
Are dorsal ramus nerve blocks the solution to postoperative lumbar spine surgery pain?
Introduction
Open microdiscectomies and decompression surgery of the lumbar spine typically involves significant soft tissue dissection and stripping. This results in the activation of nociceptive, neuropathic and inflammatory pain mechanisms (1). After surgery, patients often experience intense pain, initially severe at rest that has adverse effects on early mobilisation (2). Currently, pain control after spinal surgery follows a multimodal approach that aims to reduce opiate requirements. Good evidence supports the use of gabapentinoids, acetaminophen, neuraxial blockade and extended-release local anaesthetics in alleviating pain and reducing narcotic requirements (3); however, large variations in clinical practice exist, reflecting surgeons and anaesthetists differing assessment of the efficacy, safety and cost-effectiveness associated with each agent (4).
Among the various analgesia modalities following spinal surgery, the lumbar dorsal ramus nerve (DRN) block is a simple, minimally invasive option. However, there is a paucity of literature detailing its efficacy in pain management following minor lumbar spine decompression surgery (5). Establishing this technique’s efficacy and superiority to local anaesthetic field infiltration of surgical wound is essential for the refinement of post-operative pain management protocols after one or two-level spinal decompression surgery. We hypothesised that perioperative lumbar DRN block is beneficial and superior to surgical wound field infiltration in alleviating post-operative pain and facilitates early mobilisation and discharge.
Methods
Patient selection and data collection
We conducted a case-control observational, single centre, prospective study of 15 consecutive patients who had DRN block immediately before a single-level lumbar discectomy or one/two-level lumbar spinal decompression at our institute between May and July 2018. Patients with chronic pain were not excluded. Patients were defined as chronic pain suffers if they reported pain for greater than 12 months and were taking regular opiates or gabapentinoids.
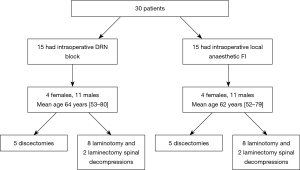
Fifteen patients, who had local anaesthetic field infiltration of their surgical wounds, were case-matched to form a comparator group, as illustrated in the consort diagram (see Figure 1). Matching criteria included type of operation performed, laterality, vertebral level, age of patient (±5 years) and gender. Those were selected from the operating theatre register for surgeries performed during 2016 and 2017. Case-matching was performed with blinding to the patient identifiable information and outcomes.
Retrospective review of prospectively collected data was performed. Pain at rest was assessed using a numerical rating scale and documented by the ward nursing staff. Patient notes were reviewed to assess if patient mobilised in the first 24 hours after surgery. Prescription and anaesthetic records were reviewed to establish opiate usage. Hospital records were interrogated to establish length of stay. The preoperative and 6 weeks postoperative Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) were collected. All questionnaires and forms were collected and checked for completeness by a lead researcher.
Surgeries and post-operative protocols
The same surgeon performed all surgeries. Discectomies and Laminotomy (Fenestration) spinal decompressions were performed through a midline incision that is no longer than 2 cm in length, followed by subperiosteal stripping of the multifidus and paraspinal musculature. Laminectomy spinal decompression utilised the same approach bilaterally with a wound length no longer than 4–5 cm, followed by the removal of the spinous process and both laminae.
Patients routinely received 100–400 mg of fentanyl during surgery (these were included in the 24-hour opiate calculations). During the postoperative hospital stay, patients were free to ask for supplemental ‘rescue’ analgesic and all patients received paracetamol 1 g four times a day.
Dorsal ramus nerve block procedure in the DRN group
Ultrasound guidance DRN block, immediately before surgery was performed by a single senior anaesthetist (n=10) or intra-operatively by the surgeon utilising landmark technique (n=5). The DRN block was performed on the ipsilateral side of the decompression and bilateral in those who underwent bilateral spinal decompression procedure. The ultrasound technique as described by Al-Alami et al. was used (5). Longitudinal paramedian scanning of the transverse process of thoraco-lumbar spine was obtained. The DRN block was performed on the ipsilateral side using an in-plane approach with hydrodissection technique using a 22-G 100 mm spinal needle. For levels L1–L4, injections were made at the postero-superior edge of the transverse process just lateral to the zygapophysial joint. For the L5 level, injections were made at the transverse process of L5 and at the sacroiliac groove midway between L5 transverse process and sacral ala. In the intraoperative landmark technique, the transverse process can be readily identified and infiltration with a 20-G needle performed. Both employed 20 mL of 0.5% bupivacaine.
Surgical wound field infiltration of local anaesthetic (FI) group
20 mL of 0.5% bupivacaine was used to infiltrate the skin and subcutaneous tissues just before wound closure.
Outcome measures
The primary outcomes investigated are the mean and maximum rest pain scores and the average morphine sulphate equivalents requirement in the first 24 hours. For objective assessment of pain medication usage, all narcotic medications were converted into their respective morphine sulfate equivalents using an equianalgesic dose table where pain relief with 10 mg parenterally administered morphine is used as a reference standard (6). Furthermore, analysis of morphine sulphate equivalents including intra-operative opiates was performed. Secondary outcomes measured were early mobilisation achieved (defined as on day of surgery) and length of stay (LoS). We also report the 6-week change in ODI and VAS scores.
Statistical analysis
Statistical analysis was performed on two cohorts: DRN block patients and field infiltration patients. Nominal and ordinal data are described as case numbers and percentages with comparison using Fisher’s exact tests. Continuous data is presented as mean and range with comparison using t-test. Statistical significance is set at the 95% confidence interval. SPSS (IBM Corp. in Armonk, NY) was used for analysis.
Results
Thirty patients were included, 15 had DRN block, case controlled with fifteen who had FI. In each group, there was 4 females and 11 males with a mean age of 62–64 years (range, 52–80 years) (Flowchart). Five of those were chronic pain sufferers. The surgeries were performed for disc hernia in six, degenerative spinal stenosis in 7 (including two with spondylolisthesis) and lateral recess stenosis in two. Those were treated surgically with discectomy (n=5) laminotomy (n=8) and laminectomy (n=2). One discectomy case was a revision procedure. These were various lumbar levels (L3–S1) with L4/5 being the most common and nine were bilateral.
Primary outcome
Table 1 demonstrates that DRN block and field infiltration patients had mean pain score at rest in the first 24 hours post-operation of 2.8 vs. 2.7 (P=0.90). Higher maximum rest pains were reported in the DRN group compared with the field infiltration group (5.7±2.6 vs. 5.0±2.5), however, this was not statistically significant (P=0.42). Similarly, no significant differences were seen in the morphine sulphate equivalents dosages required by each group (142.6±37.3 vs. 124.6±55.0, P=0.30).

Full table
Secondary outcome
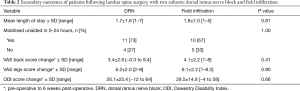
Table 2 shows similar proportions of patients mobilised early in the DRN and field infiltration groups (73% vs. 67%, P=1.00). The mean LoS was also similar between groups, 1.7 vs. 1.8 days (P=0.81). No differences in the improvements in VAS back (P=0.41), VAS legs (P=0.90) and ODI score (P=0.66) was observed between groups (see Table 3).
Full table

Full table
Discussion
Postoperative analgesia following spinal surgical procedures follows a multimodal approach and is a well-established practice; however, each modality has its side effects and possible complications that must be considered. Dorsal Ramus Nerve block has the potential to provide good postoperative pain relief with minimal side effects and complication.
The co-existence of dual sensory innervation of the back has been described (7); one arising directly from the spinal nerve segmentally, whereas the other derived from a non-segmental ascending innervation through the paravertebral sympathetic chain. Thus, blockage of the DRN impacts on both segmental and non-segmental innervation (8). As a result, DRN block has been proposed as an effective treatment method for chronic back pain. Miyakoshi et al. demonstrate that their blocks, confirmed with radiocontrast and computerised tomography, resulted in total dorsal ramus blocks. They report significant alleviation of pain at rest and during motion after total DNR block compared to the trigger point injections up to 7 days after the treatment for chronic back pain (P<0.01) (9).
Al-Alami et al. describe the ultrasound guidance technique used to perform pre-emptive DNR blocks at levels T12–L5 in six patients prior to spinal surgery. They do not present any outcome data to support its efficacy (5). In this study, the dorsal ramus nerve block did indeed provide postoperative pain control, but this was as good as local anaesthetic infiltration of the surgical wound in terms of postoperative pain scores, early mobilisation and length of hospital stay.
Opiates are often used as a first line analgesia and their efficacy in spinal surgery is well established (10), however, side effects often limit their use. Patient who had DRN block did not require less opiates in the first 24 hours when the maximum benefit of a block would be expected compared with the field infiltration group.
Patient controlled analgesia (PCA) also has an established superiority in terms of quality of analgesia and ease of use compared to intermitted divided dosing (4). In this cohort, fewer patients required PCA in the DRN block group than field infiltration group (7% vs. 33%, P=0.17) (Table 3).
Generalised local anaesthetic infiltration of wounds has proven to be effective in many areas of surgery. this is limited by potential risk of systemic toxicity. Bianconi et al, propose wound infiltrated with a solution of ropivacaine 0.5% 200 mg/40 mL, and an infusion of ropivacaine 0.2% 5 mL/h was maintained for 55 hours following spinal fusion surgery. This resulted in significant reduction pain scores and rescue medication (diclofenac and tramadol) requirements (2). Similarly, Reuben et al. found that continuous systemic administration of nonsteroidal anti-inflammatory drugs (NSAIDs) is effective in controlling pain after lumbar stabilization surgery. Moreover, when associated with centrally acting drugs such as opioids, NSAIDs have an opioid-sparing effect (11). Continuous infusions for less invasive surgeries, such as those in this study, would carry a different risk benefit profile and prolong length of hospital stay.
The number of patients with chronic pain undergoing surgical procedures is increasing, presenting a unique challenge to peri-operative pain management (12,13). Furthermore, the proportion of non-cancer chronic pain patients treated with long-term opioids is rising. Opiate use in this context is associated with issues of tolerance, dependency and addiction (13-15). Suffering chronic pain along with long-term analgesia use leads to altered pain perception, which can complicate pain management (16,17). This patient group may have had previous unpleasant experiences with poor pain control in hospital and are typically anxious pre-operatively (12). Additional opiate requirements are typically anticipated following a surgical procedure and local, regional anesthesia, and multimodal analgesia are indicated whenever possible (13,16,18). Our DRN block group had greater proportion of chronic pain suffers (40% vs. 13%, P=0.21) which, whilst not statistically significant in our small sample size, may have confounded the primary outcomes.
Whilst DRN block had limited value for our patient group, a randomised controlled study of patients undergoing one or two level lumbar spine decompression without fixation randomised to DRN block, field infiltration and no local anaesthetic groups with large number of participants would be necessary to ascertain the efficacy of DRN blocks in postoperative pain management. However, the heterogenous nature of spinal surgeries (different levels, unilateral/bilateral, pathologies, surgical approach, and extent of decompression) would present a challenge to equal recruitment into each treatment arm. In addition, the results of this study suggest any difference between groups would be small and an arbitrary clinically significance difference would need to be set.
Effort was made to strengthen this study by: (I) case-control matching to the exact pathology, operation performed, patient gender and blinding to the patient identifiable information and outcomes during the selection process; (II) the use of reproducible, objective outcome measures; and (III) reporting the results following the STROBE (Strengthening the reporting of observational studies in epidemiology) guidelines.
A limitation of this study was the single-centre, single surgeon series. The surgeries performed were heterogenous and a small sample size. Considering future areas of study, whilst our study found no difference between DRN block and field infiltration, combining both may be synergistic and provide greater pain relief. Of potential benefit to future studies of DRN in spinal surgeries would be measuring a post-operative creatine phosphokinase (CK) level. This blood test is a valid surrogate marker of surgical muscular injury (19), and could help stratify which spinal surgeries benefit from a DRN. However, Lombao Iglesias et al. found the incidence of severe post-operative pain in 96 patients following posterior midline incision is not significantly related to CK level (20).
Conclusions
In this small study dorsal ramus nerve block was not superior to local anaesthetic field infiltration of surgical wound in minor one or two level lumbar spinal decompression surgery in terms of alleviating pain, reducing opiate requirements, or facilitating earlier mobilisation and discharge.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by The North Devon Audit and Effectiveness board Reference: NDDH/DRN-3091. Informed consent for the surgery was obtained from all individual participants included in the study.
References
- Mathiesen O, Dahl B, Thomsen BA, et al. A comprehensive multimodal pain treatment reduces opioid consumption after multilevel spine surgery. Eur Spine J 2013;22:2089-96. [Crossref] [PubMed]
- Bianconi M, Ferraro L, Ricci R, et al. The pharmacokinetics and efficacy of ropivacaine continuous wound instillation after spine fusion surgery. Anesth Analg 2004;98:166-72. table of contents. [Crossref] [PubMed]
- Devin CJ, McGirt MJ. Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes. J Clin Neurosci 2015;22:930-8. [Crossref] [PubMed]
- Bajwa SJ, Haldar R. Pain management following spinal surgeries: An appraisal of the available options. J Craniovertebr Junction Spine 2015;6:105-10. [Crossref] [PubMed]
- Al-Alami A, Abou El Ezz A, Kassab F. Ultrasound guided dorsal ramus nerve block for reduction of postoperative pain in patients undergoing lumbar spine surgery: a case series imaging study. Middle East J Anaesthesiol 2015;23:251-6. [PubMed]
- Berdine HJ, Nesbit SA. Equianalgesic dosing of opioids. J Pain Palliat Care Pharmacother 2006;20:79-84. [Crossref] [PubMed]
- Edgar MA. The nerve supply of the lumbar intervertebral disc. J Bone Joint Surg Br 2007;89:1135-9. [Crossref] [PubMed]
- Higuchi K, Sato T. Anatomical study of lumbar spine innervation. Folia Morphol (Warsz) 2002;61:71-9. [PubMed]
- Miyakoshi N, Shimada Y, Kasukawa Y, et al. Total dorsal ramus block for the treatment of chronic low back pain: a preliminary study. Joint Bone Spine 2007;74:270-4. [Crossref] [PubMed]
- Gottschalk A, Durieux ME, Nemergut EC. Intraoperative methadone improves postoperative pain control in patients undergoing complex spine surgery. Anesth Analg 2011;112:218-23. [Crossref] [PubMed]
- Reuben SS, Connelly NR, Lurie S, et al. Dose-response of ketorolac as an adjunct to patient-controlled analgesia morphine in patients after spinal fusion surgery. Anesth Analg 1998;87:98-102. [PubMed]
- Hadi I, Morley-Forster PK, Dain S, et al. Brief review: perioperative management of the patient with chronic non-cancer pain. Can J Anaesth 2006;53:1190-9. [Crossref] [PubMed]
- Brill S. Managing surgical pain in long-term opioid patients. J Pain Palliat Care Pharmacother 2013;27:185-7. [Crossref] [PubMed]
- Brill S, Ginosar Y, Davidson EM. Perioperative management of chronic pain patients with opioid dependency. Curr Opin Anaesthesiol 2006;19:325-31. [Crossref] [PubMed]
- Huxtable CA, Roberts LJ, Somogyi AA, et al. Acute pain management in opioid-tolerant patients: a growing challenge. Anaesth Intensive Care 2011;39:804-23. [Crossref] [PubMed]
- Richebé P, Beaulieu P. Perioperative pain management in the patient treated with opioids: continuing professional development. Can J Anaesth 2009;56:969-81. [Crossref] [PubMed]
- Loftus RW, Yeager MP, Clark JA, et al. Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. Anesthesiology 2010;113:639-46. [PubMed]
- Bourne N. Acute pain management in the opioid-tolerant patient. Nurs Stand 2010;25:35-9. [Crossref] [PubMed]
- Arts MP, Nieborg A, Brand R, et al. Serum creatine phosphokinase as an indicator of muscle injury after various spinal and nonspinal surgical procedures. J Neurosurg Spine 2007;7:282-6. [Crossref] [PubMed]
- Lombao Iglesias D, Bagó Granell J, Vilor Rivero T. Validity of creatine kinase as an indicator of muscle injury in spine surgery and its relation with postoperative pain. Acta Orthop Belg 2014;80:545-50. [PubMed]


