
The operative treatment of shoulder pain in patients with a concurrent diagnosis of cervical spondylosis and shoulder dysfunction
Introduction
Complaints of neck and shoulder pain are amongst one of the most common orthopaedic problems, impacting activities of daily living and in turn affecting quality of life in thousands of patients. International studies have estimated a yearly cost as high as 4,400 US dollars in the treatment of shoulder pain in the primary care setting (1). Etiology of neck and shoulder pain may be multifactorial. Symptoms including pain, weakness, numbness, or tingling, may be due to cervical spine or shoulder pathology, and as such, making a diagnosis and treatment plan may be complicated (2,3). A thorough and specialized workup, including a history, physical exam (4), use of patient reported outcome measures (5), and imaging (6) will help to guide early and hopefully definite treatment.
Cervical radiculopathy may present with similar clinical symptoms that are seen with shoulder pathology (2,3). Degenerative disc disease, herniation, and foraminal stenosis (7) cause impingement of the cervical spine nerve roots presenting with the similar shoulder pain and weakness as structural shoulder defects do. While injury to most of the cervical nerve roots can result in upper extremity symptoms (8), Campbell et al. note that injury to the C5 nerve root was most often implicated in shoulder pain (9). Physical exam maneuvers including the Spurling test and diagnostic tests including plain radiographs, MRI, and electromyography (EMG) can help to identify cervical spinal causes of shoulder symptoms (10). Once the diagnosis is achieved, treatment options, including operative (11) and non-operative interventions, can be explored.
Depending on age, history, and mechanism of injury, the most common shoulder pathologies include subacromial impingement, rotator cuff tears, and osteoarthritis (12), but multiple other causes such as labral tears and bicep tendon tears can be implicated in shoulder complaints. Similar to the approach in the cervical spine, physical exam maneuvers (13), including the Neer test, the Hawkins-Kennedy test, and the Speed test, and imaging (6) centering around plain radiographs and magnetic resonance imaging (MRI) identify these pathologies. While guided physical therapy and other conservative measures have been shown to be successful treatment options (14,15), operative interventions (16) might be necessary to treat persistent symptoms.
While differentiating between spinal versus shoulder pathology should be a central part of a physician’s workup of shoulder pain (17-19), the clinical picture might be complicated by the presence of both problems concomitantly. In patients with both diagnoses of cervical and shoulder pathology, surgical intervention may be warranted after all conservative management options have failed. There are often instances where patients ultimately end up needing surgical intervention for both pathologies, and the common dilemma is which is addressed first.
The choice of whether to start with spine or shoulder surgery is an important clinical decision to make based on severity of pathologies, comorbidities, and patient preference. The literature does not offer a clear answer to this complicated picture, with very few studies exploring the incidence or results of the surgical treatment paths followed in this clinical situation (20). With this study, the authors aim to provide incidence data of patients with both cervical spine and shoulder pathology who needed various cervical spine, shoulder, and multiple surgeries while reporting their effectiveness in treating a patient’s presenting symptoms. The authors procured this study believing that the site of operative intervention chosen, the number of operations, and the order of operation all affect patient-perceived treatment success.
Methods
This study was conducted at a suburban Orthopaedic Surgery department after obtaining approval from our Institutional Review Board (IRB). The authors retrospectively reviewed the chart of every patient between 2009 and 2017 who not only received diagnoses of cervical spine and shoulder pathology but also underwent operative intervention for one or both etiologies. An a priori power analysis was performed to determine the sample size needed to demonstrate a significant difference between cohorts. No patient, regardless of age, ethnicity, gender, or past medical history, was excluded.
For each patient, demographic information, cervical spine and shoulder diagnoses, operative details, a subjective report of operative success (defined as an alleviation of shoulder symptoms that the patient was satisfied with and did not feel the need to seek out further intervention for) in relieving shoulder symptoms, and numerical rating scale (NRS) pain scores were recorded. It was assumed that all surgeries were done due to presence of clinical symptoms that brought the patient to the outpatient clinic and led to them deciding to have surgery. Using notes from physical therapy sessions and physician physical examinations, Focus on Therapeutic Outcome (FOTO) scores and final shoulder ranges of motion (ROM) were also recorded. Patients who filled out Neck Disability Index (NDI) questionnaires had their scores recorded as well. Finally, post-operative total opioid use (measured in milimorphine equivalents) was recorded using our state’s online drug monitoring program website.
Descriptive statistics, Chi-squared statistical tests, Mann Whitney rank sum tests, and independent t-tests were used as appropriate to compare the rates of subjective reports of success, pain scores, functional outcomes, and opioid use among patients who had one type of surgery (spine surgery versus shoulder surgery), single surgery versus multiple surgeries, and multiple surgeries (spine then shoulder surgery versus shoulder then spine surgery) (IBM SPSS Version 23 Statistics for Windows, Armonk, NY: IBM Corp.). For all analyses, statistical significance was set at P≤0.05.
Results
Overall, 154 charts of patients with concomitant cervical spine and shoulder pathology who underwent operative intervention were reviewed and analyzed. A demographic breakdown of our patient population is detailed in Table 1. A majority of our patients were male (n=90, 58.4%) and between the ages of 40 and 59 years (n=95, 61.7%). Patients had an average wait time of 299 days (0.81 years) between initial diagnosis and their final surgery. After surgical intervention, 70 patients (45.5%) overall noted cessation of original shoulder symptoms (pain, weakness, numbness, or tingling) during their last follow-up visit.
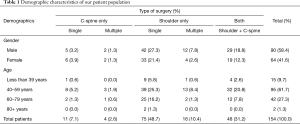
Full table
Fifteen patients (9.7%) underwent cervical spine surgery (4 had multiple spine surgeries), most commonly for arthritic changes (n=7, 46.7%). Three (20.0%) of these patients also had isolated rotator cuff pathology (Table 2). While many patients had myelopathy with concomitant radicular symptoms, 9 (60.0%) patients had myelopathy while 6 (40.0%) patients had only radicular symptoms. Patients had an average wait time of 279 days (0.76 years) between initial diagnosis and final surgery. Most of these patients (n=12, 80.0%) underwent isolated multi-level anterior cervical discectomy and fusion (ACDF) involving the C5−C6 level (n=13, 86.7%). Ninety-one patients (59.1%) underwent shoulder surgery (10 patients had multiple surgeries), most commonly for multiple pathologies (n=49, 53.8%) and isolated rotator cuff tears (n=24, 26.4%). Twenty-nine (31.9%) of these patients also had arthritic cervical spine changes (Table 2). Patients had an average wait time of 202 days (0.55 years) between initial diagnosis and surgery. Ninety (98.9%) patients underwent arthroscopic intervention (58 rotator cuff repairs), and one (1.1%) patient underwent open repair of a superior labrum from anterior to posterior (SLAP) tear.
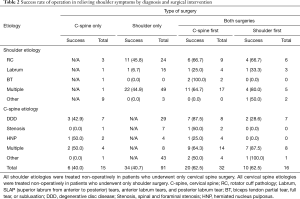
Full table
Finally, 48 patients (31.2%) underwent both spine and shoulder operations. Most patients who had cervical spine surgery first had multiple pathologies (n=14, 43.8%) and multiple shoulder pathologies (n=17, 53.1%). Fifteen (46.9%) patients had myelopathic symptoms, either in isolation or concomitantly with radiculopathy, while 5 (15.6%) patients had only radicular symptoms. These patients mostly underwent multilevel ACDF (n=30, 93.8%) involving the C5−6 level (n=15, 46.9%) and subsequent arthroscopic intervention (n=31, 96.9%) for rotator cuff pathology (n=22, 68.8%). Most patients who had shoulder surgery first had isolated rotator cuff tears (n=6, 37.5%) and multiple spine pathologies (n=8, 50.0%). Six (37.5%) of these patients had myelopathy while 8 (50.0%) patients had isolated radicular symptoms. These patients mostly underwent arthroscopic intervention (n=15, 93.8%) for rotator cuff pathology (n=9, 56.3%), and all 16 underwent subsequent multilevel ACDF involving the C5−6 level (Table 2). Patients had an average wait time of 660 days (1.8 years) between initial diagnosis and surgery and 600 days (1.64 years) between index and final surgeries. The average time between surgeries in patients who had spine surgery followed by shoulder surgery was 660 days (1.81 years). The average time between surgeries in patients who had shoulder surgery followed by spine surgery was 673 days (1.84 years).
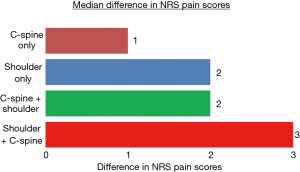
Our analysis yielded no statistical difference between the patients who reported full treatment of shoulder symptoms after only spine surgery (n=6, 40.0%) versus only shoulder surgery (n=34, 37.4%) (P=0.85). Similarly, no statistical difference was found when comparing the decrease in pain scores between patients who underwent only spine (median =1, n=11) operations versus only shoulder (median =2, n=60) operations (P=0.45) (Figure 1). There was also no statistical significance seen in final functional outcome values (FOTO scores and NDI scores) between patients who underwent only spine versus shoulder operations (Table 3). These same patients also showed no statistically significant difference between post-operative opioid use (Figure 2) after only spine surgery (median =2,400 MME) versus after only shoulder surgery (median =825 MME) (P=0.30).
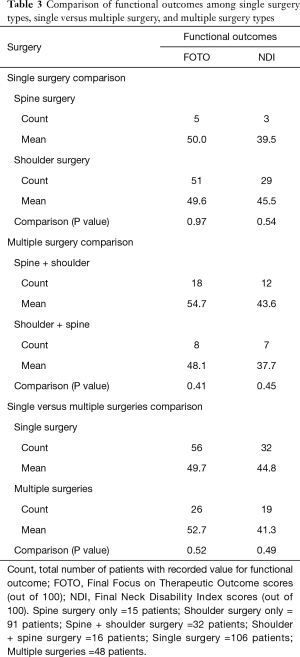
Full table
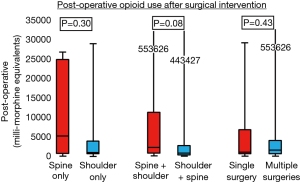
Similarly, there was no statistical difference in subjective reporting of full resolution of shoulder symptoms after spine then shoulder surgery (n=20, 62.5%) versus shoulder then spine surgery (n=10, 62.5%) (P=1.00). Furthermore, there was no statistical significant difference seen when comparing the NRS pain score decreases reported (median=2 in 21 patients versus 3 in 10 patients) pre-operatively to post-operatively between these two cohorts (P=0.37) (Figure 1). These two cohorts also showed no statistically significant difference in either functional outcome (Table 3) or post-operative opioid use (median =2,118.75 MME versus 651.25 MME) (P=0.08) (Figure 2).
Finally, patients who underwent both spine and shoulder operations were significantly more likely to report cessation of shoulder complaints (n=30, 62.5%) than those patients who only underwent one type of operation (n=40, 37.7%) (P=0.004). However, a statistical significant difference was not found when comparing the difference in NRS pain scores reported in patients who only underwent one type of surgery versus both types (P=0.18). These two cohorts also did not show any statistically significant difference in either functional outcome (Table 3) or post-operative opioid use (median =900 MME versus 1,381.25 MME), either (P=0.43) (Figure 2).
Discussion
The clinical course of shoulder pain can often be a long and complicated one, sometimes ending with either multiple surgeries or even chronic symptoms. A thorough and specialized workup (2,3), centered around definitively differentiating between a cervical spine and shoulder etiology (17-19), will help guide the creation and implementation of a curative treatment plan. When the clinical picture is complicated by the presence of both etiologies, the physician must decide which of the pathologies need operative fixation and what order of fixation to follow if multiple surgeries are needed. The mix of subjective and objective outcomes used in this study aim to provide a complete and reliable measure of each operative treatment, a measurement that has been well discussed in the literature (21,22).
Most patients who underwent spine surgery had intervention involving the C5-6 nerve root levels, a trend that follows the levels Campbell et al. reported were most implicated in shoulder complaints (9). Furthermore, the highest success rate in relieving symptoms was seen in patients who underwent repairs of rotator cuff pathology (48.3%) and biceps tendon pathology (42.3%), a pattern that also mirrors the high operative success of these problems reported in the literature (5,23-25).
However, direct statistical comparisons of patient-reported success rates and other functional outcomes after intervention for specific diagnoses (e.g., rotator cuff pathology and spine arthritis) was not undertaken due to low patient counts and an inability to qualify the severity of the two or more concomitant pathologies, both factors that affect how a patient does post-operatively. Instead, the authors thought it more fruitful to only compare full cohorts (e.g. cervical spine surgery only, shoulder surgery only, and both surgeries) and how they progressed post-operatively.
The 37.4% of our patient population that reported full cessation of shoulder symptoms after only shoulder operations falls close to the broad range of 40% to 80% of operative success for rotator cuff tears documented in the literature (23,24). However, there has been no previous literature reporting the cure rate of patient-reported symptoms after cervical spine surgery, giving us no historical control to compare our success rate of 40.0% to. Our results show that these rates of subjective success are statistically similar to one another. Furthermore, the similarities in NRS pain score decreases, functional outcomes, and post-operative opioid use lets the authors believe that surgeons can expect similar recovery and post-operative courses regardless of type of surgery. Range of motion values were not documented secondary to the high rate of inter-provider in testing and measuring absolute degree values. Patients who received multiple surgeries of one type were considered in the same cohort as those who only received a single surgery, as all these patients only had intervention of either the spine or shoulder but not both. Considering patients who had multiple surgeries differently would require an evaluation of initial surgical technique, patient compliance to post-operative guidelines, and incidence of repeat injuries that required surgical treatment.
Similarly, there was no significant differences found in subjective reports of success post-operatively (both 62.5%), NRS pain score decrease, either functional outcome, or opioid use post-operatively between patients who spine surgery first followed by shoulder surgery and patients who had shoulder surgery first followed by spine surgery. As before, these values could be affected by low documentation rates and the unqualified severity of these etiologies, but the lack of significance in all outcomes seems to point to similar efficacies between the two operative treatment orders. In this cohort, the wait time between diagnosis and final surgery (1.8 years) and between final and index surgery (1.6 years) becomes especially important, as prolonged wait time until final surgery has been documented in the literature to negatively affect patient outcomes, especially when spine surgery is involved (26). Further projects should look to stratify subjective success and post-operative outcomes by wait time before surgery between our cohorts, something our study did not do.
Finally, even though our results did show a significantly higher rate of symptom relief in patients who undergo both spine and shoulder surgery versus only one type of surgery, there was no statistically significant difference seen when comparing NRS pain score decrease, functional outcomes, or post-operative opioid use. This difference in results can either be attributed to poor documentation of outcomes or the variability in what patients considered “successful surgery”. Even though the results might point to an operative treatment plan combining both types of surgeries to be superior, the inconclusive results force surgeons to weigh the risks (27,28) and benefits of performing multiple invasive surgeries before proceeding with this complicated but possibly superior treatment plan. Our overall results, based on the work of our multiple fellowship trained surgeons, did not establish superiority of one surgical option over the other, seeming to point to the acceptable use of either cervical spine, shoulder, or both (regardless of order) surgical interventions in the treatment of these complex patients.
The study has a few weaknesses, most inherent to a chart review. Our data hinged on the accuracy of a patient’s chart. Any inaccurate or lack of documentation, patient misrepresentation of the condition of their symptoms, and patients lost to follow-up affected our results. This especially hindered the authors in obtaining a true complication rate due to lack of documentation and follow up. In addition, there may have been intangible reasons why a clinician decided to proceed with a cervical or shoulder surgery that may lead to selection bias. Inter-patient variability in reporting of symptom improvement and NRS pain scores post-operatively must also be taken into consideration. Operative success was also determined by the skill and technique used by the multiple fellowship-trained surgeons involved in this study, with no way to correct for the operative prowess of one surgeon compared to another. Finally, our study centered solely around a suburban population.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was conducted at a suburban Orthopaedic Surgery department after obtaining approval from our Institutional Review Board (IRB).
References
- Virta L, Joranger P, Brox JI, et al. Costs of shoulder pain and resource use in primary health care: a cost-of-illness study in Sweden. BMC Musculoskelet Disord 2012;13:17. [Crossref] [PubMed]
- Self EB. Clinical guidelines for shoulder pain. Orthopaedic Knowledge Update: Shoulder and Elbow 2. 2nd ed. Rosemont, Ill.: American Academy of Orthopaedic Surgeons; 2002: 443-67.
- Iannotti JP, Kwon YW. Management of persistent shoulder pain: a treatment algorithm. Am J Orthop 2005;34:16-23. [PubMed]
- Gumina S, Carbone S, Albino P, et al. Arm squeeze test: a new clinical test to distinguish neck from shoulder pain. Eur Spine J 2013;22:1558-63. [Crossref] [PubMed]
- Dawson J, Harris KK, Doll H, et al. A comparison of the Oxford shoulder score and shoulder pain and disability index: factor structure in the context of a large randomized controlled trial. Patient Relat Outcome Meas 2016;7:195-203. [Crossref] [PubMed]
- van der Heijden GJ. Shoulder disorders: a state-of-the-art review. Baillieres Best Pract Res Clin Rheumatol 1999;13:287-309. [Crossref] [PubMed]
- Radhakrishnan K, Litchy WJ, O'Fallon WM, et al. Epidemiology of cervical radiculopathy: a population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994;117:325-35. [Crossref] [PubMed]
- Foerster O. The dermatomes in man. Brain 1933;56:1-39. [Crossref]
- Campbell CC, Koris MJ. Etiologies of shoulder pain in cervical spinal cord injury. Clin Orthop Relat Res 1996.140-5. [Crossref] [PubMed]
- Tong HC, Haig AJ, Yamakawa K. The Spurling Test and Cervical Radiculopathy. Spine 2002;27:156-9. [Crossref] [PubMed]
- Persson LC, Carlsson CA, Carlsson JY. Long-lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar: a prospective, randomized study. Spine 1997;22:751-8. [Crossref] [PubMed]
- Juel NG, Natvig B. Shoulder diagnoses in secondary care, a one-year cohort. BMC Musculoskelet Disord 2014;15:89. [Crossref] [PubMed]
- Hegedus EJ, Goode A, Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med 2008;42:80-92. [Crossref] [PubMed]
- Kijima H, Minagawa H, Nishi T, et al. Long-term follow-up of cases of rotator cuff tear treated conservatively. J Shoulder Elbow Surg 2012;21:491-4. [Crossref] [PubMed]
- Kuhn JE, Dunn WR, Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg 2013;22:1371-9. [Crossref] [PubMed]
- Chaudhury S, Gwilym SE, Moser JK, et al. Surgical options for patients with shoulder pain. Nat Rev Rheumatol 2010;6:217-26. [Crossref] [PubMed]
- Bokshan SL, DePasse JM, Eltorai AE, et al. An Evidence-Based Approach to Differentiating the Cause of Shoulder and Cervical Spine Pain. Am J Med 2016;129:913-8. [Crossref] [PubMed]
- Stawicki C, Fried T, Mead L, et al. Cervical versus Shoulder/Periscapular Pain. In: Koerner JD, Vaccaro AR, Kim DH. Differential Diagnosis in Spine Surgery. New Delhi: Jp Medical Ltd; 1 edition 2016:52-60.
- Throckmorton TQ, Kraemer P, Kuhn JE, et al. Differentiating cervical spine and shoulder pathology: common disorders and key points of evaluation and treatment. Instr Course Lect 2014;63:401-8. [PubMed]
- Hawkins RJ, Bilco T, Bonutti P. Cervical spine and shoulder pain. Clin Orthop Relat Res 1990.142-6. [PubMed]
- Godil SS, Parker SL, Zuckerman SL, et al. Determining the quality and effectiveness of surgical spine care: patient satisfaction is not a valid proxy. Spine J 2013;13:1006-12. [Crossref] [PubMed]
- McGirt MJ, Speroff T, Godil SS, et al. Outcome science in practice: an overview and initial experience at the Vanderbilt Spine Center. Neurosurg Focus 2013;34:E7. [Crossref] [PubMed]
- Bishop J, Klepps S, Lo IK, et al. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg 2006;15:290-9. [Crossref] [PubMed]
- Boileau P, Brassart N, Watkinson DJ, et al. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 2005;87:1229-40. [PubMed]
- George MS, Khazzam M. Current concepts review: revision rotator cuff repair. J Shoulder Elbow Surg 2012;21:431-40. [Crossref] [PubMed]
- Braybrooke J, Ahn H, Gallant A, et al. The impact of surgical wait time on patient-based outcomes in posterior lumbar spinal surgery. Eur Spine J 2007;16:1832-9. [Crossref] [PubMed]
- Graham JJ. Complications of Cervical Spine Surgery: A Five-Year Report on a Survey of the Membership of the Cervical Spine Research Society by the Morbidity and Mortality Committee. Spine 1989;14:1046-50. [Crossref] [PubMed]
- Weber SC, Abrams JS, Nottage WM. Complications associated with arthroscopic shoulder surgery. Arthroscopy 2002;18:88-95. [Crossref] [PubMed]


