Open facet joint denervation as an adjunct in patients undergoing posterior lumbar decompression for spinal stenosis—a single blinded randomized controlled trial
Introduction
Back pain may come from a number of anatomical sites, one of which is the facet joints (1). The rationale of radiofrequency denervation is that patients with facet joint pain should obtain relief if the nerves that innervate it are coagulated (2). In the USA, lumbosacral facet radiofrequency denervation increased 568% in Medicare beneficiaries from 2000 to 2014 (3).
Despite the increasing use of this treatment, the duration of the effectiveness of facet radiofrequency denervation is not clear from placebo-controlled studies. Leclaire et al. reported that facet radiofrequency denervation is more effective than placebo for improvement in function but not pain at 4 weeks and for neither by 3 months (4). Others have found that pain relief with radiofrequency denervation is better than placebo at 6 months (5,6). Two studies reported that facet radiofrequency denervation is better than placebo with respect to pain and disability at 1 year (7,8). Therefore, in the Cochrane review of studies up to May 2014, the authors’ recommended that practitioners use caution in using radiofrequency denervation in routine practice until high quality studies on efficacy and cost effectiveness were performed (9).
Most recently, whether facet radiofrequency denervation is effective at all has been raised with Juch et al. reporting no differences in short term or 1-year outcome for patients with chronic low back pain randomized to facet radiofrequency denervation versus a control group (10). Bogduk et al. state that some of the clinical failures may be due to technical limitations when performing percutaneous radiofrequency denervation (11).
The traditional teaching is that a laminectomy to decompress the neural elements is intended to address leg symptoms but that the degenerative facet would remain and therefore, any back pain that it caused would still be present postoperatively. Although there are conflicting reports about its effectiveness, as radiofrequency denervation is an increasing common treatment for facet generated back pain, we wanted to see if adding an open facet denervation would decrease the back pain in our patients undergoing a laminectomy for spinal stenosis due to facet and ligamentum flavum hypertrophy, hence decreasing their overall pain and improve function postoperatively. To test this theory, we randomized our patients having both leg symptoms and low back pain scheduled for a laminectomy to either having or not having a facet denervation and compared the overall pain and function postoperatively in the two groups.
Methods
Study design
This study took place at a single University Health Sciences Centre between July 2016 and August 2017. Sixty-one patients were enrolled and followed for this randomized parallel single blinded trial. All study participants were blinded to their treatment group, and at no time during the course of this study was their treatment assignment revealed to them. Before the start of the study, the research manager prepared and sealed opaque envelopes based on a computer generated 1:1 allocation ratio randomization scheme. These stratum-specific envelopes containing group assignments were sealed, stored in an operating area cupboard and opened by the study surgeon when the participant was ready for their surgical procedure. The principal investigator with 27 years of experience in spinal surgery, performed all the operations. The registration number for this trial is NCT03487120 in the clinicaltrials.gov Protocol Registration and Results System with approval from our Investigational Review Board.
All eligible participants were aged above 19 years with a diagnosis of degenerative lumbar spinal stenosis based on MRI documentation of a combination of disk bulging, facet degeneration and ligamentum flavum hypertrophy who in addition to having neurogenic claudication, complained of back pain for at least 3 months. Positive facet blocks were not a criterion for eligibility. All participants had failed a trial of non-operative management before surgery. Patients were ineligible for this research if they had one or more of the following: previous surgery on their spine, fracture, systemic inflammatory disease, malignancies or an infection affecting their spine, worker’s compensation, insurance, or legal claims.
Participants were randomized to two groups. Group A had lumbar laminectomy(s) with denervation of the facet joint(s) at the level decompressed. Group B had a lumbar laminectomy(s) without facet joint denervation. The surgical procedure was focused on treating the patients’ leg symptoms by decompressing the area of neural compression identified on MRI. The operation was a bilateral posterior decompression from a unilateral approach done by removing the lamina, adjacent ligamentum flavum and medial one half of the facet on one side, leaving the entire spinous process and adjacent interspinous ligaments as well as the lamina and facet on the other side intact. As such, one facet could be denervated depending on randomization, for each spinal level addressed. We did foraminotomies on all of the cases but none had discectomies. No participants had fusions with or without instrumentation and all underwent a uniform postoperative physiotherapy protocol.
Both groups had their total pain and functional limitations measured using a 10 cm visual analogue scale (VAS) and the Roland-Morris Disability Questionnaire (RMDQ). The RMDQ is a health status measure to assess disability due to low back pain. It consists of 24 questions, 22 dealing with physical function, 1 with mood, and 1 with frequency of pain (12). The RMDQ is scored by adding up the number of items checked by the patient. Greater levels of disability are reflected by higher numbers. Scores under 4 and over 20 may not show significant change over time (13). The RMDQ is one of the most used validated back-pain specific questionnaires to assess disability (14).
The assessor was kept blinded to the patients’ treatment group. All measures were taken before surgery and at 6, 12 and 24 weeks postoperatively. We chose to follow up our patients for 24 weeks so that we could compare our findings to others who reported results within this time period, and because the effect of radiofrequency facet denervation provides temporary relief reported to be on average 10.5 months (4-6,15). Therefore, the results in both our denervation and no denervation groups would be expected to converge over time and we selected 24 weeks of follow up to prevent this from being a potential factor.
Denervation technique
The medial branch enters the posterior spine through the intertransverse ligament and runs caudally in the groove between the transverse process and the superior facet, then curving medially to end on the lamina of the vertebra below innervating the caudal portion of the facet at that level and the cranial portion of the one below it (16). Therefore, each facet has dual innervation (16) which we addressed by the laminectomy and medial facetectomy of the inferior facet plus cauterization of the superior, lateral, and inferior soft tissue surrounding that same facet joint.
Bipolar electrocautery using the System 5000™ Electrosurgical Generator ESU (ConMed®, Utica, New York, USA) set on micro mode at 20 Watts was used to cauterize the soft tissue around the cranial, lateral, and caudal aspects of the facet joint. This included the entire length of the bony groove between the transverse process and the superior facet where Bogduk recommends that the cauterization of the medial branch take place using the radiofrequency electrode (11). Charring of the soft tissues under direct vision was done to ensure that the denervation was complete.
Statistical analyses
Descriptive statistics were used to summarize patient demographics and outcomes. Differences on the RMDQ scores across different times and between groups were analyzed with one-way ANOVAs and Bonferroni post hoc tests. The RMDQ scores across times within groups were analyzed using the non-parametric Friedman’s test and the Wilcoxon sign ranks was used as the post hoc test. Parametric and non-parametric tests including independent samples t-tests, Chi-square, and the Mann Whitney U were used to analyze the ages, sex, and the pain data within and between groups. An alpha value of <0.05 was considered statistically significant.
The sample size estimate was based on a study that found a significant improvement in back pain after surgery as assessed by the RMDQ (17). Based on a change from baseline of 11 points, and standard deviations of 4.7 and 6.1, a sample size of 4 was needed in each treatment group. We decided to significantly increase this sample size because we were concerned that this would be low for clinical relevance. In addition, recruitment and adding the denervation to the laminectomy was not difficult and therefore, 61 patients were enrolled in the study.
Results
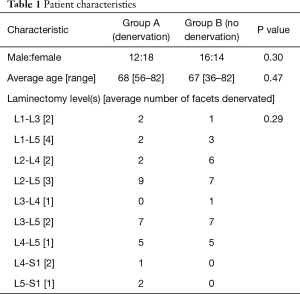
Sixty-one patients were enrolled (28 men and 33 women). One patient died and was removed from the study. The cause of death was not related to the procedure (Figure 1). There were no complications in either group. The one loss to follow-up resulted in analyses that involved all 60 participants. Furthermore, all analyses were by originally assigned groups. Baseline characteristics of the two groups were comparable (Table 1).
Full table
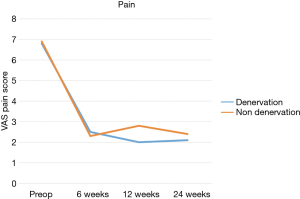
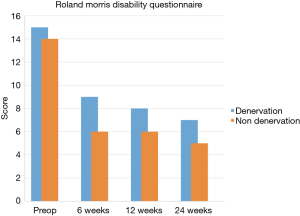
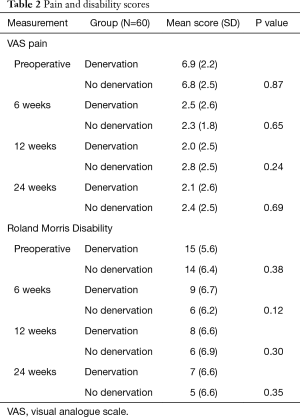
There were no statistically significant differences between groups on the pain scores at baseline or at 6-, 12- and 24-week follow-up times. The same result was found when analyzing the disability scores (Table 2).
Full table
When measures were examined by group, pain and disability scores showed significant improvements from baseline for all follow-up visits (P=0.01; P=0.001) in both the control and denervation groups (Figures 2 and 3).
Discussion
Our results showed that the total pain and disability scores within both groups significantly improved from baseline which would be expected because laminectomy(s) to address the neurogenic claudication of patients were done in both groups. Our intent was not to study the effect of facet denervation on back pain and spinal stenosis on neurogenic claudication as separate entities but as an adjunct treatment to laminectomy for the overall pain and disability of patients with spinal stenosis. However, there was no significant differences in pain or function between the open facet denervation and control groups at early, mid, or 24-week follow-up. This is consistent with the recent Mint Randomized Clinical Trials (10) which reported no improvement in chronic low back pain with radiofrequency facet denervation which is in contrast to older studies that have found that it is more effective than placebo (5-8). However, it should be emphasized that we did not study the effect of medial nerve ablation on back pain in patients having a positive diagnostic block.
The randomized single-blinded placebo-controlled design of our study was its main strength. A second strength is that we exceeded the number of patients needed according to the power calculation, and only lost 1 patient to follow-up.
One weakness is that our facet denervation was carried out using open bipolar electrocautery while other studies employ percutaneous radiofrequency denervation. However, even with percutaneous radiofrequency denervation, there are several different techniques used. Bogduk et al. state that not all the percutaneous techniques affect a wide enough area to coagulate the nerve and the open method is effective (11).
Another weakness is that we did not employ diagnostic blocks when selecting which facets to denervate. However, Cohen et al. reported that the administration of radiofrequency denervation based on clinical findings yielded a higher proportion of successful outcomes compared to using 1 and 2 diagnostic blocks in the decision-making process (18). It is traditionally taught that decompression of the neural elements treats the neurogenic claudication but does not address the back pain due to the degenerative facets and disc. One of our inclusion criteria was that the participant had back pain for at least 3 months and we made the assumption that the facet at the level of the neural compression being addressed by the laminectomy was a source of pain. We based this assumption on Kirkaldy-Willis’s “three-joint complex” theory which states that it is the degeneration of the facets and disc resulting in subluxation and osteophyte formation that causes spinal stenosis at that level (19). For these reasons, we feel that our clinical choice of facets to denervate according to the stenosis is a reasonable assumption. However, the addition of positive diagnostic facet blocks as an inclusion criterion for both the facet denervation and no facet denervation groups would reduce bias from non-specific back pain and be a goal for future work.
A further weakness is that we only used the VAS and RMDQ as measures of outcome. The addition of other patient reported outcomes would improve the sensitivity of finding differences between the facet denervation and no facet denervation groups. The addition of walking distance and time to narcotic independence or reduction of narcotic use as outcome measures would be a goal for future work.
A final weakness is that only one facet was denervated for each spinal level addressed because we employed a bilateral posterior decompression from a unilateral approach. Although we chose the patients’ reported more symptomatic side to carry out the unilateral approach and denervated the facet on that side, we cannot be certain that it as opposed to the one on the other side at that level, was the cause for the patients’ back pain. However, unless we chose the wrong facet as the cause for the patient’s back pain in all the patients in the denervation group, there should have been some difference pain and functional between the two groups if the addition of facet denervation to lumbar laminectomy(s) was effective treatment.
Conclusions
We could not show a difference in short-term pain and function with addition of denervation of the facet(s) to treat back pain in patients undergoing laminectomy(s) for spinal stenosis within our study design and further work addressing the weaknesses in the preceding discussion are necessary.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Investigational Review Board (No. 6018074). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Shealy CN. Facet denervation in the management of back and sciatic pain. Clin Orthop Relat Res 1976.157-64. [PubMed]
- Dreyfuss P, Halbrook B, Pauza K, et al. Efficacy and validity of radiofrequency neurotomy for chronic lumbar zygapophysial joint pain. Spine (Phila Pa 1976) 2000;25:1270-7. [Crossref] [PubMed]
- Manchikanti L, Hirsch JA, Pampati V, et al. Utilization of Facet Joint and Sacroiliac Joint Interventions in Medicare Population from 2000 to 2014: Explosive Growth Continues!. Curr Pain Headache Rep 2016;20:58. [Crossref] [PubMed]
- Leclaire R, Fortin L, Lambert R, et al. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine (Phila Pa 1976) 2001;26:1411-6; discussion 1417. [Crossref] [PubMed]
- Gallagher J, Petriccione di Vadi PL, Wedley JR, et al. Radiofrequency facet joint denervation in the treatment of low back pain: a prospective controlled double-blind study to assess its efficacy. Pain Clin 1994;7:193-8.
- Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: a randomized double-blind trial. Spine (Phila Pa 1976) 2008;33:1291-7; discussion 1298. [Crossref] [PubMed]
- Tekin I, Mirzai H, Ok G, et al. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain 2007;23:524-9. [Crossref] [PubMed]
- van Kleef M, Barendse GA, Kessels A, et al. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine (Phila Pa 1976) 1999;24:1937-42. [Crossref] [PubMed]
- Maas ET, Ostelo RW, Niemisto L, et al. Radiofrequency denervation for chronic low back pain. Cochrane Database Syst Rev 2015.CD008572. [PubMed]
- Juch JNS, Maas ET, Ostelo RWJG, et al. Effect of Radiofrequency Denervation on Pain Intensity Among Patients With Chronic Low Back Pain: The Mint Randomized Clinical Trials. JAMA 2017;318:68-81. [Crossref] [PubMed]
- Bogduk N, Macintosh J, Marsland A. Technical limitations to the efficacy of radiofrequency neurotomy for spinal pain. Neurosurgery 1987;20:529-35. [Crossref] [PubMed]
- Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976) 2000;25:3115-24. [Crossref] [PubMed]
- Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 1983;8:141-4. [Crossref] [PubMed]
- Yamato TP, Maher CG, Saragiotto BT, et al. The Roland-Morris Disability Questionnaire: one or more dimensions? Eur Spine J 2017;26:301-8. [Crossref] [PubMed]
- Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for lumbar facet pain. Spine (Phila Pa 1976) 2004;29:2471-3. [Crossref] [PubMed]
- Bogduk N, Long DM. Percutaneous lumbar medial branch neurotomy: a modification of facet denervation. Spine (Phila Pa 1976) 1980;5:193-200. [Crossref] [PubMed]
- Scott-Young MN, Lee MJ, Nielsen DEA, et al. Clinical and Radiological Mid-Term Outcomes of Lumbar Single-Level Total Disc Replacement. Spine (Phila Pa 1976) 2018;43:105-13. [Crossref] [PubMed]
- Cohen SP, Williams KA, Kurihara C, et al. Multicenter, randomized, comparative cost-effectiveness study comparing 0, 1, and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology 2010;113:395-405. [Crossref] [PubMed]
- Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, et al. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976) 1978;3:319-28. [Crossref] [PubMed]