The prevalence of Klippel-Feil syndrome in pediatric patients: analysis of 831 CT scans
Introduction
Klippel-Feil syndrome (KFS) is characterized by congenital fusion of cervical vertebrae as a result of incomplete cervical segmentation during embryonic development. The term was first used in 1912, by Andre Feil and Maurice Klippel, in a medical school thesis on cervical abnormalities (1-3). KFS is thought to be the result of a genetic mutation in one of the following genes: growth differentiation factor (GDF) 6 or 3 (autosomal dominant) or mesenchyme homeobox (MEOX) 1 (autosomal recessive) (4,5). The GDF genes are both associated with the transforming growth factor beta (TGF-β) family of proteins. GDF6 is associated with growth and maturation of bone and cartilage, whereas GDF3 is known to play a role in ocular and skeletal development. The MEOX1 gene has been shown to play a significant role in somitogenesis; and MEOX1 mutations have displayed similar Klippel-Feil findings in knockout mice (5). Phenotypically, KFS has been associated with a ‘clinical triad’, consisting of a short neck, a low posterior hairline, and a decreased range of cervical motion; however, studies have shown that less than 50% of KFS patients present with all 3 features (3,6).
KFS has also been shown to be associated with numerous skeletal defects and other anomalies (2,7-9). Common skeletal findings include Sprengel deformity (congenital elevated scapula) and scoliosis. Somite defects include anomalies within the urogenital system, cardiovascular system and deafness. A widely held concern regarding fused segments amongst the cervical vertebrae, is the resultant pressure or increased force on the adjacent mobile segments. It has been postulated that subsequent hypermobility of these adjacent segments could lead to advanced degenerative changes causing cervical myelopathy and neurologic injury (10,11).
The objective of this study was to evaluate the prevalence of KFS among pediatric patients undergoing cervical CT imaging in an emergency room (ER) setting over a 3-year period.
Methods
Data source
After obtaining Institutional Review Board approval we evaluated CT scans of the cervical spine of pediatric patients treated in the Emergency Department (ED) of a level I pediatric trauma center between January 2013 and the end of December 2015 (12). An institutional administrative database was queried to identify patients undergoing cervical CT scans during the study period Our inclusion criteria were patients ages 0–<19 with CTs of the cervical spine that included all seven cervical vertebrae. If multiple cervical spine CT scans for the same patient were identified, only the first CT scan was included.
The following demographics were collected: age, sex, race and ethnicity. The mechanism of injury leading to the ER visit was also collected.
The CT scans were analyzed for KFS, by examining sagittal and coronal CT images. For every patient with KFS, the cervical congenital fusion was further classified using Samartzis classification, which categorizes the type of KFS by order and number of fused segments. Type I KFS patients demonstrate a single fused segment; type II KFS—multiple noncontiguous fused segments; and type III KFS—multiple contiguous fused segments (1). The wasp-waist sign which alludes to the narrowing on a lateral or sagittal image of the midpoint of the congenital cervical fusion was also used to confirm the presence of KFS (11,13). All CT scans of patients with presumed KFS were evaluated again by the senior author.
Results
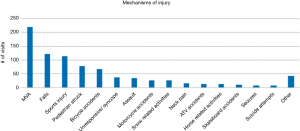
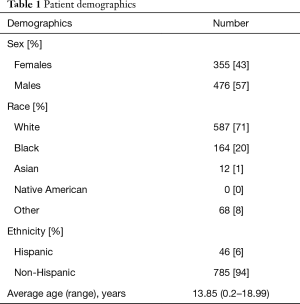
There were 848 pediatric cervical CTs obtained at Strong Memorial Hospital, between January 2013 and December 2015. Of these, 831 CTs met our inclusion criteria. There were 355 females (43%) and 476 males (57%). The average age was 13.85 years old, (range, 0.2–18.99 years). Race and ethnicity demographics were also recorded (Table 1). The primary mechanism of injury for ED visits was motor vehicle accidents or collisions, accounting for 220 patient visits (26%). Falls (15%), sports injuries (14%) and pedestrian struck (10%) accounted for the remainder (Figure 1). Of all sports injuries, football related injuries were the most common (n=38 patients, 35%).
Full table
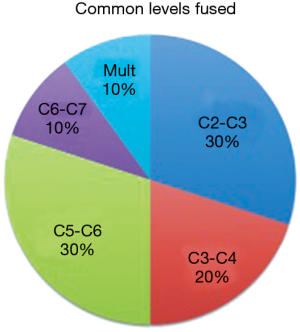
Ten patients were found to have KFS, for a prevalence of 1.2% (or approximately 1 in 83). According to the Samartzis classification, 9 had type I (single level fusion), and 1 type III (multiple contiguous level fusion). The average age was 16.02 years old (range, 10–18 years), with 8 males (80%) and 2 females (20%). The most common mechanism of injury reported for the KFS patients was sports injury, accounting for 30%. Demographics were collected for all KFS patients (Table 2). Three had congenital fusions at vertebral levels C2–C3, two at C3–C4, three at C5–C6, one at C6–C7, and one with multiple levels of cervical fusion (Figure 2).

Full table
Discussion
There have not been any previous studies assessing the prevalence of KFS in large cohorts of pediatric patients. Since the first report in 1912, KFS has been described as a rare bone disorder, and has been stated to have an incidence of 1 in 42,000 live births, with females representing 60% of cases (2,6). Other authors have demonstrated higher prevalence rates, up to 0.71% (14-16). Although studies have tried to further characterize KFS and its association with various somitic anomalies, there is little information on its true prevalence. Associations between congenital cervical fusion and risk of adjacent segment degeneration, instability and injury to the cervical spine following trauma have been reported (10,11,17). As a result, patients with KFS demonstrating signs/symptoms of radiculopathy or myelopathy should be monitored closely.
In this study, all cervical CT scans of pediatric patients treated at the ED of a Level I Trauma Center between January 2013 and December 2015 were evaluated. The demographics of the patients including race and ethnicity, did not differ significantly from that of the geographic region where the trauma center was located (18). Of the 831 CT scans that met inclusion criteria, 10 were found to be associated with KFS, for a prevalence of 1.2% or approximately 1 in 83. Eighty percent of cases were of males, whereas 20% were of females. The two most common levels fused were C2–C3 (30%) and C5–C6 (30%). According to the Samartzis classification, 9 were type I, and 1 type III. Only one patient had KFS listed as a known diagnosis in their medical record. As this study was a retrospective review of CT images, and no physical examination was performed, no clinical findings referable to KFS are available.
Although congenital cervical fusions were termed KFS in 1912, previous research indicated the findings of KFS to be present much earlier. An Egyptian mummy, from approximately 500 B.C., was found to have a fusion between C2 and C3 vertebrae (19). The pre-Hispanic population of El-Hierro were also found to have features of KFS, specifically fusions at C2–C3 and C5–C6 vertebrae (20). Along with fused cervical vertebrae, these earlier cases demonstrated associated anomalies, including scoliosis, cervical spina bifida, and restricted cervical mobility (19,20). Skeletal and non-skeletal abnormalities, such as these, have been noted in several studies on KFS. Larson et al. reported Sprengel deformity in 30% of patients with KFS, with 9–12% having an omovertebral bone (7). Scoliosis has been documented as being seen in more than 50% of KFS patients (9). Although an association with a “clinical triad” was established, it has been stated that the clinical triad is expected to be found in less than 50% of KFS cases (3,6). Based on a retrospective study completed on 31 KFS patients, less than 10% presented with the clinical triad. A proportion of 38.7% were found to have only one of the three findings, with the primary finding being limited cervical range of motion, seen in 64.5% of patients (6). In his study, Samartzis et al. also postulated that the extent of cervical fusion might affect the phenotype of the clinical triad. Gray et al. noted that a single level cervical fusion did not increase the risk of developing limited cervical mobility (21). In a study following 28 KFS patients for an average of 8 years, Samartzis et al. noticed that patients with type II or III KFS were more likely to develop radiculopathy or myelopathy (1).
Although the true incidence of KFS is still unknown, the majority of the literature quotes it to be around 1 in 42,000 (2,6). Our study found a much higher prevalence rate of 1 in 83 pediatric patients, or 1.2%. This prevalence is much closer to a study of an osseous collection completed in 1964, which reported a 0.71% incidence of congenital cervical fusion (14). Another study using either radiographic imaging incidence rates of 0.2 and 0.5 per 1,000 (6). Investigators at our institution reviewed 3,000 adult cervical CT scans from the ER and found a KFS incidence of 1 in 177 or 0.56% (16).
The vertebral levels involved and number of fused segments in a KFS patient have been shown to be associated with extent of cervical degeneration and myelopathy in the future (10,11,17). The most common levels fused in our study were C2–C3 and C5–C6 (Figure 3A,B). This coincides with previous literature stating that C2–C3 is the most common site for cervical fusion. Type III Samartzis classification patients (Figure 3C), are said to need early diagnosis, especially when involved in high-impact athletic activities (6,10). Cervical fusions, such as seen in Klippel-Feil, increase the risk for hypermobility, disc herniation, and degenerative changes to the adjacent levels. Given certain circumstances, this could lead to traumatic instability, cord compression and neurologic damage (10,17). Furthermore, research has shown a higher prevalence of KFS in patients with degenerative cervical myelopathy, suggesting KFS is a risk factor (11).

The clinical relevance of this study is the need to establish a pathway for follow up once a pediatric patient has been identified with a congenital cervical fusion. Patients may have a congenital cervical fusion without the other signs or conditions associated with KFS. However, with a prevalence of 1 in 83 ER cervical CT scans it may be appropriate for the pediatrician following the patient on out-patient basis to refer the patient to orthopaedic surgery, if the patient develops neck pain or decreased range of motion. If the orthopaedic or neurosurgery team is consulted on the patient in the ER then appropriate follow-up can also be established.
In studying a rare condition, such as KFS, there are various limitations. As a retrospective study, our data was limited to only the CT scans made available within the time period. This also prevented us from studying phenotypic associations, such as limited cervical mobility, of KFS to assess severity. Although our sample was one of the largest pediatric cohorts studied for KFS, it was still relatively small given a preconceived frequency of 1 in 42,000. As a result, our ability to examine statistical significance and draw larger conclusions, was limited. All of our data was gathered at the ED of a single center, making it hard to extrapolate our data to other populations. The nature of our study requires patients presenting to the ER, as well as those patients receiving a diagnosis that requires a CT, which also limits our sample size. Within the sample, we also had more males than females, which may be justified in view of research stating that boys take part in riskier behavior and sustain more severe injuries, thus warranting more ER visits (22). This fact makes it difficult to prove a correlation between gender and KFS prevalence.
Conclusions
KFS is a rare bone disorder, characterized by congenital cervical fusion, the prevalence of which is still unknown. In our study of 831 pediatric cervical CT scans, 10 patients were found to have KFS. This prevalence of 1.2% is higher than previously reported. Moving forward, KFS patients should be monitored longitudinally for possible development of cervical spine related symptoms. Given the evidence regarding KFS and its likely association with progressive degenerative cervical myelopathy and traumatic instability, KFS patients should be monitored closely.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of University of Rochester (No. STUDY0001098).
References
- Samartzis DD, Herman J, Lubicky JP, et al. Classification of congenitally fused cervical patterns in Klippel-Feil patients: epidemiology and role in the development of cervical spine-related symptoms. Spine (Phila Pa 1976) 2006;31:E798-804. [Crossref] [PubMed]
- Paradowska A, Szelag J, Slawecki K. Klippel-Feil syndrome - Review of the literature. Dent Med Probl 2007;44:491-4.
- Bejiqi R, Retkoceri R, Bejiqi H, et al. Klippel - Feil Syndrome Associated with Congential Heart Disease Presentaion of Cases and a Review of the Curent Literature. Open Access Maced J Med Sci 2015;3:129-34. [PubMed]
- Tassabehji M, Fang ZM, Hilton EN, et al. Mutations in GDF6 are associated with vertebral segmentation defects in Klippel-Feil syndrome. Hum Mutat 2008;29:1017-27. [Crossref] [PubMed]
- Bayrakli F, Guclu B, Yakicier C, et al. Mutation in MEOX1 gene causes a recessive Klippel-Feil syndrome subtype. BMC Genet 2013;14:95. [Crossref] [PubMed]
- Samartzis D, Kalluri P, Herman J, et al. "Clinical triad" findings in pediatric Klippel-Feil patients. Scoliosis Spinal Disord 2016;11:15. [Crossref] [PubMed]
- Larson AR, Josephson KD, Pauli RM, et al. Klippel-Feil anomaly with Sprengel anomaly, omovertebral bone, thumb abnormalities, and flexion-crease changes: novel association or syndrome? Am J Med Genet 2001;101:158-62. [Crossref] [PubMed]
- Fernandes T, Costa C. Klippel-Feil syndrome with other associated anomalies in a medieval Portuguese skeleton (13th-15th century). J Anat 2007;211:681-5. [Crossref] [PubMed]
- Mesfin A, Bakhsh WR, Chuntarapas T, et al. Cervical Scoliosis: Clinical and Radiographic Outcomes. Global Spine J 2016;6:7-13. [Crossref] [PubMed]
- Samartzis D, Lubicky JP, Herman J, et al. Symptomatic cervical disc herniation in a pediatric Klippel-Feil patient: the risk of neural injury associated with extensive congenitally fused vertebrae and a hypermobile segment. Spine (Phila Pa 1976) 2006;31:E335-8. [Crossref] [PubMed]
- Nouri A, Martin AR, Lange SF, et al. Congenital Cervical Fusion as a Risk Factor for Development of Degenerative Cervical Myelopathy. World Neurosurg 2017;100:531-9. [Crossref] [PubMed]
- New York State Department of Health. New York State Trauma Centers. Available online: https://www.health.ny.gov/professionals/ems/state_trauma/trauma2.htm. Accessed August 9, 2017.
- Nguyen VD, Tyrrel R. Klippel-Feil syndrome: patterns of bony fusion and wasp-waist sign. Skeletal Radiol 1993;22:519-23. [Crossref] [PubMed]
- Brown MW, Templeton AW, Hodges FJ 3rd. The incidence of acquired and congenital fusions in the cervical spine. Am J Roentgenol Radium Ther Nucl Med 1964;92:1255-9. [PubMed]
- Clarke RA, Catalan G, Diwan AD, et al. Heterogeneity in Klippel-Feil syndrome: a new classification. Pediatr Radiol 1998;28:967-74. [Crossref] [PubMed]
- Gruber J, Saleh A, Bakhsh W, et al. The Prevalence of Klippel-Feil Syndrome: A Computed Tomography-Based Analysis of 2,917 Patients. Spine Deform 2018;6:448-53. [Crossref] [PubMed]
- Samartzis D, Kalluri P, Herman J, et al. 2008 Young Investigator Award: The role of congenitally fused cervical segments upon the space available for the cord and associated symptoms in Klippel-Feil patients. Spine (Phila Pa 1976) 2008;33:1442-50. [Crossref] [PubMed]
- US Census Bureau. Available online: https://www.census.gov/quickfacts/fact/table/monroecountynewyork/RHI125216. Accessed June 29, 2017.
- Saker E, Loukas M, Oskouian RJ, et al. The intriguing history of vertebral fusion anomalies: the Klippel-Feil syndrome. Childs Nerv Syst 2016;32:1599-602. [Crossref] [PubMed]
- González-Reimers E, Mas-Pascual A, Arnay-De-La-Rosa M, et al. Klippel-Feil syndrome in the prehispanic population of El Hierro (Canary Islands). Ann Rheum Dis 2001;60:174. [Crossref] [PubMed]
- Gray SW, Romaine CB, Skandalakis JE. Congenital fusion of the cervical vertebrae. Surg Gynecol Obstet 1964;118:373-85. [PubMed]
- Morrongiello BA, Rennie H. Why do boys engage in more risk taking than girls? The role of attributions, beliefs, and risk appraisals. J Pediatr Psychol 1998;23:33-43. [Crossref] [PubMed]