Current trends in ambulatory spine surgery: a systematic review
Introduction
Spine surgery has been gradually moving out of the inpatient setting and into ambulatory surgery centers (ASC). This change has been in response to decreasing invasiveness of surgery, patients’ desire to recuperate at home, and significant net reductions in cost, which is critical in this era of value-based care (1,2). With this ongoing transition from hospital-based to standalone ASC-based spine surgery, careful attention should be paid to the evolving body of literature regarding spine surgery in this setting, specifically its safety, outcomes, protocols, and cost implications. The purpose of this article is to perform a systematic review of literature published within the past five years to report the most up-to-date evidence regarding safety and utilization trends in ambulatory spine surgery.
Methods
A systematic review was conducted on currently available literature regarding ambulatory spine surgery according to PRISMA guidelines (3). A search of PubMed was performed using the query terms (“spine surgery” or “spinal surgery”) and (“ambulatory” or “outpatient”) within the title of the article. All titles greater than 5 years from the search date (January 6, 2019) were excluded in order to maintain a focus on current literature. Studies in languages other than English were excluded. The remaining articles were reviewed in their entirety by the lead author (EM DelSole), and the individual article bibliographies were screened for additional relevant studies. Articles were evaluated for relevance to ambulatory or outpatient spine surgery, and subsequently excluded if the search result was determined to be irrelevant to the topic. All studies were evaluated by study design and level of evidence was determined. Articles with unclear or uninterpretable methodologies were excluded.
Results
A total of 56 articles published between January 6, 2014 and January 6, 2019 (the date of the database query) were identified and considered for review. Two studies were excluded because they were written in a language other than English. From the remaining 54 studies, 36 were excluded because they lacked relevance to the topic of current trends in ambulatory spine surgery. Two articles were excluded due to lack of clear study methodology and data analysis. Following exclusion, 16 studies were available for review. Ten additional studies were identified from review of bibliographies and included in this review, making a total of 26 articles.
Quality of the current literature
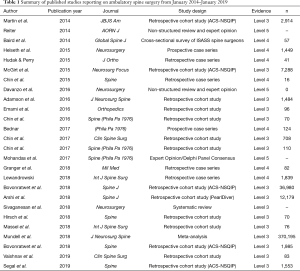
With respect to level of evidence, this systematic review yielded 16 level III, seven level IV, and three level V studies (Table 1) (4). This is consistent with prior reviews of ambulatory spine surgery literature, with no level I or II studies available in the English language (5).
Full table
Clinical practice trends in ambulatory spine surgery
The utilization of outpatient spine surgery appears to be increasing. This systematic review identified nine articles discussing ambulatory anterior cervical discectomy and fusion (ACDF), seven discussing lumbar decompression, four discussing posterior lumbar fusion, one discussing lateral lumbar interbody fusions, and three discussing cervical disc replacement. Baird et al. conducted a cross-sectional survey of spine surgeons practicing in the United States and found that 84.2% performed ambulatory surgery in some capacity, with nearly 50% of the surgeons surveyed reporting they were investors in an ASC (6).
Best et al. evaluated national trends in ambulatory spine surgery via a retrospective analysis of the Centers for Disease Control and Prevention (CDC)’s national survey of ambulatory surgery. They noted substantial increases in ambulatory surgery utilization from 1994–2006 (7). Specifically, outpatient surgery for intervertebral disc disorders increased by 340% during that time, and surgeries for spinal stenosis increased by more than 2,000% during that same period. Similarly, Arshi et al. noted an increase in the annual relative incidence of outpatient ACDF from 0.11 in 2011 to 0.22 in 2016 in a study of patients in the PearlDiver database (8).
Patient selection
Three manuscripts explicitly commented on patient selection for ambulatory surgery. Commonly considered selection criteria include American Society of Anesthesiologists (ASA) Score, body mass index (BMI), cardiac risk, opioid dependency, and psychosocial factors including the existence of a reliable support system (9). Mohandas et al. utilized a Delphi panel to define consensus statements on safe patient selection and preoperative assessment for ambulatory spine surgery (10). The panel consisted of spine surgeons, anesthesiologists, and one registered nurse, and consensus was set at >70% agreement. The authors were able to achieve consensus on 22 variables for optimizing patient selection for outpatient surgery. Chin et al. described a list of eligibility criteria for a single private practice (11). In this practice and using these criteria, 79% of patients were eligible for an ambulatory procedure. The authors’ proposed inclusion criteria for outpatient spine surgery are reported in Table 2. If these numbers were reproducible on a national scale, the result could be substantial cost reductions related to inpatient hospital stay.

Full table
Cost savings
Cost savings is a critical component of the value equation and should be continually evaluated as payors alter reimbursements to facilities providing these services. ASC utilization has demonstrated measurable decreases in cost, however one confounding factor in that determination is selection bias of healthier patients into the ASC, with the more medically complex patients undergoing surgery in the traditional hospital setting. This finding, of course, could account for greater expense. Mundell et al. sought to evaluate the influence of patient selection on the perceived cost savings of ASC use compared to hospital-based surgery (12). The authors performed a meta-analysis of 16 level III studies and 370,195 patients undergoing spine surgery (ACDF and lumbar decompression). The meta-analysis data demonstrated that outpatient operations were associated with significantly lower reoperations, readmissions, and costs of care. However, when stratifying the results by age, the direct cost savings for younger patients was substantially less than for older patients ($555 vs. $7,290, respectively). Because younger patients are more likely to be in good health, the authors inferred that cost savings in older patients may be the result of selection of healthier patients for outpatient operations. While beyond the scope of this review, it is important to note the distinction between outpatient surgery at ASCs versus hospital outpatient departments (HOPD), namely in terms of healthcare cost. ASC payments are typically 50–60% of that at HOPDs, providing savings for both patients and the healthcare system (13).
Narcotic consumption
Postoperative consumption of opioid pain medication has been of particular concern due to the risk of dependence and adverse outcomes, specifically physical dependence, delirium, respiratory depression, constipation and urinary retention, and even increases in length of hospital stay (LOS) (14-16). Massel et al. compared postoperative opioid analgesia between ASC-based ACDF and hospital-based ACDF (16,17). The authors found that the hospital-based cohort had significantly greater hourly and long-term opioid medication consumption compared with those having surgery at the ASC. Contributing to this finding was that on average, hospital patients consumed greater average doses of fentanyl and oxycodone. Despite receiving lower opioid doses overall, the ASC patients achieved similar pain outcomes postoperatively. The statistical analysis suggested that these outcomes were connected with length of stay. As such, outpatient surgery represents an opportunity to modify perioperative analgesia and limit postoperative opioid use.
Hirsch et al. evaluated hourly oral morphine equivalents consumed by patients undergoing revision lumbar decompression surgery in either an ASC or traditional hospital setting (18). The authors found a non-significant trend toward greater morphine consumption among hospital-based patients. However, it is unclear if the study was adequately powered to detect this difference.
Clinical outcomes & safety profile
The majority of literature in the past five years has focused on the feasibility of performing outpatient spine surgery, specifically ensuring that it can be done safely and that clinical outcomes are non-inferior to hospital-based historical standards. Definitions of safety must be determined by the surgical team, but general principles of safe outpatient surgery should include similar complication rate and profile, that complications can be appropriately managed in a timely fashion, and that the resources exist to address the complications appropriately.
Helseth et al. reported on the results of a 1,449 patients case series of lumbar decompressions and ACDFs (19). The overall complication rate was 3.5%, which is lower than other reported complication rates in spine surgery (20). In their experience, 99.8% of patients were successfully discharged on the day of surgery. The remaining 0.2% patients (3 patients total) were admitted for the following reasons: one ACDF patient with unilateral arm hemiparesis necessitating cerebrovascular event workup (workup resulted as negative), one ACDF patient with unilateral hemiparesis necessitating cerebrovascular event workup which demonstrated right cerebral infarction, and one single-level lumbar decompression patient with a postoperative symptomatic retroperitoneal hematoma. Beyond this, 22 patients (1.5%) required hospital admission within the first 90-day postoperatively for issues related to pain, infection, CSF leak, hematoma, dysphagia, vocal issues/recurrent laryngeal nerve palsy. It is important to note the authors’ careful attention to developing a postoperative protocol centered around patient optimization and safety, including the ability for patients to call an on-call neurosurgeon directly 24 h per day, 7 days per week following their operation. However, this article received criticism due to its lack of control group and its limited statistical methodology (21).
Martin et al. evaluated the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) to determine the risks of complication following elective single-level ACDF in the inpatient and outpatient setting (22). The authors found a 3.2% overall incidence of complications, with risk factors including patient age >65 years, BMI >30 kg/m2, American Society of Anesthesiologists class 3 or 4, concurrent dialysis requirement, concurrent corticosteroid use, recent sepsis, and surgical time >120 min. Analysis comparing inpatient and outpatient complications revealed that outpatient treatment was not a risk factor for complications.
Hudak and Perry evaluated a case series of 41 consecutive patients who were diagnosed as obese by BMI ≥30 undergoing outpatient endoscopic lumbar decompression. Their primary outcomes were postoperative decreases in visual analog pain (VAS) leg and Oswestry disability index (ODI), with secondary outcomes being rates of complication, blood losses, and length of surgery (23). The authors found that endoscopic decompression resulted in significant pain relief with minimal blood loss and no complications. Lewandrowski also reported the outcomes in a series of patients undergoing endoscopic transforaminal lumbar decompressive surgery in an ASC (24). With respect to clinical outcomes, the authors reported good or excellent results in 72% of patients with contained disc herniations, 75% of patients with bony central stenosis, and 83% of patients with extruded disc fragments. Complications were rare at a rate of 0.86%, and included leg dysesthesias, wound infections, and poor pain control.
Revision surgery represents another challenge due to its sometimes more complex nature than primary surgical procedures. Hirsch et al. evaluated the safety of revision lumbar decompression performed in an ASC (18). They found that patients who underwent surgery in the ASC had significantly decreased length of stay (2.7 vs. 11 h, P<0.001). The only complication reported from either cohort was a superficial infection occurring in one patient from the ASC, which was treated with oral antibiotics.
Bovonratwet et al. compared perioperative complications in inpatient and outpatient lumbar posterolateral fusion (PLF) using data from the ACS-NSQIP from 2005–2015 (25). After propensity score matching to control for confounders, they found no difference in postoperative adverse events between groups. Additionally, there was no difference in 30-day readmission rates. The authors did, however, identify a significant reduction in the number of blood transfusions performed in the outpatient group, which could translate into reductions in complications and cost.
Emami et al. compared the outcomes of patients undergoing minimally invasive transforaminal lumbar interbody fusion (TLIF) in an ASC and an inpatient hospital setting (26). Notably, the outpatient group was significantly younger than the inpatient group and had lower ASA scores. They authors noted no difference in postoperative complication rates, hospital readmission rates, or clinical outcomes according to ODI and VAS score at two-years follow-up.
Chin et al. performed a retrospective comparative study of 70 consecutive patients who underwent lateral lumbar interbody fusion (40 inpatients and 30 outpatients treated in an ASC) (27). The indication for surgery was chronic low back pain without radiculopathy having failed conservative therapy. The authors found that postoperative ODI remained unchanged for inpatients, whereas it decreased for outpatients in the ASC. Both groups experienced improvements in VAS back pain score, however, there was no difference based upon the location of surgery.
Granger et al. evaluated a series of active-duty military patients undergoing outpatient minimally invasive lumbar decompression surgery for radiculopathy or spinal stenosis (28). All surgeries were performed in an ASC. At one year after surgery, there were significant reductions in self-reported pain and disability compared with preoperatively. Within three months, all active servicemen had returned to duty. The mean surgical time was 62 min, with a mean blood loss of 30.6 mL.
The historical literature at present suggests that ACDF is considered a safe outpatient procedure (29). The majority of current literature is in line with this observation. Chin et al. report a clinical case series of 16 consecutive patients who underwent single-level posterior lumbar interbody fusion in an ASC (30). Final postoperative follow-up ranged from 5–32 months. The authors found that patients had statistically significant reductions in VAS back pain and ODI after surgery. The authors did not report on 30-day readmissions.
Adamson et al. retrospectively evaluated 1,000 consecutive one- and two-level ACDF performed in an outpatient ASC compared with 484 performed in a traditional hospital (31). When comparing the two groups, LOS was greater when ACDF was performed within the hospital. There were no differences in 90-day surgical morbidity and mortality between the inpatient and outpatient groups for one- and two-level operations, with the exception of postoperative dysphagia, which appeared to occur more frequently after surgery in the ASC.
McGirt et al. evaluated the available ACS-NSQIP data for patients undergoing inpatient and outpatient ACDF from 2005–2011, focusing on 30-day morbidity and mortality rates (32). They found significantly decreased rates of morbidity and 30-day reoperation rate among patients having surgery at an ASC. These findings remained significant after controlling for confounders by propensity score matching and logistic regression analysis.
Khanna et al. performed a follow up study using the ACS-NSQIP data from 2011–2013 evaluating rates of complication, reoperation, readmission, and mortality among both inpatient and outpatient ACDF (33). They found the improved perioperative safety outcomes reported by McGirt were sustained through this time period (32).
Vaishnav et al. compared clinical outcomes and safety for patients undergoing 2-level ACDF in the ASC and hospital setting (34). Patients undergoing surgery in the ASC were found to have lower BMI and lower ASA scores. No patients in the ASC group required hospitalization or reintubation postoperatively. They found no difference in 6- or 12-month patient-reported outcomes.
Chin et al. compared the safety of outpatient cervical total disc replacement (TDR) with ACDF (35). The authors found no difference in the groups with respect to perioperative complications and clinical outcomes at two years follow-up. Two additional studies have looked at clinical outcomes and safety of cervical disc arthroplasty (CDA) in the outpatient setting. Using the NSQIP database, studies from Segal et al. and Bovonratwet et al. found no difference in reoperation, readmission and complication rates at 30 days between outpatient and inpatient CDRs (36,37).
However, not all data on outpatient anterior cervical surgery is positive. Arshi et al. evaluated the Humana PearlDiver database and compared complication and reoperation rates among 1- or 2-level ACDF performed as an outpatient or an inpatient procedure (8). They reported that outpatient operations were more likely to undergo revision ACDF or posterior cervical decompression and fusion (PCDF) at both the 6- and 12-month time points. Among medical complications, acute renal failure was more commonly associated with outpatient ACDF than for those who underwent an inpatient procedure.
Financial conflicts
Baird et al. noted that surgeon investors are more likely to attempt more complex cases in ASCs than non-investors (6). The obvious concern in this situation is the risk that financial incentives are driving increased risk-taking in the ASC environment.
Consensus on best practices & care protocols
Two manuscripts focused on consensus opinion of the existing literature for determining clinical best practices when transitioning surgeries to the outpatient setting (10,38). Notably, nursing leadership has also taken the lead in optimizing ambulatory spine surgery by working to develop best practices for patient education for those undergoing outpatient procedures (38). While this represents level V evidence, the author does advocate for individualized patient assessment to optimize the perioperative process, postoperative recovery, and the overall patient outcome. Similar expert opinion was generated from the previously mentioned Delphi panel published by Mohandas et al. (10).
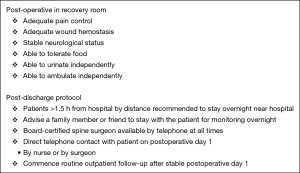
Two manuscripts describe in detail postoperative care protocols, which appear critical for success when discharging patients on the same day following a spine operation. Bednar et al. described a strict postoperative protocol for optimizing postoperative lumbar decompressions and fusions to be discharged the morning after surgery (39). With use of the protocol, the author achieved discharge of 122/124 patients the morning after surgery, with 2 men with a history of prostatic hyperplasia requiring admission for urinary retention. Interestingly the postoperative protocol described by Bednar et al. utilized opioid pain management only. Helseth et al. also described the postoperative protocol used for ambulatory spine surgery, which included a defined period of postoperative observation (6 h for cervical, 3 h for lumbar), mobilization in the recovery room, and implementation of a postoperative checklist that must be fully satisfied before discharge (Figure 1) (19).
All four of these articles describe strict inclusion and exclusion criteria for performing outpatient spine operations. While the criteria did vary among the authors, in general there appeared to be agreement on selecting patients with ASA class I and II, Age <70 years, and appropriate surgical load (one- or two-level operations, limited fusions).
Discussion
This systematic review demonstrates the current literature has a specific focus on understanding the safety and efficacy of outpatient spine surgery in an effort to improve patient outcomes and demonstrate a net gain in value to payors. The data presented suggest that ACDF, lumbar decompression, single-level lumbar fusions, minimally invasive surgery (MIS) TLIF, and lateral lumbar interbody fusion (LLIF) can all be performed safely in an ambulatory setting with patients discharged the same day with little reported risk of complication. It is critical to note, however, that patient selection is paramount in order to optimize outcomes and safe delivery of care. Emphasis has been placed upon postoperative protocols to prevent catastrophic complications such as airway compromise or postoperative hematomas with neurologic loss. With organized planning and anticipation of complications, comparable outcomes to inpatient surgery have been achieved.
The literature, however, does deserve criticism for generally low evidence levels. There are currently no level I or II studies available for interpretation. This limits our capacity for inference and generalizability. At this time, there is no consensus on patient selection, case complexity thresholds, and optimal postoperative protocols to maximize safety and clinical outcomes. Similarly, there is little explicit data across all studies presented on postoperative readmissions and ASC to hospital transfers. Further complicating the issue is that the term “outpatient” or “ambulatory” can hold multiple meanings depending on the state in which surgery is performed; more specifically, there is no distinction between patients sent home the same calendar day versus those who are kept for 23-hour observation. Current and future research should strive for clarity of these terms in order to ensure generalizability of results and provide a clearer picture of the safety and efficacy of ambulatory spine surgery.
Conclusions
Ambulatory spine surgery represents an opportunity to optimize the healthcare value equation. Patients undergoing outpatient surgery should be carefully selected and postoperative protocols should be established to maintain a safe perioperative experience. Further research of higher quality is needed to determine optimal patient and case complexity for this environment.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gray DT, Deyo RA, Kreuter W, et al. Population-Based Trends in Volumes and Rates of Ambulatory Lumbar Spine Surgery. Spine 2006;31:1957-63. [Crossref] [PubMed]
- Fabricant PD, Seeley MA, Rozell JC, et al. Cost Savings From Utilization of an Ambulatory Surgery Center for Orthopaedic Day Surgery. J Am Acad Orthop Surg 2016;24:865-71. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J Clin Epidemiol 2009;62:1006-12. [Crossref] [PubMed]
- Marx RG, Wilson SM, Swiontkowski MF. Updating the assignment of levels of evidence. J Bone Joint Surg Am 2014;97:1-2. [Crossref] [PubMed]
- Sivaganesan A, Hirsch B, Phillips FM, et al. Spine Surgery in the Ambulatory Surgery Center Setting: Value-Based Advancement or Safety Liability? Neurosurgery 2018;83:159-65. [Crossref] [PubMed]
- Baird EO, Brietzke SC, Weinberg AD, et al. Ambulatory spine surgery: a survey study. Global Spine J 2014;4:157-60. [Crossref] [PubMed]
- Best MJ, Buller LT, Eismont FJ. National Trends in Ambulatory Surgery for Intervertebral Disc Disorders and Spinal Stenosis: A 12-Year Analysis of the National Surveys of Ambulatory Surgery. Spine 2015;40:1703-11. [Crossref] [PubMed]
- Arshi A, Wang C, Park HY, et al. Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision surgery and perioperative complications: an analysis of a large nationwide database. Spine J 2018;18:1180-7. [Crossref] [PubMed]
- Sayari AJ, Hirsch BP. Case selection for spine surgery in the ambulatory setting. Semin Spine Surg 2018;30:142-7. [Crossref]
- Mohandas A, Summa C, Worthington WB, et al. Best Practices for Outpatient Anterior Cervical Surgery: Results From a Delphi Panel. Spine (Phila Pa 1976) 2017;42:E648-59. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Coombs AV, et al. Eligibility of Outpatient Spine Surgery Candidates in a Single Private Practice. Clin Spine Surg 2017;30:E1352-8. [Crossref] [PubMed]
- Mundell BF, Gates MJ, Kerezoudis P, et al. Does patient selection account for the perceived cost savings in outpatient spine surgery? A meta-analysis of current evidence and analysis from an administrative database. J Neurosurg Spine 2018;29:687-95. [Crossref] [PubMed]
- Kurd MF, Schroeder GD, Vaccaro AR. Spine Surgery in an Ambulatory Setting: What Can Be Done Safely? JBJS Rev 2015. [Crossref] [PubMed]
- Rodgers J, Cunningham K, Fitzgerald K, et al. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am 2012;37:645-50. [Crossref] [PubMed]
- Walid MS, Hyer L, Ajjan M, et al. Prevalence of opioid dependence in spine surgery patients and correlation with length of stay. J Opioid Manag 2007;3:127-8, 130-2. [Crossref] [PubMed]
- Hyer LA, Walid MS, Brooks AM, et al. Interaction of age and opioid dependence on length of hospital stay for spine surgery patients. Psychol Rep 2009;105:361-4. [Crossref] [PubMed]
- Massel DH, Narain AS, Hijji FY, et al. A Comparison of Narcotic Consumption Between Hospital and Ambulatory-Based Surgery Centers Following Anterior Cervical Discectomy and Fusion. Int J Spine Surg 2018;12:595-602. [Crossref] [PubMed]
- Hirsch BP, Khechen B, Patel DV, et al. Safety and Efficacy of Revision Minimally Invasive Lumbar Decompression in the Ambulatory Setting. Spine (Phila Pa 1976) 2019;44:E494-9. [Crossref] [PubMed]
- Helseth Ø, Lied B, Halvorsen CM, et al. Outpatient Cervical and Lumbar Spine Surgery is Feasible and Safe: A Consecutive Single Center Series of 1449 Patients. Neurosurgery 2015;76:728-37. [Crossref] [PubMed]
- Dekutoski MB, Norvell DC, Dettori JR, et al. Surgeon perceptions and reported complications in spine surgery. Spine (Phila Pa 1976) 2010;35:S9-21. [Crossref] [PubMed]
- Davanzo J, Lane J, Daggubati L, et al. Journal Club: Outpatient Cervical and Lumbar Spine Surgery Is Feasible and Safe: A Consecutive Single Center Series of 1449 Patients. Neurosurgery 2016;79:765-7. [Crossref] [PubMed]
- Martin CT, Pugely AJ, Gao Y, et al. Thirty-Day Morbidity After Single-Level Anterior Cervical Discectomy and Fusion: Identification of Risk Factors and Emphasis on the Safety of Outpatient Procedures. J Bone Joint Surg Am 2014;96:1288-94. [Crossref] [PubMed]
- Hudak EM, Perry MW. Outpatient minimally invasive spine surgery using endoscopy for the treatment of lumbar spinal stenosis among obese patients. J Orthop 2015;12:156-9. [Crossref] [PubMed]
- Lewandrowski KU. Readmissions After Outpatient Transforaminal Decompression for Lumbar Foraminal and Lateral Recess Stenosis. Int J Spine Surg 2018;12:342-51. [Crossref] [PubMed]
- Bovonratwet P, Ottesen TD, Gala RJ, et al. Outpatient elective posterior lumbar fusions appear to be safely considered for appropriately selected patients. Spine J 2018;18:1188-96. [Crossref] [PubMed]
- Emami A, Faloon M, Issa K, et al. Minimally Invasive Transforaminal Lumbar Interbody Fusion in the Outpatient Setting. Orthopedics 2016;39:e1218-22. [Crossref] [PubMed]
- Chin KR, Pencle FJ, Coombs AV, et al. Lateral Lumbar Interbody Fusion in Ambulatory Surgery Centers: Patient Selection and Outcome Measures Compared With an Inhospital Cohort. Spine (Phila Pa 1976) 2016;41:686-92. [Crossref] [PubMed]
- Granger E, Prada S, Bereczki Z, et al. Return-to-Duty Rates Following Minimally Invasive Spine Surgery Performed on Active Duty Military Patients in an Ambulatory Surgery Center. Mil Med 2018;183:e619-23. [Crossref] [PubMed]
- Villavicencio AT, Pushchak E, Burneikiene S, et al. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine J 2007;7:148-53. [Crossref] [PubMed]
- Chin KR, Coombs AV, Seale JA. Feasibility and Patient-Reported Outcomes After Outpatient Single-Level Instrumented Posterior Lumbar Interbody Fusion in a Surgery Center: Preliminary Results in 16 Patients. Spine 2015;40:E36-42. [Crossref] [PubMed]
- Adamson T, Godil SS, Mehrlich M, et al. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine 2016;24:878-84. [Crossref] [PubMed]
- McGirt MJ, Godil SS, Asher AL, et al. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus 2015;39:E9. [Crossref] [PubMed]
- Khanna R, Kim RB, Lam SK, et al. Comparing Short-term Complications of Inpatient Versus Outpatient Single-level Anterior Cervical Discectomy and Fusion: An Analysis of 6940 Patients Using the Acs-nsqip Database. Clin Spine Surg 2018;31:43-7. [Crossref] [PubMed]
- Vaishnav A, Hill P, McAnany S, et al. Safety of 2-level Anterior Cervical Discectomy and Fusion (ACDF) Performed in an Ambulatory Surgery Setting With Same-day Discharge. Clin Spine Surg 2019;32:E153-9. [Crossref] [PubMed]
- Chin KR, Pencle FJR, Seale JA, et al. Clinical Outcomes of Outpatient Cervical Total Disc Replacement Compared With Outpatient Anterior Cervical Discectomy and Fusion. Spine (Phila Pa 1976) 2017;42:E567-74. [Crossref] [PubMed]
- Segal DN, Wilson JM, Staley C, et al. Outpatient and Inpatient Single-level Cervical Total Disc Replacement: A Comparison of 30-day Outcomes. Spine 2019;44:79-83. [Crossref] [PubMed]
- Bovonratwet P, Fu MC, Tyagi V, et al. Safety of Outpatient Single-level Cervical Total Disc Replacement: A Propensity-Matched Multi-institutional Study. Spine (Phila Pa 1976) 2019;44:E530-8. [Crossref] [PubMed]
- Reiter K. A Look at Best Practices for Patient Education in Outpatient Spine Surgery. AORN J 2014;99:376-84. [Crossref] [PubMed]
- Bednar DA. Description and Results of a Comprehensive Care Protocol for Overnight-Stay Spine Surgery in Adults. Spine (Phila Pa 1976) 2017;42:E871-5. [Crossref] [PubMed]