Novel minimally invasive technique in the treatment of cubital tunnel syndrome
Introduction
Cubital tunnel syndrome is the second most common entrapment neuropathy of the upper extremity in the United States (1-3). Incidence per 100,000 person-years of this syndrome is 25 cases in men and 19 cases in women (4). The ulnar nerve travels through the cubital tunnel bordered by the medial epicondyle, the olecranon, and the medial collateral ligament deep, and Osborne’s ligament superficially. The syndrome is maybe brought on by trauma or arthritic changes, but most cases are idiopathic (5). Clinical presentation consists of a combination of weakness, pain, and sensory disturbances ranging from paresthesias and dysesthesias to numbness or complete anesthesia. Sensory and pain findings are present in both dorsal and volar aspects of the medial 4th and entire 5th finger and hypothenar region consistent with the sensory distribution of the ulnar nerve. Motor findings are weakness with 4th and 5th finger flexion and finger abduction and adduction with atrophy, paralysis, and claw deformity in more severe cases. Symptoms are commonly worsened by flexion of the elbow as Osborne’s ligament is pulled taut causing further compression against the medial collateral ligament deep to the nerve. The prevalence of the condition and its shared treatment by multiple surgical specialties has led to the development of a variety of surgical techniques and approaches with the consensus as to the appropriate standard of care remaining elusive. Most current techniques fall predominantly into two categories: in situ decompression and ulnar nerve transposition. In situ techniques were done fully open initially but are now often being done with smaller incisions and endoscopic techniques to minimize recovery time and improve outcomes.
Here, we propose a novel technique of addressing ulnar compression in the cubital tunnel utilizing nerve decompression with proximal direct visualization and more distal line dissection to achieve maximum efficacy with minimal complications and minimizing the total incision size to a modest 1–2 cm. Despite the many techniques used today, with none of them demonstrating superiority, we hypothesize that we can achieve the benefits of a minimally invasive approach and distal dissection while minimizing complication rates, all without the need for endoscopes and the associated training, equipment, and maintenance costs required for such systems.
Indications/contraindications
This technique was considered indicated for intractable cases of McGowan grades: I, sensory alone; II, muscle weakness; and III, paresis and/or wasting of the involved muscles (6). Patient symptomatology was unresponsive to conservative means, including medical management and physical therapy. There were no absolute contraindications for the procedure.
Methods
Study methods
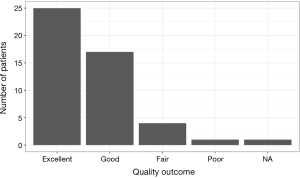
All patients with cubital tunnel syndrome were diagnosed clinically without the use of advanced diagnostic testing. Those that failed conservative therapy with physical therapy and symptomatic management underwent the described procedure. Interviews and physical exams were conducted on patients with a median follow-up time of 23 days postoperatively (mean =30.36±26.37 days). Strength, vibratory sense, proprioception, and pain/temperature were assessed on physical exam. Patients were graded during standard post-operative follow-up visits based on the Gabel/Amadio scale (7) of pre- and post-operative symptomatology and degree of improvement and assigned to poor, fair, good, or excellent outcomes accordingly (Table 1).
Full table
All procedures were performed by a single surgeon and first assistant at several hospital sites with similar facilities and available equipment, and all data collected in a retrospective manner. Institutional Review Board (ID: PDRUNSG) approval and necessary patient consents were obtained for this study.
Surgical method
The patient is placed on the operative table in a supine position. General anesthesia is obtained. The procedure can also be done using local anesthesia, with or without sedation. The entire upper extremity is then prepped and draped in the usual sterile fashion.
A 15-blade knife is then used to make a 1–2-cm incision just below the medial epicondyle. The skin edges are pulled apart with Adson forceps while the initial layer of soft tissue is divided with Bovie (Bovie Medical, Purchase, New York, USA) electrocautery. Metzenbaum scissors are then used to carefully descend upon the ulnar nerve with both sharp and blunt dissection. Bipolar forceps are used to coagulate any small veins that bleed. Once the ulnar nerve is identified, a small Ohm’s retractor is inserted and a Senn retractor is used to pull the skin edges initially proximally, then distally to increase the direct visual exposure of the ulnar nerve. Metzenbaum scissors are bluntly inserted along the course of the nerve approximately 8 cm proximally and distally and spread out to open any constrictions on the ulnar nerve. Tight areas are divided sharply with the Metzenbaum scissors under direct visualization. We did not encounter significant compression far from our entry site that has limited the ability of the blind blunt dissection from safely dilating the space around the nerve.
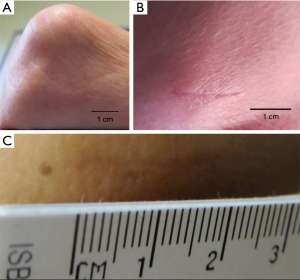
The wound is then irrigated with Bacitracin solution. The skin edges are closed with a simple interrupted inverted dermis/subcuticular layer of 3.0 Vicryl (Ethicon, Somerville, New Jersey, USA). Dermabond (Ethicon, Somerville, New Jersey, USA) glue is then placed over the incision (Figure 1). The patient is taken to the recovery room and subsequently discharged.

Patients are allowed regular activity without restriction immediately, no immobilization is required. Patients return for post-operative evaluation in three weeks and subsequently only as needed. Physical therapy and occupational therapy are recommended only to patients with significant residual weakness at this time.
Results
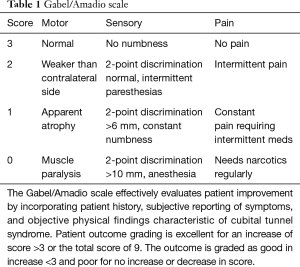
A total of 48 procedures were performed on 41 unique patients. All patients undergoing the procedure during a 5-year period from January 2012 to January 2017 were included in the study. Five patients had bilateral procedures. Twenty-two left arms and 26 right arm procedures were performed. Average patient age was 60.52 years (SD: ±12.18 years), there were 34 (72.3%) males and 1 patient was lost to follow-up.
All study patients reported subjective improvement of ulnar neuropathic symptoms. Patient outcomes were measured by the Gabel/Amadio Scale, taking into account sensory, motor, and pain related symptomatology (Table 1). The average preoperative score was 4.89±1.26, and the average postoperative score was 7.83±1.00 (Table 2). There was an average improvement in score of 2.93±1.22 coinciding with improvements of “good” to “excellent” in all patients (Figure 2). The largest clinical improvements were the reduction of frequency, character, and intensity of pain. All patients experienced complete resolution of pain resulting from ulnar neuropathy. Numbness in the ulnar distribution was the most common residual symptom postoperatively. However, these patients report these instances continuing to decrease in frequency and intensity at the time of follow-up.
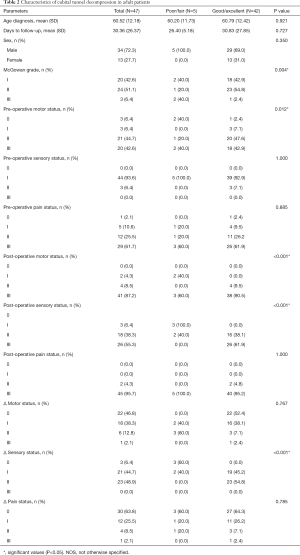
Full table
There were no intraoperative or postoperative complications, including infection, or significant new pain or numbness at the incision site. No patients experienced new-onset of or worsening of any symptoms of ulnar neuropathy. There were no instances of hematoma or neuroma formation. Scar formation at the incision site was minimal (Figure 3), with complete patient satisfaction with postoperative aesthetics of the scar.
Discussion
Surgical management of cubital tunnel syndrome encompasses a variety of techniques with generally high efficacy with no single procedure demonstrating a significant advantage (2,8,9). We propose a novel relatively simple technique utilizing minimally invasive decompression under direct visualization to maximize clinical improvement, minimize complications, and provide the highest level of patient satisfaction through a less painful and more rapid recovery.
Historically there have been several widely accepted techniques for treating cubital tunnel syndrome, each with specific advantages and disadvantages. The earliest techniques, open in situ decompression and anterior transposition, demonstrated good outcomes but require a great deal of tissue dissection and large incisions. In 1981, Foster and Edshage (10) found equivalent outcomes between anterior transposition and open decompression surgeries for overall outcome but a better intrinsic muscle function return was noted in the transposition group. Gervasio et al. (11) [2005] found no statistically significant difference between submuscular transposition and open decompression with good to excellent outcomes in 82.86% and 80% of patients respectively, using Bishop scores. Another study by Bartels et al. (8) [2005] demonstrated that 65.3% of patients undergoing simple decompression and 70.1% of patients with subcutaneous transposition showed excellent to good results, albeit this was not statistically significant. However, patients undergoing subcutaneous transposition showed a significantly greater complication rate (31.1%) compared to those with the simple decompression surgery (9.6%). Still, in 2014, Sousa et al. (12) found no significant difference between subcutaneous anterior transposition with 69.7% of patients and open decompression with 67.2% of patients having good to excellent outcomes on the Wilson and Krout scale (13). In both techniques, the benefit of direct visualization along the entire course of dissection must be weighed against the large incision with the accompanying trauma to local tissues. Transposition also carries with it the risk of disrupting the blood supply to the nerve.
Like many surgical procedures, over time the natural progression has been towards minimally invasive approaches to decrease the size of incisions and degree of local tissue trauma. This resulted in the subsequent development of endoscopic and minimal incision techniques.
In 1995, Tsai et al. (14) described a new endoscopic technique for cubital tunnel syndrome, and in 1999, studied outcomes in 85 procedures (76 patients) and found 87.06% had good or excellent outcomes using Bishop scores (15). Cobb et al. (16) [2010] demonstrated good to excellent results in 94% of 104 procedures (94 patients) using Bishop scores. This study had a mean follow-up time of 736 days which allows for much more healing and resultantly improved outcomes when compared with scoring done at a short-term post-operative visit as in our study. Mirza et al. (17) [2014] showed good to excellent outcomes in 69.57% of 80 patients (92 procedures) utilizing the same Gabel/Amadio scale as in our study. Dützmann et al. (18) [2013] compared endoscopic and open decompressions finding that long-term outcomes were equal between both groups but that short-term results were significantly better with the endoscopic technique. This short-term benefit is likely due to the benefit of using a smaller incision resulting in a faster recovery. In 2015, Schmidt et al. (19) compared endoscopic and open techniques, finding no significant difference with 81.5% of open and 82.8% of endoscopic patients having good or excellent results using Bishop scores. They did note a statistically significant increase in postoperative hematoma formation in the endoscopic group compared to the open group.
In 2002, Taniguchi et al. (20) described a small incision technique without the use of endoscopes. They demonstrated good to excellent results in 77.8% of 17 patients using a Messina classification (21). This study was limited by its small sample size but was encouraging that endoscopes may not be necessary for a minimally invasive approach. In 2007, Cho et al. (21) compared endoscopic with open decompression and found no significant difference between the two groups, although this study was limited by small sample size. Karthik et al. (22) [2012] studied 30 patients (46 procedures) finding an 80% rate of good to excellent outcomes according to Bishop scores. A recent study by Vanaclocha et al. (23) [2017] found that patients undergoing in situ decompression reported higher Bishop Scores (7.50±1.74) compared to those receiving anterior transposition surgery (6.12±1.75). These studies suggested that it might be possible to achieve the benefits of a minimally invasive approach without the need for all of the training and expenses associated with the use of endoscopes.
Only one study, Bolster et al. (24) [2013], has compared endoscopic and minimal incision techniques. In a study of 60 patients, they found a good to excellent outcome rate of 90.91% in the endoscopic group and 93.40% in the minimal incision group, but this difference was not significant. In a large retrospective multi-center study of 375 patients conducted by Bacle et al. (2) [2013] four of the present surgical techniques (open or endoscopic in situ decompression, or subcutaneous or submuscular anterior transposition) were compared at a mean follow-up time of 92 months post-operation. None of the procedure showed a significant advantage over the others, with more than 90% of the patients reporting an improvement in their symptoms with minimal long-term complications and recurrences. Once again, even with the development of new techniques, there is still not one clearly superior method for the surgical treatment of cubital tunnel syndrome.
Our study had an 89.4% good to excellent outcome rate using the Gabel/Amadio score for our new technique, demonstrating effectiveness similar to that of other techniques widely used at the present. While these results are not directly comparable in a quantitative sense to Bishop scores, Wilson and Krout, and Messina scores used in most of the previous studies, the use of qualitative “good” and “excellent” outcomes are likely comparable to some extent. With good and excellent improvement in a majority of patients, this procedure matches the most highly effective existing surgical management for cubital tunnel syndrome. In particular, minimally invasive simple decompression appears to be most effective at addressing pain and other sensory changes with incomplete improvement in motor symptoms. However, it should be noted that the efficacy of resolution of motor symptoms is difficult to determine due to the sample size and length of follow-up in this study. The authors expect that improvement in patients to continue with more time, as it has been documented that recovery from muscular weakness and atrophy may continue beyond 2 years postoperatively (16). Of note, 5 patients received bilateral ulnar decompression procedures.
Patients with more severe preoperative disease experienced relatively similar improvement measured by the Gabel/Amadio Scale to those of less severe symptoms but were less likely to experience complete resolution of symptoms. These results match efficacy seen in endoscopic techniques (25). However, the additional equipment and training required for endoscopic techniques are not necessary.
The lack of complications in our study suggests the safety of the procedure and acts as a point of comparison to existing options. More aggressive techniques have been associated with pain and numbness at the elbow possibly resulting from damage to the medial antebrachial cutaneous nerve, or instability or subluxation of the ulnar nerve (25). While the lack of direct visualization during the process of scissor insertion along the nerve may theoretically create greater potential for nerve injury when compared with endoscopic or open approaches, no nerve injuries have occurred to date with this technique.
Limitations of this study include the non-standard score scale amongst comparative studies and low patient number and relatively short follow-up time as the literature has demonstrated the need for extended follow-up time for full symptomatic improvement to become evident. The ability to assess long-term outcomes is of great significance in evaluating the efficacy of surgical procedures, and as such further studies are required with a longer follow-up period which may better capture treatment failure. As a result, the results for post-operative improvement cannot be definitively described for patients with variable demographics, comorbidities, or severity of pre-operative cubital tunnel syndrome symptomatology. However, the preliminary results thus far are extremely encouraging and suggest that it is reasonable to consider using the described technique with hopes of achieving the best patient outcomes.
Conclusions
This minimally invasive procedure is a refinement of existing techniques, providing the highest efficacy for symptom relief, maximizing avoidance of complications, allowing rapid recovery, and improving patient satisfaction. In addition, we assert that this technique is more cost effective than endoscopic surgical options by elimination of expensive extra equipment and shorter operative time.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board (ID: PDRUNSG) approval and necessary patient consents were obtained for this study.
References
- Ahcan U, Zorman P. Endoscopic decompression of the ulnar nerve at the elbow. J Hand Surg Am 2007;32:1171-6. [Crossref] [PubMed]
- Bacle G, Marteau E, Freslon M, et al. Cubital tunnel syndrome: comparative results of a multicenter study of 4 surgical techniques with a mean follow-up of 92 months. Orthop Traumatol Surg Res 2014;100:S205-8. [Crossref] [PubMed]
- Seror P, Nathan PA. Relative frequency of nerve conduction abnormalities at carpal tunnel and cubital tunnel in France and the United States: importance of silent neuropathies and role of ulnar neuropathy after unsuccessful carpal tunnel syndrome release. Ann Chir Main Memb Super 1993;12:281-5. [Crossref] [PubMed]
- Staples JR, Calfee R. Cubital Tunnel Syndrome: Current Concepts. J Am Acad Orthop Surg 2017;25:e215-24. [Crossref] [PubMed]
- Waugh RP, Zlotolow DA. In situ decompression of the ulnar nerve at the cubital tunnel. Hand Clin 2007;23:319-27. vi. [Crossref] [PubMed]
- McGOWAN AJ. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg Br 1950;32-B:293-301. [Crossref] [PubMed]
- Gabel GT, Amadio PC. Reoperation for failed decompression of the ulnar nerve in the region of the elbow. J Bone Joint Surg Am 1990;72:213-9. [Crossref] [PubMed]
- Bartels RH, Verhagen WI, van der Wilt GJ, et al. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery 2005;56:522-30; discussion 522-30. [Crossref] [PubMed]
- Keiner D, Gaab MR, Schroeder HW, et al. Comparison of the long-term results of anterior transposition of the ulnar nerve or simple decompression in the treatment of cubital tunnel syndrome--a prospective study. Acta Neurochir (Wien) 2009;151:311-5; discussion 316. [Crossref] [PubMed]
- Foster RJ, Edshage S. Factors related to the outcome of surgically managed compressive ulnar neuropathy at the elbow level. J Hand Surg Am 1981;6:181-92. [Crossref] [PubMed]
- Gervasio O, Gambardella G, Zaccone C, et al. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery 2005;56:108-17; discussion 117. [Crossref] [PubMed]
- Sousa M, Aido R, Trigueiros M, et al. Cubital compressive neuropathy in the elbow: in situ neurolysis versus anterior transposition - comparative study. Rev Bras Ortop 2014;49:647-52. [Crossref] [PubMed]
- Wilson DH, Krout R. Surgery of ulnar neuropathy at the elbow: 16 cases treated by decompression without transposition. Technical note. J Neurosurg 1973;38:780-5. [Crossref] [PubMed]
- Tsai TM, Bonczar M, Tsuruta T, et al. A new operative technique: cubital tunnel decompression with endoscopic assistance. Hand Clin 1995;11:71-80. [PubMed]
- Tsai TM, Chen IC, Majd ME, et al. Cubital tunnel release with endoscopic assistance: results of a new technique. J Hand Surg Am 1999;24:21-9. [Crossref] [PubMed]
- Cobb TK. Endoscopic cubital tunnel release. J Hand Surg Am 2010;35:1690-7. [Crossref] [PubMed]
- Mirza A, Reinhart MK, Bove J, et al. Scope-assisted release of the cubital tunnel. J Hand Surg Am 2011;36:147-51. [Crossref] [PubMed]
- Dützmann S, Martin KD, Sobottka S, et al. Open vs retractor-endoscopic in situ decompression of the ulnar nerve in cubital tunnel syndrome: a retrospective cohort study. Neurosurgery 2013;72:605-16; discussion 614-6. [Crossref] [PubMed]
- Schmidt S, Kleist Welch-Guerra W, Matthes M, et al. Endoscopic vs Open Decompression of the Ulnar Nerve in Cubital Tunnel Syndrome: A Prospective Randomized Double-Blind Study. Neurosurgery 2015;77:960-70; discussion 970-1. [Crossref] [PubMed]
- Taniguchi Y, Takami M, Takami T, et al. Simple decompression with small skin incision for cubital tunnel syndrome. J Hand Surg Br 2002;27:559-62. [Crossref] [PubMed]
- Cho YJ, Cho SM, Sheen SH, et al. Simple decompression of the ulnar nerve for cubital tunnel syndrome. J Korean Neurosurg Soc 2007;42:382-7. [Crossref] [PubMed]
- Karthik K, Nanda R, Storey S, et al. Severe ulnar nerve entrapment at the elbow: functional outcome after minimally invasive in situ decompression. J Hand Surg Eur Vol 2012;37:115-22. [Crossref] [PubMed]
- Vanaclocha V, Blanco T, Ortiz P, et al. Can We Make Simple In Situ Decompression of the Ulnar Nerve at the Elbow Still Easier? World Neurosurg 2017;107:908-924.e2. [Crossref] [PubMed]
- Bolster MA, Zöphel OT, van den Heuvel ER, et al. Cubital tunnel syndrome: a comparison of an endoscopic technique with a minimal invasive open technique. J Hand Surg Eur Vol 2014;39:621-5. [Crossref] [PubMed]
- Damert HG, Altmann S, Infanger M, et al. Operative decisions for endoscopic treatment of cubital tunnel syndrome. Orthopedics 2013;36:354-9. [Crossref] [PubMed]