
Complication avoidance and management in ambulatory spine surgery
Introduction
The volume of outpatient spine procedures has increased steadily over the past several decades (1-4). As indications expand to encompass an increasing variety of procedures, there has been focus in the literature on detailing the outcomes and examining the appropriateness of outpatient spine surgery (5-11). Despite an abundance of studies supporting the safety of ambulator spine surgery, concerns remain regarding the generalizability of these findings to the population at large given the observed selection bias toward young, healthy patients (12). While careful patient selection has served to limit complications after outpatient spine surgery, both intra- and postoperative complications can be devastating when they arise in the ambulatory setting. Patient and provider education, awareness of potential complications and their management, as well as creation of protocols to prevent and address complications serve to mitigate the potential risks of ambulatory spine surgery.
Safety profile of ambulatory spine surgery
Ambulatory lumbar microdiscectomy was first described in the mid-1980s—excellent outcomes were reported in one series of 103 prospectively-collected patients, three of whom required overnight observation for urinary retention or persistent nausea and vomiting (13). Similarly, anterior cervical discectomy and fusion (ACDF) has been practiced in the outpatient setting for decades. Stieber et al. first reported their experience with outpatient one- and two-level ACDF performed in a freestanding ambulatory surgery center between 1998 and 2004, noting a lower complication rate compared to inpatient controls (14). Over time, advances in technology have expanded the compendium of spine procedures offered in the outpatient setting. Chin et al. found that outpatient single-level lateral lumbar interbody fusion (LLIF) could be successfully performed, noting only two instances of postoperative dermatomal numbness, no instances of post-operative weakness, and no extended stay admissions or readmissions for complications (8). Hirsch et al. determined that minimally invasive tubular revision lumbar decompression was safe in a carefully selected patient population, reporting a single instance of superficial wound infection as the only complication among 35 outpatient cases (9). Outpatient cervical disc replacement, transforaminal lumbar interbody fusion (TLIF), posterior cervical foraminotomy, and anterior lumbar interbody fusion (ALIF) have also been described (15-18).
Studies have consistently reported low complication rates following outpatient spine surgery, though with the caveat that an inherent selection bias likely exists (2,7,12,19,20). Patients undergoing outpatient procedures in these studies were typically younger and healthier than individuals having surgery on an inpatient basis, thus limiting the generalizability of the findings to the population at large.
Some studies have attempted to control for this bias. Bovonratwet et al. queried the National Surgical Quality Improvement Program (NSQIP) database to identify a cohort of 360 patients undergoing posterior lumbar fusion (PLF) (6). On average, patients who had outpatient surgery had fewer instrumented levels, were more likely to be male, and tended to have lower American Society of Anesthesiologist (ASA) scores. However, these differences lost significance after propensity score matching, and adverse event rates were similar between the inpatient and outpatient cohorts. A study by Khanna et al. found that, after matching, overall complications and readmissions were higher for those undergoing inpatient ACDF (21).
Outpatient spine surgery can be performed safely, though perhaps not in all patients or all settings. Careful attention should be paid to patient, surgeon, and institutional factors which can affect outcomes.
Common complications
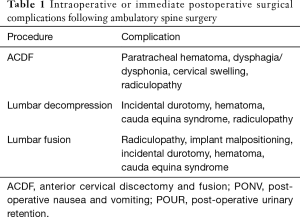
Though the literature largely supports the safety of outpatient spine surgery, complications may occur in any setting. Complications most frequently encountered in outpatients are similar to those seen in inpatients, though perhaps at lower rates due to patient selection (Table 1).
Full table
ACDF
Numerous studies have been published on the safety of ambulatory ACDF. Sheperd and Young reported on a series of 150 patients undergoing outpatient one- or two-level ACDF, demonstrating a 3.9% complication rate with six patients returning to the hospital due to neck pain, dysphagia, nausea, and/or cervical swelling (22). A prospective study of 96 patients undergoing one- or two-level outpatient ACDF reported a 5.2% morbidity rate, including two instances of postoperative dysphagia, two cases of postoperative hematoma, and one readmission for neurologic decline (23). Another study of 1,000 consecutive outpatient one- and two-level ACDFs reported two instances of reoperation for hematoma evacuation, 14 readmissions for dysphagia, two for surgical site infection (SSI), and two for new nerve root deficits (24).
A large single-surgeon case series from Norway reported on 1,449 consecutive patients undergoing outpatient spine surgery (25). Of their cohort, 376 underwent cervical procedures with an overall complication rate of 2.6%. Cervical complications included postoperative hematoma which was noted and evacuated in the immediate postoperative period (0.5%), neurological deterioration including two instances of acute stroke noted on the date of surgery (0.8%), incidental durotomy (0.3%), and persistent dysphagia or dysphonia (1.0%). A meta-analysis of studies on outpatient ACDF meeting at least Oxford Center for Evidence-Based Medicine Level 3 evidence found that the most commonly reported complication associated with outpatient ACDF was dysphagia (1.6%) with neck hematoma, new nerve root deficit, neurologic deterioration, and SSI occurring less frequently (26).
Lumbar decompression
The most commonly reported complication following ambulatory lumbar decompression is incidental durotomy, though anesthetic-related complications are also frequently observed. A retrospective Canadian study reported a 6.9% complication rate in a cohort of 406 patients undergoing primary or revision outpatient microdiscectomy (27). The majority of the 28 recorded complications were durotomy (20/28), though transient or permanent radiculopathy (7/28) and urinary retention (1/28) were also observed. A single-surgeon study of 122 consecutive patients reported a 4.9% complication-related rate of conversion to inpatient status—there were two incidental durotomies, three instances of anesthetic-related complications (post-operative nausea and vomiting, urinary retention), and one case of laryngospasm requiring re-intubation (28). In their series of 1,449 outpatient spine surgeries (1,073 of which were lumbar microdiscectomies), Helseth et al. reported 14 incidental durotomies (25). Ahuja and Sharma reported their experience with outpatient microdiscectomy in the United Kingdom—of the 95 patients included in the analysis, three (3.2%) suffered intraoperative complications necessitating inpatient admission (including one episode of transient heart block and two incidental durotomies) and seven (7.4%) had various postoperative complications (prolonged nausea and vomiting, partial foot drop, prolonged anesthetic recovery) which precluded same-day discharge (29).
Complications related to the surgical site are also frequently reported. Pugely et al. used the NSQIP database to identify 1,652 patients who had undergone outpatient microdiscectomy, noting a 3.45% complication rate (30). A third of the recorded complications were superficial or deep wound infection or wound dehiscence. Helseth et al. reported 13 cases of postoperative infection, six of which required readmission for irrigation and debridement within 30 days of surgery (25). This series also included seven cases of postoperative hematoma, six of which were noted and evacuated prior to discharge home, and one case of a retroperitoneal hematoma managed with transfusion in the inpatient setting. Recurrent disc herniation has also been observed. A large, single-surgeon retrospective study reported an 8.6% complication rate in 1,322 consecutive patients, with the most common complication being recurrent disc herniation (6.4%) (31). Incidental durotomy (0.2%), urinary retention (0.2%), infection (0.5%), and hematoma/seroma (0.3%) comprised the remainder of the reported complications.
Medical complications following ambulatory spine surgery are uncommon. In a propensity-matched comparison of readmission rates following inpatient and outpatient lumbar discectomy, Pugely et al. reported significantly lower rates of medical complications requiring readmission within 30 days of discharge after outpatient lumbar discectomy. Complications in the outpatient cohort included pneumonia, deep vein thrombosis (DVT) and pulmonary embolus (PE), renal insufficiency, and urinary tract infection (32). It should be noted that medical complications observed after discharge may occur postoperatively regardless of the surgical setting and are more likely attributable to patient selection rather than the inherent safety profile of ambulatory surgery.
Lumbar fusion
A case series comparing a cohort of 32 patients undergoing minimally invasive TLIF in the ambulatory setting to 64 patients staying in the hospital at least overnight found no difference in postoperative complication rates (16). In the outpatient cohort, the authors reported two cases of postoperative radiculopathy due to implant malpositioning and one case of rod disengagement. Postoperative hematoma, incidental durotomy, and SSI were also recorded in the inpatient cohort but not in the outpatient cohort, although it is certainly conceivable that such complications could occur in either setting. Villavicencio et al. retrospectively reported their experience with ambulatory TLIF performed through a mini-open approach noting nine complications in 27 patients (33). There were two instances of malpositioned hardware, three incidental durotomies, and one case of pericarditis. After discharge, two patients presented to and were managed in the emergency department (one for constipation and one for incidental durotomy) and two were readmitted within one week of surgery (one for pain control and another for a wound infection). In a cohort of 30 patients undergoing lateral interbody fusion in an ambulatory surgery center, Chin et al. reported a 7% rate of dermatomal numbness, but there were no cases of weakness or inability to walk, an adverse event that was observed in a comparative inpatient cohort (34). Nonetheless, it must be emphasized that the outpatient setting does not shield surgeons and their patients from complications inherent to a given procedure.
Complication avoidance
Undoubtedly, patient selection plays a role in the safety profile of ambulatory spine surgery. Numerous studies have noted that ambulatory surgery is preferentially offered to younger, healthier patients which may limit the generalizability of the results (2,6,19,25,35). However, others have reported good outcomes in elderly patients and a trend toward offering ambulatory spine surgery to patients 60 years of age or older (1,36). In general, however, limiting outpatient surgery to medically optimized patients undergoing less technically-challenging surgery can minimize rates of complications, hospital transfer, and readmission (37).
In higher risk patients, it may be prudent to perform same-day surgery in a hospital-based center where the option for overnight admission is readily available in the event complications arise in the immediate postoperative setting. However, when performed at ambulatory surgery centers, procedures should be in place for transfer to an inpatient setting with the capability to manage potential major complications. A recent survey assessing the current practices of spine surgeons performing ambulatory surgery in the United States found that only 48.3% of respondents operated in an ambulatory surgery center where 23-hour observation was available, while the remainder indicated that patients requiring an extended postoperative stay would require transfer to another facility. A complication that could not be managed in the outpatient setting was reported by 10.3% of surgeons, and 92% of all respondents indicated that there was an institutional protocol in place should such an event occur (38).
Patient education before surgery is critical. Providing patients with information to reference regarding postoperative management and expectations—including appropriate analgesic use at home, potential complications to be aware of, and appropriate contact information should complications arise—can help to allay patients’ concerns, minimize the potential for complications, and decrease the likelihood of readmission. This teaching is best performed prior to the day of surgery so that patients have time to process the information. In addition to verbal education and confirmation of adequate understanding from patients and family members, several authors have advocated for written instruction detailing postoperative expectations and emergency contact numbers in the event of issues (29,39).
Given the increasing push to limit opioid use, multimodal pain management protocols have been widely adopted, including use of local analgesic infiltration, non-steroidal analgesics, and cortisone formulations to aid in pain management and reduce opioid intake. Limiting opioid analgesia both pre- and intraoperatively has been recommended to decrease the risk of postoperative nausea and vomiting (40) and can decrease rates of opioid-related respiratory depression which may otherwise necessitate inpatient observation and management. Awake endoscopic TLIFs using sedation and local anesthetic to completely obviate the need for general anesthetic and opioid medications has been described with clinical success (41). Early recovery after surgery (ERAS) protocols may also improve patient pain levels without the addition of opioids and the myriad potential adverse events which can result from opioid use and misuse after surgery. ERAS protocols provide a framework to speed recovery and decrease length of stay, focusing on patient education, preoperative nutritional optimization, and postoperative multimodal analgesia, early nutrition and early mobilization (42). Several studies of ERAS have demonstrated excellent results for various spine procedures—reduced operative time, blood loss, complication rates, and readmission rates have been reported (43,44).
Prolonged surgical times and intraoperative blood loss have been associated with an increased risk of complications associated (45-47). As such, it is important to select procedures that can be consistently performed in an efficient timeframe if considering outpatient surgery. Surgeons must be introspective and realistic about their individual skill level and would be well served by timing their procedures prior to making a switch to ambulatory surgery, especially if considering operating in a stand-alone ambulatory surgery center rather than a hospital outpatient department.
In addition to selecting less technically demanding cases, utilization of minimally invasive approaches in the outpatient setting may decrease complications associated with intraoperative blood loss as well as rates of surgical site infection. A meta-analysis of studies comparing outcomes between minimally invasive surgery (MIS) and open posterior lumbar and transforaminal fusion found a pooled estimated blood loss ranging from 51 to 496 cc for MIS procedures versus 125 to 1,147 cc in open procedures (48). MIS techniques may also decrease rates of SSI compared to open surgery (49,50). Mueller et al. retrospectively reviewed infection rates after 961 MIS and 481 open lumbar spine procedures, observing an overall SSI rate of 0.5% in MIS lumbar surgery compared with 3.3% for open techniques (50). Another review of 1,338 lumbar MIS decompressions and fusions found an overall SSI rate of 0.22% (49).
Careful attention should be paid to maintaining meticulous hemostasis throughout the procedure to limit the incidence of postoperative hematoma. Risk factors for development of postoperative hematoma include preoperative use of non-steroidal anti-inflammatory medications, multilevel procedures, and known preoperative coagulopathy or elevated international normalized ratio (INR) (51,52). Anticoagulants should be stopped prior to surgery in accordance with published guidelines and/or hospital policies (53). Bone wax, topical hemostatic agents including hemostatic sponges and fibrin sealants, and use of bipolar electrocautery can be helpful in maintaining hemostasis (54). Some authors recommend discharging outpatient anterior cervical patients with a penrose drain in place and instructions to remove it 24 hours postoperatively (55). Hemostasis is also extremely important in lumbar tubular surgeries where a relatively small hematoma may cause symptomatic compression of the neural elements given the relative lack of dead space compared to open procedures.
Postoperative urinary retention (POUR) is an uncommon issue following outpatient spine surgery, but it nonetheless does occur. Altschul et al. found that patients with preexisting benign prostatic hypertrophy (BPH), chronic constipation, and prior urinary retention undergoing posterior lumbar surgery were at an increased risk for developing POUR in an inpatient cohort (56). Prophylactic 5-alpha reductase inhibitors may be initiated before surgery in patients with a history of BPH to prevent retention (57). Limiting intraoperative intravenous fluids, opioids, and overall surgical time may also decrease the incidence of POUR (58).
Complication management
While careful consideration of the above can help avoid complications in outpatient spine surgery, complications should be proactively managed when they do occur. Intraoperative complications are managed in an identical manner as they would be in an inpatient setting, and those requiring advanced levels of care (e.g., significant vascular injuries) may require emergent transfer to a hospital in which such services are available.
Incidental durotomy is a frequently reported complication in both the inpatient and ambulatory setting and can lead to significant morbidity when unrecognized or inadequately treated. When possible, incidental durotomy should be addressed with primary repair (59,60). If poor tissue quality or access precludes primary suture repair, use of fibrin glue, collagen matrix, and/or muscle or fat graft have been described as alternatives or adjuncts to primary repair (61-64). Successful durotomy closure using specialized instruments or metallic clips has also been reported in the setting of MIS spine surgery (65,66). Intraoperative Valsalva and Trendelenburg have been shown to be useful in evaluating the adequacy of the repair (62,67). There is not strong evidence to support the traditional dogma that the occurrence of an intraoperative incidental durotomy requires postoperative bedrest. In fact, good outcomes have been reported by allowing patient to ambulate postoperatively and only restricting their activity if symptoms develop (68). Admission for observation and bed rest after incidental durotomy may be indicated based on the adequacy of the repair and may be employed for symptomatic treatment in the event of postural headache, dizziness, or nausea and vomiting thought to be secondary to cerebrospinal fluid leak. If asymptomatic postoperatively, patients may be discharged home at the surgeon’s discretion.
Perhaps the most concerning of the potential postoperative complications with outpatient spine surgery, particularly in the setting of anterior cervical procedures, is catastrophic airway compromise. A period of postoperative monitoring prior to discharge can help to minimize the risk of morbidity and mortality from an acute paratracheal hematoma, though patients and surgeons should be well aware that retropharyngeal hematoma has been reported to occur for up to one week following anterior cervical surgery (19,69-71). The present literature lacks consistent guidelines for the duration of observation prior to discharge, but a period of six hours postoperatively is utilized by the authors. Any patient demonstrating symptoms of postoperative hematoma should be closely monitored with a low threshold for inpatient admission or even emergent return to the operating room for evacuation depending on the severity of the clinical presentation. For patients who are discharged home, thorough education regarding signs and symptoms of potential airway compromise—including surgical site or neck swelling, dysphagia or respiratory distress—should be reviewed at length before discharge.
Epidural hematoma causing acute cauda equina syndrome a major concern for patients undergoing lumbar surgery. Perioperative staff must be aware of the potential for this complication during observation in the immediate postoperative period as most episodes of symptomatic epidural hematoma occur in the first four hours postoperatively (72). Evidence of developing cauda equina syndrome (e.g., urinary retention, increasing lower extremity and back pain, saddle anesthesia) observed prior to discharge should result in emergent return to the operating room for hematoma evacuation. If symptoms are subacute or the suspicion for epidural hematoma is not so great as to merit an immediate return to the operating room, admission or transfer to an inpatient facility with advanced imaging capabilities should be considered (73). Similar to instruction regarding ACDF, patients should be educated on the signs and symptoms of epidural hematoma and given appropriate provider contact information so that they can be evaluated in a timely manner should symptoms develop.
Bladder distension, failure to void within eight hours of surgery, or catheter removal and inability to void with a residual bladder volume greater than 600 mL are signs of urinary retention (74,75). In cases of prolonged retention, providing a comfortable environment and allowing the patient to sit or stand to void may lead to spontaneous voiding. Patients should be admitted for overnight observation if they fail to spontaneously void prior to discharge. Inpatient urology consultation and possible discharge home with an indwelling catheter and outpatient urology follow-up may be indicated in refractory cases.
While several studies have advocated for patients being located near a well-equipped emergency department or large hospital center post-discharge, a study by Pak et al. found that access to outpatient spine clinics after surgery was the only factor independently associated with a reduced rate of emergency department utilization at the 30- and 90-day postoperative timepoints (19,25,40,76,77). In addition to cost savings from reduced unnecessary healthcare resource utilization and its potential associated penalties, outpatient spine clinics can serve as a resource for postoperative patients with concerns which may or may not merit escalation to an emergency department visit or hospital admission.
Appropriate management and safe discharge after surgical or medical complications requires communication between the surgeon, anesthesiologist and perioperative care staff. In all cases, patients should be admitted to the inpatient setting if deemed unsafe for discharge by the treating team.
Protocols for an integrated approach
Ultimately, creation of surgeon and institutional protocols can help to systematically address potential complications and limit them in the first place through adequate safeguards and appropriate indications. Helseth et al. utilize a postoperative checklist to determine when patients are eligible for discharge—required items included adequate pain control, wound hemostasis, stable neurologic status, and the ability to drink, urinate and ambulate (25). Patients must be monitored by a family member or friend during the first night postoperatively; they are contacted the day after surgery; and a board-certified neurosurgeon is on call at all times.
In a study from Canada, where limited inpatient beds and long wait-times have pushed hospitals and providers toward ambulatory cases, Bednar detailed a protocol developed for overnight (23-hour stay) stay spine surgery (39). While the author performed open surgery in a hospital setting where patients were observed overnight, the tenets are applicable to same-day surgery. First among these was patient selection. Beyond age and comorbidities, independent ambulation and social support were considered as they ease the burden of postoperative care in the home. Patients had to fully understand the postoperative instructions and share the expectation that they would be discharged home in an agreed upon timeframe. Postoperative instructions and expectations tailored to the procedure—either cervical or lumbar—were reviewed at length with patients prior to surgery. In addition to preoperative medical and anesthesia assessment and referral to appropriate specialists for clearance, patients in this study were asked to stop smoking for a minimum of six weeks prior to surgery. A standardized postoperative pain management regimen and observation period were utilized for all patients. Using this protocol for a variety of cases (e.g., microdiscectomy, lumbar decompression, lumbar fusion and ACDF), the author reported successful next-day discharge for 122 of 124 patients included in the study—two patients were admitted for urinary retention. This study details one surgeon’s experience, with the caveat that it was conducted in the setting of overnight-stay surgery which allows for in-hospital management of immediate postoperative issues that may have otherwise resulted in inpatient conversion or readmission of discharged patients. Regardless, the creation of evidence-based protocols can help to systematically address the multiple variables associated with successful ambulatory spine surgery, decreasing the risk for negative outliers.
Conclusions
The reassuring safety profile of outpatient spine surgery, at least among relatively healthy patients, is well established, but complications may still occur. Institutional protocols should be developed to guide patients and providers through the pre-, intra-, and postoperative periods. Standardized selection criteria and appropriate preoperative screening and education are modifiable factors which may limit complications. Utilizing anesthetic techniques to facilitate rapid recovery and multimodal pain management strategies which limit PONV and urinary retention increases rates of successful same-day discharge without detrimental effects on outcomes. Intraoperative strategies to limit bleeding and subsequent hematoma formation can also decrease postoperative complications after ambulatory spine surgery. Anticipation, recognition and timely management of adverse events can be life-saving. In the event complications do occur, ASCs should have protocols in place for patient transfer to the inpatient setting for additional management and observation.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Sheha has no conflicts of interest to report. Dr. Derman receives research support from and is a consultant to Orthofix Medical Inc.; he also receives research support from Aesculap Implant Systems, LLC.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Arshi A, Park HY, Blumstein GW, et al. Outpatient Posterior Lumbar Fusion: A Population-Based Analysis of Trends and Complication Rates. Spine (Phila Pa 1976) 2018;43:1559-65. [Crossref] [PubMed]
- Baird EO, Egorova NN, McAnany SJ, et al. National trends in outpatient surgical treatment of degenerative cervical spine disease. Global Spine J 2014;4:143-50. [Crossref] [PubMed]
- Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976) 2006;31:1957-63; discussion 1964.
- Idowu OA, Boyajian HH, Ramos E, et al. Trend of Spine Surgeries in the Outpatient Hospital Setting Versus Ambulatory Surgical Center. Spine (Phila Pa 1976) 2017;42:E1429-36. [Crossref] [PubMed]
- Lee MJ, Kalfas I, Holmer H, et al. Outpatient surgery in the cervical spine: is it safe? Evid Based Spine Care J 2014;5:101-11. [Crossref] [PubMed]
- Bovonratwet P, Ottesen TD, Gala RJ, et al. Outpatient elective posterior lumbar fusions appear to be safely considered for appropriately selected patients. Spine J 2018;18:1188-96. [Crossref] [PubMed]
- Fu MC, Gruskay JA, Samuel AM, et al. Outpatient Anterior Cervical Discectomy and Fusion is Associated With Fewer Short-term Complications in One- and Two-level Cases: A Propensity-adjusted Analysis. Spine (Phila Pa 1976) 2017;42:1044-9. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Lateral Lumbar Interbody Fusion in Ambulatory Surgery Centers. Spine (Phila Pa 1976) 2016;41:686-92. [Crossref] [PubMed]
- Hirsch BP, Khechen B, Patel DV, et al. Safety and Efficacy of Revision Minimally Invasive Lumbar Decompression in the Ambulatory Setting. Spine (Phila Pa 1976) 2019;44:E494-9. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Seale JA, et al. Clinical Outcomes of Outpatient Cervical Total Disc Replacement Compared With Outpatient Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:E567-74. [Crossref] [PubMed]
- Wohns R. Safety and cost-effectiveness of outpatient cervical disc arthroplasty. Surg Neurol Int 2010;1:77. [Crossref] [PubMed]
- Mundell BF, Gates MJ, Kerezoudis P, et al. Does patient selection account for the perceived cost savings in outpatient spine surgery? A meta-analysis of current evidence and analysis from an administrative database. J Neurosurg Spine. 2018;29:687-95. [Crossref] [PubMed]
- Zahrawi F. Microlumbar discectomy. Is it safe as an outpatient procedure? Spine (Phila Pa 1976) 1994;19:1070-4. [Crossref] [PubMed]
- Stieber JR, Brown K, Donald GD, et al. Anterior cervical decompression and fusion with plate fixation as an outpatient procedure. Spine J 2005;5:503-7. [Crossref] [PubMed]
- Gornet MF, Buttermann GR, Wohns R, et al. Safety and Efficiency of Cervical Disc Arthroplasty in Ambulatory Surgery Centers vs. Hospital Settings. Int J spine Surg 2018;12:557-64. [Crossref] [PubMed]
- Emami A, Faloon M, Issa K, et al. Minimally Invasive Transforaminal Lumbar Interbody Fusion in the Outpatient Setting. Orthopedics 2016;39:e1218-22. [Crossref] [PubMed]
- Branch BC, Hilton DL, Watts C. Minimally invasive tubular access for posterior cervical foraminotomy. Surg Neurol Int 2015;6:81. [Crossref] [PubMed]
- Schoeff J. ALIF Surgery in ASC: A Strategy for Success Ambulatory Spine Surgery/Multimodal Analgesia Techniques. 2018 [cited 2019 Jun 24]. Available online: https://www.vumedi.com/channel/society-for-minimally-invasive-spine-surgery/tab/ambulatory-spine-surgery-multimodal-analgesia-techniques/video/alif-surgery-in-asc-a-strategy-for-success/
- Patel DV, Yoo JS, Haws BE, et al. Comparative analysis of anterior cervical discectomy and fusion in the inpatient versus outpatient surgical setting. J Neurosurg Spine 2019.1-6. [Epub ahead of print]. [PubMed]
- Purger DA, Pendharkar AV, Ho AL, et al. Outpatient vs Inpatient Anterior Cervical Discectomy and Fusion: A Population-Level Analysis of Outcomes and Cost. Neurosurgery 2018;82:454-64. [Crossref] [PubMed]
- Khanna R, Kim RB, Lam SK, et al. Comparing Short-term Complications of Inpatient Versus Outpatient Single-level Anterior Cervical Discectomy and Fusion: An Analysis of 6940 Patients Using the ACS-NSQIP Database. Clin spine Surg 2018;31:43-7. [Crossref] [PubMed]
- Sheperd CS, Young WF. Instrumented outpatient anterior cervical discectomy and fusion: is it safe? Int Surg 2012;97:86-9. [Crossref] [PubMed]
- Lied B, Rønning PA, Halvorsen CM, et al. Outpatient anterior cervical discectomy and fusion for cervical disk disease: a prospective consecutive series of 96 patients. Acta Neurol Scand 2013;127:31-7. [Crossref] [PubMed]
- Adamson T, Godil SS, Mehrlich M, et al. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine 2016;24:878-84. [Crossref] [PubMed]
- Helseth Ø, Lied B, Halvorsen CM, et al. Outpatient Cervical and Lumbar Spine Surgery is Feasible and Safe: A Consecutive Single Center Series of 1449 Patients. Neurosurgery 2015;76:728-37; discussion 737-8. [Crossref] [PubMed]
- McClelland S, Oren JH, Protopsaltis TS, et al. Outpatient anterior cervical discectomy and fusion: A meta-analysis. J Clin Neurosci 2016;34:166-8. [Crossref] [PubMed]
- Fallah A, Massicotte EM, Fehlings MG, et al. Admission and Acute Complication Rate for Outpatient Lumbar Microdiscectomy. Can J Neurol Sci 2010;37:49-53. [Crossref] [PubMed]
- Singhal A, Bernstein M. Outpatient Lumbar Microdiscectomy: A Prospective Study in 122 Patients. Can J Neurol Sci 2002;29:249-52. [Crossref] [PubMed]
- Ahuja N, Sharma H. Lumbar microdiscectomy as a day-case procedure: Scope for improvement? Surgeon 2018;16:146-50. [Crossref] [PubMed]
- Pugely AJ, Martin CT, Gao Y, et al. Outpatient surgery reduces short-term complications in lumbar discectomy: an analysis of 4310 patients from the ACS-NSQIP database. Spine (Phila Pa 1976) 2013;38:264-71. [Crossref] [PubMed]
- Best NM, Sasso RC. Success and safety in outpatient microlumbar discectomy. J Spinal Disord Tech 2006;19:334-7. [Crossref] [PubMed]
- Pugely AJ, Martin CT, Gao Y, et al. Causes and risk factors for 30-day unplanned readmissions after lumbar spine surgery. Spine (Phila Pa 1976) 2014;39:761-8. [Crossref] [PubMed]
- Villavicencio AT, Nelson EL, Mason A, et al. Preliminary Results on Feasibility of Outpatient Instrumented Transforaminal Lumbar Interbody Fusion. J Spinal Disord Tech 2013;26:298-304. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Lateral Lumbar Interbody Fusion in Ambulatory Surgery Centers: Patient Selection and Outcome Measures Compared With an Inhospital Cohort. Spine (Phila Pa 1976) 2016;41:686-92. [Crossref] [PubMed]
- Bekelis K, Missios S, Kakoulides G, et al. Selection of patients for ambulatory lumbar discectomy: Results from four US states. Spine J 2014;14:1944-50. [Crossref] [PubMed]
- Best NM, Sasso RC. Outpatient lumbar spine decompression in 233 patients 65 years of age or older. Spine (Phila Pa 1976) 2007;32:1135-9; discussion 1140. [Crossref] [PubMed]
- Sivaganesan A, Hirsch B, Phillips FM, et al. Spine Surgery in the Ambulatory Surgery Center Setting: Value-Based Advancement or Safety Liability? Neurosurgery 2018;83:159-65. [Crossref] [PubMed]
- Baird EO, Brietzke SC, Weinberg AD, et al. Ambulatory Spine Surgery: A Survey Study. Global Spine J 2014;4:157-60. [Crossref] [PubMed]
- Bednar DA. Description and Results of a Comprehensive Care Protocol for Overnight-Stay Spine Surgery in Adults. Spine (Phila Pa 1976) 2017;42:E871-5. [Crossref] [PubMed]
- Mohandas A, Summa C, Worthington WB, et al. Best Practices for Outpatient Anterior Cervical Surgery: Results From a Delphi Panel. Spine (Phila Pa 1976) 2017;42:E648-59. [Crossref] [PubMed]
- Kolcun JPG, Brusko GD, Basil GW, et al. Endoscopic transforaminal lumbar interbody fusion without general anesthesia: operative and clinical outcomes in 100 consecutive patients with a minimum 1-year follow-up. Neurosurg Focus 2019;46:E14. [Crossref] [PubMed]
- Grasu RM, Cata JP, Dang AQ, et al. Implementation of an Enhanced Recovery After Spine Surgery program at a large cancer center: a preliminary analysis. J Neurosurg Spine 2018;29:588-98. [Crossref] [PubMed]
- Soffin EM, Wetmore DS, Beckman JD, et al. Opioid-free anesthesia within an enhanced recovery after surgery pathway for minimally invasive lumbar spine surgery: a retrospective matched cohort study. Neurosurg Focus 2019;46:E8. [Crossref] [PubMed]
- Development of an Enhanced Recovery After Surgery (ERAS) approach for lumbar spinal fusion. J Neurosurg Spine 2017;26:411-8. [Crossref] [PubMed]
- Akins PT, Harris J, Alvarez JL, et al. Risk Factors Associated With 30-day Readmissions After Instrumented Spine Surgery in 14,939 Patients: 30-day readmissions after instrumented spine surgery. Spine (Phila Pa 1976) 2015;40:1022-32. [Crossref] [PubMed]
- Hersey AE, Durand WM, Eltorai AEM, et al. Longer Operative Time in Elderly Patients Undergoing Posterior Lumbar Fusion Is Independently Associated With Increased Complication Rate. Glob spine J 2019;9:179-84.
- Kim BD, Hsu WK, De Oliveira GS, et al. Operative duration as an independent risk factor for postoperative complications in single-level lumbar fusion: an analysis of 4588 surgical cases. Spine (Phila Pa 1976) 2014;39:510-20. [Crossref] [PubMed]
- Goldstein CL, Macwan K, Sundararajan K, et al. Comparative Outcomes of Minimally Invasive Surgery for Posterior Lumbar Fusion: A Systematic Review. Clin Orthop Relat Res 2014;472:1727-37. [Crossref] [PubMed]
- O’Toole JE, Eichholz KM, Fessler RG. Surgical site infection rates after minimally invasive spinal surgery. J Neurosurg Spine 2009;11:471-6. [Crossref] [PubMed]
- Mueller K, Zhao D, Johnson O, et al. The Difference in Surgical Site Infection Rates Between Open and Minimally Invasive Spine Surgery for Degenerative Lumbar Pathology: A Retrospective Single Center Experience of 1442 Cases. Oper Neurosurg (Hagerstown) 2019;16:750-5. [Crossref] [PubMed]
- Kou J, Fischgrund J, Biddinger A, et al. Risk factors for spinal epidural hematoma after spinal surgery. Spine (Phila Pa 1976) 2002;27:1670-3. [Crossref] [PubMed]
- Awad JN, Kebaish KM, Donigan J, et al. Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br 2005;87:1248-52. [Crossref] [PubMed]
- Hornor MA, Duane TM, Ehlers AP, et al. American College of Surgeons’ Guidelines for the Perioperative Management of Antithrombotic Medication. J Am Coll Surg 2018;227:521-536.e1. [Crossref] [PubMed]
- Szpalski M, Gunzburg R, Sztern B. An overview of blood-sparing techniques used in spine surgery during the perioperative period. Eur Spine J 2004;13:S18-27. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Eligibility of Outpatient Spine Surgery Candidates in a Single Private Practice. Clin Spine Surg 2017;30:E1352-8. [Crossref] [PubMed]
- Altschul D, Kobets A, Nakhla J, et al. Postoperative urinary retention in patients undergoing elective spinal surgery. J Neurosurg Spine 2017;26:229-34. [Crossref] [PubMed]
- Roehrborn CG, Bruskewitz R, Nickel JC, et al. Sustained decrease in incidence of acute urinary retention and surgery with finasteride for 6 years in men with benign prostatic hyperplasia. J Urol 2004;171:1194-8. [Crossref] [PubMed]
- Agrawal K, Majhi S, Garg R. Post-operative urinary retention: Review of literature. World J Anesthesiol 2019;8:1-12. [Crossref]
- Tafazal SI, Sell PJ. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J 2005;14:287-90. [Crossref] [PubMed]
- Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res 2001.238-47. [Crossref] [PubMed]
- Jankowitz BT, Atteberry DS, Gerszten PC, et al. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J 2009;18:1169-74. [Crossref] [PubMed]
- Cammisa FP, Girardi FP, Sangani PK, et al. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25:2663-7. [Crossref] [PubMed]
- Narotam PK, José S, Nathoo N, et al. Collagen matrix (DuraGen) in dural repair: analysis of a new modified technique. Spine (Phila Pa 1976) 2004;29:2861-7; discussion 2868-9. [Crossref] [PubMed]
- Shaffrey CI, Spotnitz WD, Shaffrey ME, et al. Neurosurgical applications of fibrin glue: augmentation of dural closure in 134 patients. Neurosurgery 1990;26:207-10. [Crossref] [PubMed]
- Ruban D, O’Toole JE. Management of incidental durotomy in minimally invasive spine surgery. Neurosurg Focus 2011;31:E15. [Crossref] [PubMed]
- Ferroli P, Franzini A, Messina G, et al. Use of self-closing U-clips for dural repair in mini-invasive surgery for herniated disc. Acta Neurochir (Wien) 2008;150:1103-5. [Crossref] [PubMed]
- Khan MH, Rihn J, Steele G, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 2006;31:2609-13. [Crossref] [PubMed]
- Hodges SD, Humphreys SC, Eck JC, et al. Management of incidental durotomy without mandatory bed rest. A retrospective review of 20 cases. Spine (Phila Pa 1976) 1999;24:2062-4. [Crossref] [PubMed]
- Sethi R, Tandon MS, Ganjoo P. Neck hematoma causing acute airway and hemodynamic compromise after anterior cervical spine surgery. J Neurosurg Anesthesiol 2008;20:69-70. [Crossref] [PubMed]
- O’Neill KR, Neuman B, Peters C, et al. Risk factors for postoperative retropharyngeal hematoma after anterior cervical spine surgery. Spine (Phila Pa 1976) 2014;39:E246-52. [Crossref] [PubMed]
- Sagi HC, Beutler W, Carroll E, et al. Airway complications associated with surgery on the anterior cervical spine. Spine (Phila Pa 1976) 2002;27:949-53. [Crossref] [PubMed]
- Kebaish KM, Awad JN. Spinal epidural hematoma causing acute cauda equina syndrome. Neurosurg Focus 2004;16:e1. [PubMed]
- Haws BE, Khechen B, Guntin JA, et al. Complication management in outpatient spine surgery. Semin Spine Surg 2018;30:169-72. [Crossref]
- Jellish WS, Thalji Z, Stevenson K, et al. A prospective randomized study comparing short- and intermediate-term perioperative outcome variables after spinal or general anesthesia for lumbar disk and laminectomy surgery. Anesth Analg 1996;83:559-64. [Crossref] [PubMed]
- Pavlin DJ, Pavlin EG, Gunn HC, et al. Voiding in patients managed with or without ultrasound monitoring of bladder volume after outpatient surgery. Anesth Analg 1999;89:90-7. [PubMed]
- Pak LM, Fogel HA, Chaudhary MA, et al. Outpatient Spine Clinic Utilization is Associated with Reduced Emergency Department Visits following Spine Surgery. Spine (Phila Pa 1976) 2018;43:E836-E841. [Crossref] [PubMed]
- Missios S, Bekelis K. Outpatient continuity of care and 30-day readmission after spine surgery. Spine J 2016;16:1309-14. [Crossref] [PubMed]


