (Phila Pa 1976) 2016;41:E91-100. [Crossref] [PubMed]
- Rasouli MR, Rahimi-Movaghar V, Shokraneh F, et al. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev 2014.CD010328. [PubMed]
- Srinivasan D, Than KD, Wang AC, et al. Radiation safety and spine surgery: systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg 2014;82:1337-43. [Crossref] [PubMed]
- Hamada N, Fujimichi Y. Classification of radiation effects for dose limitation purposes: history, current situation and future prospects. J Radiat Res 2014;55:629-40. [Crossref] [PubMed]
- Mayer HM, Brock M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg 1993;78:216-25. [Crossref] [PubMed]
- Pao JL, Chen WC, Chen PQ. Clinical outcomes of microendoscopic decompressive laminotomy for degenerative lumbar spinal stenosis. Eur Spine J 2009;18:672-8. [Crossref] [PubMed]
- 1990 Recommendations of the International Commission on Radiological Protection. ICRP Publication 60. Ann. ICRP 21 (1-3), 1991, Superseded by ICRP Publication 103.
- Mayer HM. Spine update. Percutaneous lumbar disc surgery. Spine (Phila Pa 1976) 1994;19:2719-23. [Crossref] [PubMed]
- Kambin P, Zhou L. Arthroscopic discectomy of the lumbar spine. Clin Orthop Relat Res 1997.49-57. [Crossref] [PubMed]
- Brayda-Bruno M, Cinnella P. Posterior endoscopic discectomy (and other procedures). Eur Spine J 2000;9 Suppl 1:S24-9. [Crossref] [PubMed]
- Wu X, Zhuang S, Mao Z, et al. Microendoscopic discectomy for lumbar disc herniation: surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976) 2006;31:2689-94. [Crossref] [PubMed]
- Minamide A, Yoshida M, Yamada H, et al. Endoscope-assisted spinal decompression surgery for lumbar spinal stenosis. J Neurosurg Spine 2013;19:664-71. [Crossref] [PubMed]
- Mariscalco MW, Yamashita T, Steinmetz MP, et al. Radiation exposure to the surgeon during open lumbar microdiscectomy and minimally invasive microdiscectomy: a prospective, controlled trial. Spine (Phila Pa 1976) 2011;36:255-60. [Crossref] [PubMed]
- Ahn Y, Kim CH, Lee JH, et al. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine (Phila Pa 1976) 2013;38:617-25. [Crossref] [PubMed]
- Funao H, Ishii K, Momoshima S, et al. Surgeons' exposure to radiation in single- and multi-level minimally invasive transforaminal lumbar interbody fusion; a prospective study. PLoS One 2014;9:e95233. [Crossref] [PubMed]