
Priapism associated with lumbar stenosis: case report and literature review
Introduction
Lumbar spinal stenosis (LSS) is characterized by narrowing of the central canal, lateral recesses, or associated neural foramina (1). Unlike its more common degenerative counterpart, primary LSS is congenital in origin with short pedicles predisposing patients to central canal narrowing (2,3). As a result, patients with primary LSS have an onset of symptoms at an early age and present without degenerative changes. Acquired LSS is the most common etiological form and is the direct result of spondylotic changes such as disc degeneration, disc herniation, facet osteophyte formation, and ligamentous hypertrophy (4). Less common etiological forms of LSS include iatrogenic, post-traumatic, or secondary to endocrinopathies or skeletal diseases such as Cushing’s syndrome or Paget’s disease. The clinical syndrome associated with LSS is usually neurogenic claudication, which often presents as lower back and extremity pain, numbness, and tingling (1). Priapism, defined as a prolonged and undesired erection in the absence of sexual stimulation, is a rare finding in the context of LSS. Herein, we describe a case of LSS with neurogenic claudication and intermittent priapism, which were completely resolved following minimally invasive surgery.
Case presentation
History and physical
A 33-year-old male experienced onset of lower back pain and neurogenic claudication symptoms in 2013. The patient was evaluated at an outside clinic and diagnosed with degenerative joint disease. At that time, he noted back pain rated as a 7/10 with lower extremity tingling, weakness, and numbness. He denied bladder and bowel incontinence. The treatment regimen was conservative, consisting of analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy. Conservative therapies reduced pain to a 5/10 rating; however, the patient still required multiple leaves of absence from his occupation.
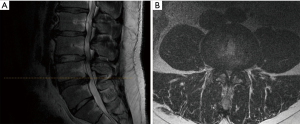
The patient presented to the senior author (LAT) for progressively worsening symptoms in 2018. His lower extremity pain radiated to both feet and was exacerbated by both standing and walking approximately 50 feet. Associated symptoms such as numbness and tingling persisted and remained unchanged. Furthermore, the patient noted uncontrolled erections while walking, which almost always occurred in conjunction with his worsening bilateral leg numbness. The patient exhibited slight gait instability but denied falls. The physical exam revealed normal muscle bulk and tone without weakness. MRI of his lumbar spine revealed severe stenosis at L2–3 and L3–4, as well as a L4–5 disc herniation (Figure 1). The patient’s presentation was consistent with a diagnosis of LSS with neurogenic claudication. Given the progressive nature of symptoms, the patient elected to have decompression surgery.
Of note, the differential for priapism consists of, but is not limited to, blood disorders, adverse drug reactions, and pelvic trauma—all of which were of low clinical suspicion for this patient. Extensive urological evaluation was avoided given that episodes of priapism were not notable for penile pain and self-resolved within minutes following cessation of ambulation. These factors offered reassurance that the risk of long-term urologic damage was low.
Operative and postoperative course
After successfully intubation, the patient was placed in the prone position on a Jackson table using Wilson frame. The lumbar area was prepped and draped in the usual fashion. A 2 cm midline incision was made at L2–3; sequential dilators were used to gain access to the right hemi-lamina and an 18 mm tube was used to maintain exposure. The microscope was brought into the field and a right hemi-laminectomy was performed with high-speed burr. Bilateral decompression was achieved via the unilateral hemi-laminectomy using high-speed burr at right L2–3 by under-cutting the lamina on the left side. At this level, the ligamentum flavum, which demonstrated substantial hypertrophy, was removed using curettes and Kerrison rongeurs. Decompression was confirmed with Woodson probe. The same steps were repeated at the L3–4 and L4–5 levels to achieve decompression. At L4–5, a microdiscectomy was also performed to remove the herniated disc fragment. The wound was thoroughly irrigated and closed with vicryl sutures and skin glue. The patient was successfully extubated then transferred to PACU in stable condition.
Surgical and pathologic findings confirmed admission diagnosis of LSS with neurogenic claudication. The post-operative course was uncomplicated. The patient’s pain was well controlled. The patient was discharged on post-operative day (POD) 1. At his 6-week follow-up visit, the patient revealed complete resolution of spontaneous priapism and postural instability. Furthermore, severity of claudication symptoms was markedly decreased. During this visit, the senior author requested and received verbal consent from the patient to publish these findings.
Discussion
LSS is one of the most commonly diagnosed spinal conditions and affects more than 200,000 people in the United States (5,6). Although symptoms and neurologic findings vary, LSS is characterized by lower back and lower extremity pain, paresthesia, numbness, and weakness. Foraminal or lateral recess stenosis is associated with unilateral radiculopathy while central canal stenosis usually presents with bilateral symptoms (7,8). Neurogenic claudication is the cardinal sign of LSS, which is characterized as the posture-dependent progressive onset of lower extremity pain, paresthesia, and numbness while standing, walking, or performing any activity that requires extension of the lumbar spine. Weakness, manifesting as foot drop or knee buckling, can be experienced before the onset of pain (9). Patients will often relieve the debilitating pain by assuming a stooped posture, which increases central canal or lateral recess space and subsequently decreases pressure on neural tissue and vasculature (10).
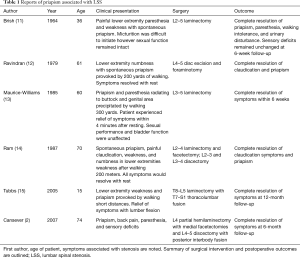
Autonomic dysfunction is rarely observed in patients with LSS; however, a subset of male patients has been reported to experience intermittent priapism associated with the onset of neurogenic claudication symptoms (Table 1). Priapism is defined as an erection in the absence of sexual arousal and/or stimulation. An erection in a healthy patient is mediated by a reflex mechanism from the S2–S4 segments of the cord. Tactile stimuli are transmitted to the cord via dorsal roots of S2–S4 (15). The reflex loop is completed with parasympathetic input from the perineal branches of the pudendal nerve, arising from the same levels, which stimulates the shunting of arterial blood in the corpus cavernosa erectile tissue of the penis (12). Sympathetic stimuli from the hypogastric nerve trigger vasoconstriction within the corpus cavernosa resulting in penile relaxation. In patients with LSS and intermittent priapism, mechanical compression of the thecal sac is thought to increase parasympathetic reflex activity (16).
Full table
The combination of priapism and neurogenic claudication in the context of LSS has been observed in a broad range of ages, coexisting conditions, and LSS etiologies (11). Cansever et al. describes the case of a 74-year-old man who presented with LSS neurogenic claudication and intermittent priapism (2). L4 partial hemilaminectomy with medial facetectomies were performed and the patient noted complete resolution of all symptoms at the 6-month follow-up. Similarly, Maurice-Williams et al. reported complete resolution of symptoms following decompression surgery in patient who also presented with neurogenic claudication and intermittent priapism (13). Furthermore, a 15-year-old male with achondroplasia reported the onset of bilateral lower extremity weakness provoked by walking. He received relief within 10 minutes after assuming the fetal position. The patient underwent extensive thoracolumbar fusion from T7–S1 and was completely asymptomatic at the 12-month follow-up (15).
Baba et al. contributed the most comprehensive examination of LSS with intermittent priapism to date (16). They report the results of electrophysiological studies as well as imaging studies for seven patients with LSS and spontaneous priapism with an average follow-up time of 3.3 years. Priapism was provoked by a range of anatomical positions including walking, standings, and squatting while defecating in the lavatory. Furthermore, the patients exhibited variable exercise intolerance. Some became symptomatic after walking 50 meters while others noted the onset of priapism after walking 300 meters. MRI revealed various degrees of arachnoiditis in three patients, highlighting a possible pathological role of inflammation of the meninges in addition to mechanical compression of the thecal sac.
Herein, we report the case of a 33-year-old male who presented with neurogenic claudication and intermittent priapism caused by LSS. Priapism is a rare clinical finding associated with LSS; however, our case and others in the literature demonstrate the utility of decompressive surgery in the resolution of these symptoms.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Katz JN, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum 1995;38:1236-41. [Crossref] [PubMed]
- Cansever T, Civelek E, Sencer A, et al. Intermittent priapism in degenerative lumbar spinal stenosis: case report. Turk Neurosurg 2007;17:260-3. [PubMed]
- Singh K, Samartzis D, Vaccaro AR, et al. Congenital lumbar spinal stenosis: a prospective, control-matched, cohort radiographic analysis. Spine J 2005;5:615-22. [Crossref] [PubMed]
- Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006.198-207. [Crossref] [PubMed]
- Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J 2009;9:545-50. [Crossref] [PubMed]
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ 2016;352:h6234. [Crossref] [PubMed]
- Lee CK, Rauschning W, Glenn W. Lateral lumbar spinal canal stenosis: classification, pathologic anatomy and surgical decompression. Spine 1988;13:313-20. [Crossref] [PubMed]
- Reynolds AF, Weinstein PR, Wachter RD. Lumbar monoradiculopathy due to unilateral facet hypertrophy. Neurosurgery 1982;10:480-6. [Crossref] [PubMed]
- Binder DK, Schmidt MH, Weinstein PR. Lumbar spinal stenosis. Semin Neurol 2002;22:157-66. [Crossref] [PubMed]
- Wilson CB. Significance of the small lumbar spinal canal: cauda equina compression syndromes due to spondylosis. 3: intermittent claudication. J Neurosurg 1969;31:499-506. [Crossref] [PubMed]
- Brish A, Lerner MA, Braham J. Intermittent claudication from compression of cauda equina by a narrowed spinal canal. J Neurosurg 1964;21:207-11. [Crossref] [PubMed]
- Ravindran M. Cauda equina compression presenting as spontaneous priapism. J Neurol Neurosurg Psychiatry 1979;42:280-2. [Crossref] [PubMed]
- Maurice-Williams RS, Marsh HT. Priapism as a feature of claudication of the cauda equina. Surg Neurol 1985;23:626-8. [Crossref] [PubMed]
- Ram Z, Findler G, Spiegelman R, et al. Intermittent priapism in spinal canal stenosis. Spine 1987;12:377-8. [Crossref] [PubMed]
- Tubbs RS, Oakes WJ. An unusual presentation of achondroplasia. Case report. J Neurosurg 2005;103:170-1. [PubMed]
- Baba H, Maezawa Y, Furusawa N, et al. Lumbar spinal stenosis causing intermittent priapism. Paraplegia 1995;33:338-45. [PubMed]


