
Anesthesia and postoperative pain control—multimodal anesthesia protocol
Introduction
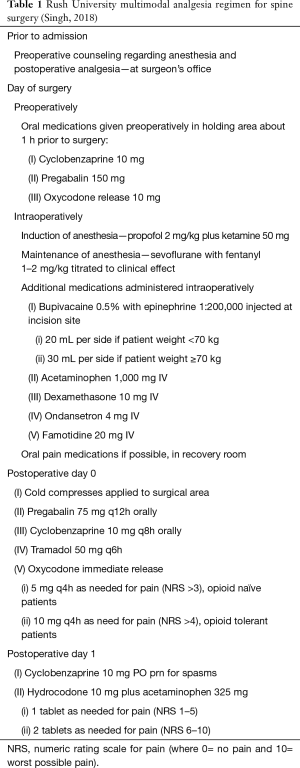
Postoperative pain following spine surgery can originate from the skin, muscle, vertebrae, intervertebral discs, facet joints and neural tissue (1). Multimodal anesthesia (MMA) for pain control has become an important component of the perioperative management of patients undergoing ambulatory spine surgery (Table 1). MMA involves the use of additive or synergistic combinations of analgesics to achieve clinically required analgesia while minimizing significant side effects associated with higher dose of a single equianalgesic medication such as an opioid analgesic. MMA generally involves optimizing non-opioid pharmacologic and non-pharmacologic interventions and reserving opioid use to treat breakthrough pain. Patients receiving medications via MMA protocols are likely to have lower opioid consumption compared to those managed using primarily IV opioid patient-controlled analgesia (2). MMA pain management strategies have become important components of enhanced recovery after surgery (ERAS) protocols in an effort to optimize care by standardizing analgesic medications in the perioperative setting while minimizing adverse effects and improving quality and patient outcomes. These efforts have shown promising results in achieving adequate pain control and reducing use of opioids. The essential goal of a MMA is effective pre-emptive pain management and judicious treatment of breakthrough pain using the lowest doses of opioids required.
Full table
Constructing a MMA protocol
Pharmacological combinations of analgesics and non-pharmacological therapies are the fundamental components of a MMA protocol. Dosing and timing of these agents is also an important consideration as a goal of an effective MMA is to have antinociceptive therapy in place prior to surgery in an effort to minimize or mitigate the burden of pain in the postoperative period. The Rush University Medical Center MMA protocol is shown in Table 1 as an example of such a multifaceted approach.
On the day of surgery, administration of pain medication should start in the preoperative holding area 1 to 2 hours prior to surgery. Most MMA protocols include several different medications by mouth often including a muscle relaxant, a long acting opioid, and an anticonvulsant prior to initiation of the general anesthetic (3). Muscle relaxants such as cyclobenzaprine have been shown to provide significant symptomatic relief when used as therapy for low back pain (4). Though combining cyclobenzaprine with NSAIDs has not been shown to provide significantly different pain relief for acute low back pain compared with monotherapy, it is still more efficacious than opioids in this setting (5). The rationale for administering a opioid analgesic preoperatively is to take advantage of any pre-emptive analgesic effect that the opioid may provide and reduce the need for intravenous opioid postoperatively; which decreases the risk of nausea, pruritus and sedation. The anticonvulsants gabapentin and pregabalin exert their analgesic activity by binding to the presynaptic voltage-gated calcium channels, specifically to the alpha-2-delta protein. This binding reduced calcium influx through these channels and reduces neurotransmitter release. These voltage-gated channels are upregulated in the dorsal root ganglia and spinal cord in response to surgical trauma. By inhibiting calcium influx, central sensitization is reduced, thus reducing analgesic requirements and pain post operatively (6). When used in conjunction with a muscle relaxant and a long acting opioid, superior analgesia is achieved with decreased side effects of the individual drugs. Ketorolac may also be considered both pre and post operatively. It helps reduce inflammatory processes and hypersensitivity by blocking prostaglandins. There is a risk of adverse events when this drug is given after spinal fusion but only when given for greater than 2 days at doses higher than 120 mg/day (7). When ketorolac was given at a safe dose in conjunction with pregabalin and acetaminophen, patients has lower pain scores, better ambulation tolerance, improved functional outcomes, and decreased opioid requirements along with shorter hospital stay with no additional complications (8).
In addition to the agents administered on the day of surgery, many MMA protocols may include starting a selective cyclooxygenase enzyme inhibitor such as celecoxib or meloxicam two to three days prior to surgery, based on the discretion of the surgeon and the type of spine surgery being performed (9). In a study of colorectal surgery patients in an ERAS protocol, morphine consumption at postoperative days 1–3 was significantly less is the group receiving COX-2 inhibitors. These patients had faster return of gastrointestinal function and shorter hospital stays overall (10). These benefits may translate to patients undergoing other surgeries as well.
Intraoperative management of these patients generally begins with a standard induction using propofol and an inhaled anesthetic. Ketamine may also be used at induction as well. Ketamine is a NMDA receptor antagonist that decreases opioid consumption by decreasing central excitability and possibly modulates opioid receptors. It has been shown to be effective when used as a sole agent, or in conjunction with opioids, NSAIDs, and acetaminophen (11). Ketamine usage intraoperatively decreases opioid consumption postoperatively, and has the potential to decrease pain scores several weeks to months after surgery (12). Liberal use of local anesthetic by the surgeon is also recommended prior to surgical incision, and dexamethasone and famotidine are often administered to preemptively decrease nausea and vomiting.
Dexamethasone is also associated with reduction in pain scores during mobilization postoperatively. As part of a multimodal analgesia plan, high-dose dexamethasone (more than 0.2 mg/kg) was found to have opioid sparing effects (13). It has also been shown to delay time to first postoperative analgesic intake when used in conjunction with peripheral nerve blocks (14). Small doses of fentanyl (totaling 1–2 mcg/kg) can be administered throughout the operation. Methadone is also being considered for use in MMA. Methadone has a longer half-life than other opioids, while also inhibiting NMDA receptors and inhibiting the uptake of serotonin and norepinephrine. This can inhibit the development of opioid tolerance and may play a role in mood elevation (15). When compared to patients receiving IV hydromorphone, patient receiving methadone had fewer postoperative opioid requirements and improved pain scores. Optimal use and dosing of methadone remains to be determined.
Intravenous lidocaine can also play a role in multimodal analgesia. In a study of patients undergoing complex spine surgery, patients who received 2 mg/kg/h of IV lidocaine had lower pain scores. They also had slightly fewer complications at 30 days post operatively (16). They also had lower opioid requirements but this difference was not statistically significant. This may be due to the type of pain experienced after spine surgery (vs. abdominal surgery where it has shown to be effective). Prior to extubation, most MMA protocols recommend administration of intravenous acetaminophen.
Acetaminophen has analgesic and antipyretic effects by acting as a reducing agent to prevent a secondary peroxidase step involved in prostaglandin synthesis by the cyclooxygenase enzymes. Intravenous administration provides rapid onset of pain relief, within 25 min, and is associated with decreased time to extubation, shorter intermediate stays, and shorter hospitalization overall in surgical patients (17). Though it has not consistently been shown to decrease opioid requirements, acetaminophen does improve pain scores post operatively and it’s utility as a part of ERAS protocols for spine surgery remains under investigation (18).
There are several options for regional anesthetics to be incorporated into any MMA plan for spine surgery. In a small study, a single shot epidural injection of local anesthetic was found to decrease opioid requirements in the postoperative setting (19). Erector spinae plane blocks and continuous infusion catheters anesthetize the dorsal and ventral rami of spinal nerves and can also be used as a part of MMA protocols for various spine procedures (20). Patients receiving these blocks achieved adequate pain control with little or no opioid consumption, and did not have any issues with neuromonitoring during their procedures (21). A retrospective study of pediatric spinal fusion surgery patients showed that opioid usage was significantly less in patients receiving continuous infusion of local anesthetic into the surgical site via elastomeric pain pump (22). There are case reports of lumbar spine surgery being performed under spinal or epidural anesthesia exclusively (23,24). Benefits include reduction in post-op pain and decreased incidence of PONV, but this requires more cooperation on the part of the patient, the anesthesiologist, and the surgeon. Epidural anesthesia may blunt the surgical stress response after major surgery (25).
Postoperative management of patients after spine surgery using multimodal anesthesia involves continuation of the preoperative medications (muscle relaxant, opioid, anticonvulsant) with the possible addition of scheduled NSAIDs and/or acetaminophen. Gabapentin and pregabalin have been found to be effective in reducing opioid use in the immediate postoperative setting (26). Though the ideal dosing of each is actively under investigation, there is evidence to support that pregabalin 150 mg is superior to pregabalin 75 mg given preoperatively and at 12 hours post-surgery in reducing postoperative opioid consumption (27). Gabapentin also has a dose dependent effect, with a dose of 600 mg given preoperatively superior to 300 mg in reducing pain scores and fentanyl consumption for 24 hours postoperatively, but escalating doses beyond 600 mg did not further reduce pain or opioid consumption (28). Gabapentin administration is also associated with an increased risk of sedation, but a reduced incidence of nausea, vomiting, and pruritus compared to opioids (29). Tramadol, a weak µ-opioid receptor agonist also has analgesic activity due to serotonin-norepinephrine inhibitor activity, may be given postoperatively in place of more potent opioids such as hydrocodone or oxycodone (30). The use of ice packs can be incorporated into the post-operative portion of any MMA protocol. Though there is no specific data to support this therapy in spine surgery patients specifically, a randomized control trial of postpartum patients with perineal pain showed a greater than 30% reduction in pain for a significant number of patients for up to two hours after an ice pack was applied for ten minutes (31).
Postoperative pain can be a significant source of stress, anxiety, depression, and can be a precursor to the development of chronic pain (32). Multimodal anesthesia protocols have become commonplace in today’s landscape of spinal surgery because they have consistently shown a decrease in opioid consumption and improvement in postoperative mobilization while also improving issues with postoperative nausea, vomiting, and sedation (33). Pain scores assessed immediately postop and in the days following surgery are consistently lower in patients receiving multimodal anesthesia versus opioids alone (21). What remains to be investigated are the more long term implications of these protocols (34). Though the classes of medications used have been well described, the exact dosages used still vary, and these nuances may lead to significant differences in 30–90 days outcomes, complication rates, and readmission rates.
Implementing a MMA
Successful implementation of a MMA requires the input and cooperation of all of the stakeholders including the caregivers as well as the patients. Discussions regarding the plan for pain management should begin in the outpatient setting when the patient’s surgery is scheduled and consent is obtained (35). The surgeon’s office is an ideal location to begin these discussions as the patient is more relaxed. In addition to the intraoperative anesthesia, this discussion should include the proposed postoperative analgesic management strategy. The role and importance of each of the medication as well as the overall approach to the multimodal management can be discussed and the patient can be allowed to ask questions. Patients’ expectations should be discussed as should the plan to minimize opioid use postoperatively, the importance of the non-opioid adjuvant therapy and the patient’s role and agreement with the MMA approach.
A preoperative evaluation by the anesthesiologist, ideally through the preoperative clinic should be encouraged for patients that may be difficult to manage using the standard MMA protocol. This is especially important for chronic pain patients who may already be taking high doses of opioids. These patients often have additional risk factors for increased postoperative pain such as increased anxiety, depression, and tobacco/drug/alcohol use, which also increase their risk of long-term opioid use postoperatively (36,37). While beneficial for all patients, the importance of multimodal anesthesia is especially highlighted in patients who may be susceptible to opioid related adverse effects, such as patients with obstructive sleep apnea (38). Health system benefits can also be realized from the implementation of an effective MMA, as fewer opioid related side effects can improve patient recovery and lead to faster discharge and improved utilization of resources.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Sharma S, Balireddy RK, Vorenkamp KE, et al. Beyond opioid patient-controlled analgesia: a systematic review of analgesia after major spine surgery. Reg Anesth Pain Med 2012;37:79-98. [Crossref] [PubMed]
- Rajpal S, Gordon DB, Pellino TA, et al. Comparison of perioperative oral multimodal analgesia versus IV PCA for spine surgery. J Spinal Disord Tech 2010;23:139-45. [Crossref] [PubMed]
- Bohl DD, Louie PK, Shah N, et al. Multimodal versus patient-controlled analgesia after an anterior cervical decompression and fusion. Spine (Phila Pa 1976) 2016;41:994-8. [Crossref] [PubMed]
- van Tulder M, Becker A, Bekkering T, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15 Suppl 2:S169-91. [Crossref] [PubMed]
- Friedman B, Dym AA, Davitt M, et al. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain. JAMA 2015;314:1572-80. [Crossref] [PubMed]
- Tiippana EM, Hamunen K, Kontinen VK, et al. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg 2007;104:1545-56. [Crossref] [PubMed]
- Li J, Ajiboye RM, Orden MH, et al. The effect of ketorolac on thoracolumbar posterolateral fusion: a systematic review and meta-analysis. Clin Spine Surg 2018;31:65-72. [Crossref] [PubMed]
- Raja D, Shetty A, Subramanian B, et al. A prospective randomized study to analyze the efficacy of balanced pre-emptive analgesia in spine surgery. Spine J 2019;19:569-77. [Crossref] [PubMed]
- Garcia RM, Cassinelli EH, Messerschmitt PJ, et al. A multimodal approach for postoperative pain management after lumbar decompression surgery: a prospective, randomized study. J Spinal Disord Tech 2013;26:291-7. [Crossref] [PubMed]
- Lohsiriwat V. Opioid-sparing effect of selective cyclooxygenase-2 inhibitors on surgical outcomes after open colorectal surgery within an enhanced recovery after surgery protocol. World J Gastrointest Oncol 2016;8:543-9. [Crossref] [PubMed]
- Loftus RW, Yeager MP, Clark JA, et al. Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. Anesthesiology 2010;113:639-46. [PubMed]
- Young A, Buvanendran A. Recent advances in multimodal analgesia. Anesthesiol Clin 2012;30:91-100. [Crossref] [PubMed]
- De Oliveira G, Almeida M, Benzon H, et al. Perioperative Single Dose Systemic Dexamethasone for Postoperative Pain: A Meta-analysis of Randomized Control Trials. Anesthesiology 2011;115:575-88. [Crossref] [PubMed]
- Clement JC, Besch G, Puyraveau M, et al. Clinical Effectiveness of single dose of intravenous dexamethasone on the duration of ropivacaine axillary brachial plexus block: the randomized placebo-controlled ADEXA trial. Reg Anesth Pain Med 2019;44:370-4. [Crossref] [PubMed]
- Murphy GS, Szokol JW, Avram MJ, et al. Clinical effectiveness and safety of intraoperative methadone in patients undergoing posterior spinal fusion surgery: A randomized, double-blinded, controlled trial. Anesthesiology 2017;126:822-33. [Crossref] [PubMed]
- Farag E, Ghobrial M, Sessler D, et al. Effect of perioperative intravenous lidocaine administration on pain, opioid consumption, and quality of life after complex spine surgery. Anesthesiology 2013;119:932-40. [Crossref] [PubMed]
- Hansen RN, Pham AT, Böing EA, et al. Comparative analysis of length of stay, hospitalization costs, opioid use, and discharge status among spine surgery patients with postoperative pain management including intravenous versus oral acetaminophen. Curr Med Res Opin 2017;33:943-8. [Crossref] [PubMed]
- Mörwald EE, Poeran J, Zubizarreta N, et al. Intravenous acetaminophen does not reduce inpatient opioid prescription of opioid-related adverse events among patients undergoing spine surgery. Anesth Analg 2018;127:1221-8. [Crossref] [PubMed]
- Thepsoparn M, Sereeyotin J, Pannangpetch P. Effects of combined lower thoracic epidural/general anesthesia on pain control in patients undergoing elective lumbar spine surgery: a randomized controlled trial. Spine (Phila Pa 1976) 2018;43:1381-5. [PubMed]
- Chin KJ, Lewis S. Opioid-free analgesia for posterior spinal fusion surgery using erector spinae plane (ESP) blocks in a multimodal anesthetic regimen. Spine (Phila Pa 1976) 2019;44:E379-83. [Crossref] [PubMed]
- Melvin JP, Schrot RJ, Chu GM, et al. Low thoracic erector spinae plane block for perioperative analgesia in lumbosacral spine surgery: a case series. Can J Anaesth 2018;65:1057-65. [Crossref] [PubMed]
- Reynolds RA, Legakis JE, Tweedie J, et al. Postoperative pain management after spinal fusion surgery: an analysis of the efficacy of continuous infusion of local anesthetics. Global Spine J 2013;3:7-14. [Crossref] [PubMed]
- Ulutas M, Secer M, Taskapilioglu O, et al. General versus epidural anesthesia for lumbar microdiscectomy. J Clin Neurosci 2015;22:1309-13. [Crossref] [PubMed]
- Yilmaz C, Buyrukcu SO, Cansever T, et al. Lumbar microdiscectomy with spinal anesthesia: comparison of prone and knee-chest positions in means of hemodynamic and respiratory function. Spine (Phila Pa 1976) 2010;35:1176-84. [Crossref] [PubMed]
- Ezhevskaya AA, Mlyavykh SG, Anderson DG. Effects of continuous epidural anesthesia and postoperative epidural analgesia on pain management and stress response in patients undergoing major spinal surgery. Spine (Phila Pa 1976) 2013;38:1324-30. [Crossref] [PubMed]
- Schmidt PC, Ruchelli G, Mackey SC, et al. Perioperative gabapentinoids: choice of agent, dose, timing, and effects on chronic postsurgical pain. Anesthesiology 2013;119:1215-21. [Crossref] [PubMed]
- Kim JC, Choi YS, Kim KN, et al. Effective dose of peri-operative oral pregabalin as an adjunct to multimodal analgesic regimen in lumbar spinal fusion surgery. Spine (Phila Pa 1976) 2011;36:428-33. [Crossref] [PubMed]
- Pandey CK, Navkar DV, Giri PJ, et al. Evaluation of the optimal preemptive dose of gabapentin for postoperative pain relief after lumbar diskectomy: A randomized double-blind, placebo-controlled study. J Neurosurg Anesthesiol 2005;17:65-8. [Crossref] [PubMed]
- Ho KY, Gan TJ, Habib AS. Gabapentin and postoperative pain -- A systematic review of randomized controlled trials. Pain 2006;126:91-101. [Crossref] [PubMed]
- Terracina S, Robba C, Prete A, et al. Prevention and treatment of postoperative pain after lumbar spine procedures: A systematic review. Pain Pract 2018;18:925-45. [Crossref] [PubMed]
- Francisco AA, De Oliveira SM, Steen M, et al. Ice pack induced perineal analgesia after spontaneous vaginal birth: randomized control trial. Women Birth 2018;31:e334-40. [Crossref] [PubMed]
- MacLachlan C, Shipton EA, Wells JE. Perioperative pain correlates and prolonged postoperative pain predictors: Demographic and psychometric questionnaires. Pain Ther 2015;4:119-33. [Crossref] [PubMed]
- Mathiesen O, Dahl B, Thomsen BA, et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J 2013;22:2089-96. [Crossref] [PubMed]
- Grasu RM, Cata JP, Dang AQ, et al. Implementation of an Enhanced Recovery After Spine Surgery program at a large cancer center: a preliminary analysis. J Neurosurg Spine 2018;29:588-98. [Crossref] [PubMed]
- Singh K, Bohl DD, Ahn J, et al. Multimodal analgesia versus intravenous patient-controlled analgesia for minimally invasive transforaminal lumbar interbody fusion procedures. Spine (Phila Pa 1976) 2017;42:1145-50. [Crossref] [PubMed]
- Jain N, Phillips FM, Weaver T, et al. Preoperative chronic opioid therapy: a risk factor for complications, readmission, continued opioid use and increased costs after one- and two-level posterior lumbar fusion. Spine (Phila Pa 1976) 2018;43:1331-8. [Crossref] [PubMed]
- Jain N, Brock JL, Phillips FM, et al. Chronic preoperative opioid use is a risk factor for increased complications, resource use, and costs after cervical fusion. Spine J. 2018;18:1989-98. [Crossref] [PubMed]
- Buvanendran A, Thillainathan V. Preoperative and postoperative anesthetic and analgesic techniques for minimally invasive surgery of the spine. Spine (Phila Pa 1976) 2010;35:S274-80. [Crossref] [PubMed]


