
Minimally invasive stabilization for thoracolumbar and lumbar fractures: a comparative study with short segment open Schanz screw constructs
Introduction
Fractures of the thoracolumbar and lumbar spine most commonly affect the thoracolumbar junction with the majority (50–78%) of patients being neurologically intact (1). The goal of fracture treatment primarily is to obtain and maintain a stable reduction that leads to early mobilisation and, ultimately, union and satisfactory function. A secondary aim is to restore sagittal alignment which has gained increasing emphasis in the last decade. The impetus for this study is that there is ongoing controversy regarding management of these fractures without neurological impairment and minimally invasive techniques are becoming commonplace in spinal practice, often without comparison of outcomes to existing gold standard techniques.
Our institution has been managing unstable thoracolumbar and lumbar fracture with short segment internal fixation without fusion using open transpedicular Schanz Screw system for the past 30 years. The Schanz screw system has long lever arm that can be used to correct posttraumatic kyphosis and offer great rigidity of construct once secured. Originally designed for treating degenerative diseases, minimally invasive spine surgery techniques utilizing percutaneous pedicle screw have been progressively introduced for treatment of thoracolumbar and lumbar fractures. Multiple comparative case series have suggested that there may be an advantage in the management of these injuries using minimally invasive techniques (2,3), but the main disadvantage of minimally invasive systems have been the reduced angular stability of polyaxial screws resulting in a lesser potential to correct posttraumatic kyphotic deformity. To address this, we started using combined monoaxial and polyaxial screws in our fixation construct inserted percutaneously.
The aim of this study was to compare radiographic and clinical indices of open Schanz screw fixation to MIS fixation with monoaxial-polyaxial screw constructs for thoracolumbar and lumbar fractures. Primary outcomes were the correction of fracture angulation and percentage loss of reduction until fracture union.
Methods
A retrospective review of case notes, radiographs and operative records was performed on patients with thoracolumbar and lumbar fractures who underwent short segment internal fixation using minimally invasive percutaneous pedicle screws-rods construct and open transpedicular Schanz screw-rod construct without decompression between July 2014–July 2017. Study inclusion was limited to neurologically intact patients with non-pathological, unstable thoracolumbar and lumbar fracture. None of the patients had additional decompressive procedure. All patients provided informed consent for their radiological and clinical data to the utilised for research purposes.
Patient demographic characteristics including gender, age, fracture level, Thoracolumbar Injury Classification and Severity (TLICS) score were collected. Fracture characteristics were assessed on CT scan and classified using McCormack Load Sharing Classification of Spine (4) and the AO Spine Classification for thoracolumbar fractures. Perioperative information collected included operating time, pre- and post-operative haemoglobin, radiation dose, postoperative length of stay (excluding poly trauma patients whose length of stay may have been affected by other injuries) and complications. Radiographic data acquisition was performed pre-, intra-, post-operatively and at final review at 9 months. The main radiographic parameter of interest was the bi-segmental Cobb angle, defined as the angle between a line drawn parallel to the superior endplate of one vertebra above the fracture, and a line drawn parallel to the inferior endplate of the vertebra below the fracture. Pre-operative measurements were on supine radiographs, which gave the value for preoperative kyphotic deformity measurements. This is compared with on table fluoroscopic images, which give the value of extent of correction. Erect lateral radiographs postoperatively were assessed at two time periods: prior to patient discharge, which was, on average, 3 days post-operatively and at final follow-up, which assessed the loss of reduction over time. To assess the loss of vertebral body reduction over time, vertebral body angles were assessed for collapse by measuring the angles subtended by the superior and inferior end plates between three time periods: pre-operatively on computed tomography, on-table fluoroscopy and at final follow-up.
Minimally invasive surgical technique
Since 2012 surgeons in our institution has preferentially used MIS as a preferred technique for fixation of thoracolumbar and lumbar fractures. Prior to this, all operative cases were performed with open techniques. For the MIS technique, we perform a pre-operative X-ray to assess the ability to visualise the pedicles on plain fluoroscopy. If the pedicles could be visualised then MIS surgery was considered to be feasible as there was no access to advanced intra-operative navigation or 3D imaging reconstructions at that time. In all patients undergoing MIS, the instrumentation set used was VIPER 2 (DePuy Synthes Spine, Raynham, Massachusetts, USA) pedicle screw instrumentation. We positioned patients prone on a standard Jackson Table (MizuhoOsi, Union City, California, USA). Typically, partial correction of deformity can be generated by placing the patient in prone position. Standard percutaneous pedicle screw instrumentation was undertaken, at one level above and below the fracture using biplanar fluoroscopy. This screw insertion technique has been well described (5). Two types of screws were used, monoaxial screws were inserted in the caudal level and polyaxial screws were inserted in the cranial level. Rod contouring was done manually using French benders or table mounted vices. After passage of rods subfascially through the screw heads, we locked the polyaxial screw heads proximally and lever of the screw towers of the monoaxial screws to generate additional lordosis to correct the deformity.
Patients were mobilized immediately post-operatively without an external orthosis and a post-operative CT scan was performed to assess screw position and fracture reduction. Patient would then be discharged when fit although some patients had other injuries that needed concurrent treatment by other subspecialties. All patients were followed up until bony union was achieved radiographically.
These data were then compared with a group of patients who had undergone short segment fixation using open transpedicular Schanz screw system without decompression for similar indications over a similar time period. For the open technique standard pedicle screw and rod instrumentation was utilized (AO USS Schanz Depuy Synthes, West Chester, PA, USA) as described by Sanderson et al. [1999] (6).
Statistical analysis
Continuous measures are summarised as means with standard deviations and medians with interquartile range. Group differences were assessed using the Wilcoxon test. TLICS score was dichotomised as 4 versus 5–7; Gains score was dichotomised as 3–6 versus 7–9. Group differences on binary variables (sex, TLICS and load sharing score) were summarised as counts and percentages and assessed using Pearson’s Chi-square test. All analyses were completed using SAS v9.4 (SAS Institute Inc., Cary, NC, USA).
Results
There were 13 patients included in the MIS group. A total of 38 patients underwent open Schanz screw fixation at our institution between 2010–2017, of those 19 patients underwent additional laminectomy to decompress the neural elements. To keep the two groups comparable, the latter were excluded. Nineteen patients did not have additional decompressive surgery and their data were used as the OS group.
The demographic data of the two groups are summarised in Table 1. There were slightly more males in both groups than females, with a mean age of 42 in the MIS group and 37 in the open group. The mean duration of follow-up was 9.6 and 10.2 months respectively. The mean TLICS Score and McCormack load sharing score (4) were not statistically different when comparing groups. Overall, there were no significant difference in cohorts when comparing demographics and fracture classification (Table 1).

Full table
The perioperative data of the two groups are summarised in Table 2. Mean operative time was 50 minutes shorter in the MIS group but no statistical difference was found (P=0.15). The mean drop in HB was higher in the OS group, although the significance was marginal (P=0.05). Radiation exposure to the patient and surgical team was however significantly higher in the MIS group (P=0.0007). One patient in the MIS group had postoperative ileus which resolved non-operatively and one patient in the open group progressed to non-union and had failure of implants.

Full table
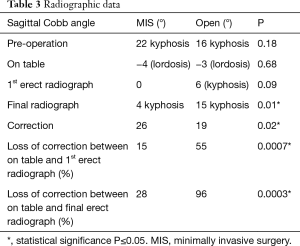
The results of radiographic parameters are shown in Table 3. Pre-operatively, the mean kyphotic angle was 22° in the MIS and 16° in the OS group. Both groups achieved similar on-table correction. On immediate postoperative erect radiographs, the MIS group lost 4° of correction vs. 9° in the OS group, equating to a 15% and 55% loss, respectively (P=0.0007). At final follow-up, both groups had a further loss of position, but significantly higher in the OS group (28% vs. 96%, P=0.0003). The final position achieved for OS group was not different to the preoperative position.
Full table
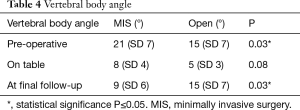
Vertebral body angle was corrected from 21° in the MIS group and 15° in the OS group to 8° and 5° respectively. At final follow-up, there was significant loss of reduction of the vertebral body in the open group vs. MIS group (15 vs. 9, P=0.03) (Table 4).
Full table
Screw accuracy we assess for all MIS patients on postoperative CT and we graded according to classification described by Zdichavsky et al. (7). Only 2 of the 52 screws (4%) inserted we graded as grade 1b (in-out-in). The rest we confined within the pedicles with an overall accuracy of 96%.
Discussion
Treatment of thoracolumbar and lumbar fractures include non-operative measures, posterior instrumented fixation or fusion, anterior column reconstruction or combined anterior-posterior surgery. In neurologically intact patients, the decision to perform surgery is dependent on stability and post-traumatic kyphotic deformity. The TLICS score is commonly used as a guide to predict stability and future deformity to assist in clinical decision making. However, in the absence of level I studies to guide decision making, the choice of MIS versus OS in thoracolumbar and lumbar fractures without neurology comes down to training, surgical philosophy and interpretation of best available evidence.
A previous publication by our institution demonstrated poor outcomes for patients with post-traumatic kyphotic deformity of >20° or more than 50% loss of anterior vertebral body height if treated conservatively (8). Our institution subsequently published our experience with short segment fixation without fusion for these fractures (6) and it has been our practice to treat majority of such fracture utilising this technique. In that publication, the authors reported that while there was an initially high amount of correction of post-traumatic kyphosis, there was a loss of correction of 50% at 2 years follow-up although it should be recognised that none of these fractures were treated with concomitant anterior column reconstruction (6). Another older study has also shown that short-segment pedicle screw instrumentation for unstable thoracolumbar fracture is association with high rate of progressive kyphotic deformity (9). In a more recent publication on thoracolumbar and lumbar fractures using short segment fixation without fusion, Aono et al. [2016] reported that this technique yielded satisfactory reduction and maintenance of fractured vertebra (10). They have attributed their success to modern implant material (titanium), diameter of pedicle screws (>6 mm) and avoidance of posterior surgical decompression (10). While the fractured vertebral body angle (which is a measure of vertebral body reduction) was maintained in the Aono study, their patients actually had a mean loss of correction in bi-segmental Cobb angle of 10° out of the mean 13° achieved, which equates to an 82% loss of reduction over time (10). They acknowledged the loss of position and attributed this finding to loss of disc height adjacent to the injured vertebra (10). Our OS cohort underwent comparable surgical techniques—titanium pedicle screws, without additional decompressive procedure. Sixteen of the 19 patients had all pedicles instrumented with 6 mm in diameter screws. Two patients were instrumented with 5 mm pedicles screws due to small pedicle diameter and one patient had combination of 5 and 6 mm pedicle screw instrumentation. In addition, our OS group had a similar load sharing score of 7 similar to Aono et al. (10). In our study, we have however noted high rate of loss of correction in the OS group, comparable with our institution earlier experience. In fact, more than 50% of correction is loss on 1st erect radiograph and 96% of correction is lost at final follow-up. Our OS group had almost double the correction on table by comparison (19° vs. 10°) (10) which may account for the greater degree of loss of position, and we have noted that the loss of position is mainly due to the collapse of the fractured vertebra. The final vertebral body angle for OS group was not different to the pre-operative position.
Minimally invasive surgery (MIS) using percutaneous instrumentation provides the advantage of less tissue dissection and minimises approach related complication (3) but there is limited data on its performance compared to open techniques in thoracolumbar and lumbar fractures. Extrapolating from degenerative fusion studies it is likely that less soft tissue trauma is associated with less blood loss and infection in spinal trauma with use of MIS compared to OS (11,12). Zhang et al. published their experience with the use of minimally invasive percutaneous pedicle screw for thoracolumbar and lumbar fractures and reported satisfactory fracture reduction and maintenance of reduction (3). In their study, their mean preoperative pre-operative kyphotic deformity of 11° and they were able to achieve complete anatomical correction of 11° with a minimal loss of correction at 12 months of only 3° (3). Our MIS patient cohort had a pre-operative kyphotic deformity more than double the aforementioned study. Most standard percutaneous pedicle screw systems have a polyaxial head to allow easier linkup to the rod, however the reduced angular stability of polyaxial screws equate to a lesser potential to correct for higher degrees of posttraumatic kyphotic deformity. The use of combined percutaneous monoaxial and polyaxial screws confer rigidity required to correct for such deformity as well as rod link up. We used the monoaxial screws in the caudal larger vertebra to allow a larger diameter pedicle screws to be inserted and a stable base to levered on after locking off the rod on the cranial polyaxial screws. A combination of 6 and 5 mm screws were used depending on pedicle size. Our study showed that we were able to achieve a mean of 26° correction, which was superior to the OS group. In addition, despite being only a short construct (single level cranial and caudal to the fracture), fracture reduction was satisfactory over time. Despite losing 28% of correction at final follow-up, the mean final position was 4° kyphosis which can be satisfactorily tolerated in most patients. We believe the superior maintenance of reduction seen in the MIS group is because of preservation of the residual capsular ligamentous structure and facet capsule that provides additional stability to the construct. Open approach for transpedicular screw insertion disrupts the thoracolumbar fascia, paraspinal muscles and risk disruption to facets’ capsular integrity. For our MIS technique, we utilise a slight lateral entry point as an effort to avoid injury to the facet capsule, which can sometimes be the only intact structure for such injury.
Our practice of treating neurological intact patients with thoracolumbar and lumbar fractures using standalone short segment fixation is in line with findings from recent systematic review showing high level of evidence for using this technique in the operative treatment for such fractures (13). Posterior standalone technique had similar outcome to anterior standalone reconstruction or combined anterior-posterior reconstruction (13). In addition, the posterior approaches were associated with lower complications as opposed to the anterior or combined approaches (13). We acknowledge the potential loss of reduction without anterior column support in highly comminuted vertebral body fractures, however our study has shown that the MIS group had a mean of 4° kyphotic deformity at final follow which can be well tolerated in most patients, not justifying the additional risk for anterior column reconstruction. We reserve additional anterior reconstruction in patients with neurological deficit due to anterior retropulsed bone fragments, whom we cannot achieve satisfactory decompression and reduction of fragment through ligamentotaxis through the posterior approach.
The main limitation of our study is that our study is a retrospective study and it was up to the surgeons’ preference to utilise either implants. One can argue that Schanz screw construct might have been used for treatment of more complex fracture, however as shown in Table 1, both groups have comparable preoperative fracture characteristics (predominant AO type A3 fractures and mean TLICS 5). Another limitation is that only 40% of patients in both the MIS and OS group had their implants removed. Whilst in the past we routinely plan for removal at 12 months post-surgery, we now offer patients the choice of this additional surgical procedure. While it is not a difficult procedure, it is not benign and the majority of patients in both groups elected not to have this additional procedure done. This is in line with our institution’s earlier publication that the lack of problems associated with implant retention suggests that routine removal of these internal fixation devices may not be necessary (6). For those that had their implants removed, further radiological analysis of did not reveal any further collapse from their final position radiographs when compared to radiographs with implants in situ at 9 months. Other limitations include definitive confirmation of fusion with CT scanning and lack of assessment of the erect global sagittal alignment in each group.
In conclusion, combined polyaxial-monoaxial screw MIS constructs demonstrate favorable radiological and clinical outcomes for treatment of unstable thoracolumbar and lumbar fractures for patients who do not require additional decompressive surgery. Our study also demonstrates higher rates of radiological collapse in the OS cohort.
Acknowledgements
We thank Dr. Stuart Howell, Data, Design and Statistics Service, Adelaide Health Technology Assessment, School of Public Health, University of Adelaide, for his assistance in statistical analysis.
Funding: The Royal Adelaide Hospital Spinal Unit receives annual Fellowship Funding from Johnson & Johnson Ltd. ($50,000 PA) and LifeHealthCare Ltd. ($80,000 PA).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethics approval was not required for this study. Consent was obtained from all patients for their radiological and clinical data to be collected for research purposes.
References
- Rajasekaran S, Kanna RM, Shetty AP. Management of thoracolumbar spine trauma: An overview. Indian J Orthop 2015;49:72-82. [Crossref] [PubMed]
- Vanek P, Bradac O, Konopkova R, et al. Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine 2014;20:150-6. [Crossref] [PubMed]
- Zhang W, Li H, Zhou Y, et al. Minimally Invasive Posterior Decompression Combined With Percutaneous Pedicle Screw Fixation for the Treatment of Thoracolumbar Fractures With Neurological Deficits: A Prospective Randomized Study Versus Traditional Open Posterior Surgery. Spine (Phila Pa 1976) 2016;41 Suppl 19:B23-9. [Crossref] [PubMed]
- McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976) 1994;19:1741-4. [Crossref] [PubMed]
- Mobbs RJ, Sivabalan P, Li J. Technique, challenges and indications for percutaneous pedicle screw fixation. J Clin Neurosci 2011;18:741-9. [Crossref] [PubMed]
- Sanderson PL, Fraser RD, Hall DJ, et al. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J 1999;8:495-500. [Crossref] [PubMed]
- Zdichavsky M, Blauth M, Knop C, et al. Accuracy of Pedicle Screw Placement in Thoracic Spine Fractures. Eur J Trauma 2004;30:234-40. [Crossref]
- Osti OL, Fraser RD, Cornish BL. Fractures and fractures-dislocations of the lumbar spine. A retrospective study of 70 patients. Int Orthop 1987;11:323-9. [Crossref] [PubMed]
- McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 1993;75:162-7. [Crossref] [PubMed]
- Aono H, Tobimatsu H, Ariga K, et al. Surgical outcomes of temporary short-segment instrumentation without augmentation for thoracolumbar burst fractures. Injury 2016;47:1337-44. [Crossref] [PubMed]
- McGirt MJ, Parker SL, Lerner J, et al. Comparative analysis of perioperative surgical site infection after minimally invasive versus open posterior/transforaminal lumbar interbody fusion: analysis of hospital billing and discharge data from 5170 patients. J Neurosurg Spine 2011;14:771-8. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Sansur CA, et al. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2011;36:556-63. [Crossref] [PubMed]
- Scheer JK, Bakhsheshian J, Fakurnejad S, et al. Evidence-Based Medicine of Traumatic Thoracolumbar Burst Fractures: A Systematic Review of Operative Management across 20 Years. Global Spine J 2015;5:73-82. [Crossref] [PubMed]


