Instrumentation complication rates following spine surgery: a report from the Scoliosis Research Society (SRS) morbidity and mortality database
Introduction
Instrumentation related complications (IRC) are among the most common complications that occur in spine surgery. Over the past two decades, the reported incidence has ranged from 0.6–3% in the adolescent idiopathic scoliosis (AIS) population and up to 40.2% in adult spinal deformity patients that undergo three-column osteotomies for major deformity correction (1-3). IRC range from malpositioning, with resultant neurological or infectious sequelae, to catastrophic construct failure. Unfortunately, many of the studies reporting on IRC in spine surgery are limited by a single surgeon, single institution, or a relatively small patient population (4-7).
The Scoliosis Research Society (SRS) was founded in 1966 as an international society committed to research and education in the field of spinal deformities. The SRS morbidity and mortality (M&M) database is not funded, and relies completely on volitional, prospectively gathered information from SRS surgeons (8). Surgical databases, like the SRS database, have tremendous value in spine surgery. The SRS has gathered surgeon-reported complications, including instrumentation failure, visual complications, new neurological deficits, infections, and death. The true power of the SRS database is gained through its large and diverse sample size: extensive data collection, vast number of cases, broad spectrum of pathology, extensive numbers of surgeons and numerous institutions. Additionally, Webb and colleagues have substantiated the generalizability of the SRS database and the validity of surgeon-reported data (9). As a result, there have been numerous publications reporting on the data within this database (1,10-13).
Overall, there remains limited literature on the incidence and risk factors that predispose patients to IRC. Analysis of large, validated databases are necessary to develop generalizable conclusions and to help inform patients on the risk of such complications, especially with the increasing number of spinal fusion procedures performed each year. The objective of the current study was to analyze instrumentation complications within the SRS M&M database to determine the incidence, patient characteristics, and perioperative factors associated with this complication.
Methods
By requirement of the SRS, all members must annually submit data on spine surgeries performed, as well as those associated with M&M. Through a secure Internet-based system, de-identified data is recorded and submitted by the surgeon. Data collected includes the total number of surgeries performed across several diagnoses, as well as specific information on patients with instrumentation complications, acute infection, vision loss, neurologic deficits, and death.
The database was queried for all patients experiencing IRC from 2009–2012. Patient demographics, comorbidities, preoperative diagnoses, curve magnitudes, perioperative factors, and intraoperative characteristics were analyzed. Intraoperative characteristics included surgical approach, performance of fusion, performance of osteotomy, operative times, operative blood loss, type of instrumentation used, and documented IRC. The type of instrumentation complication was further classified into three categories: implant failure, implant migration, or malpositioned implant. Potential associated complications were also assessed, including new perioperative neurologic deficit, intraoperative implant removal secondary to the development of a neurologic deficit, postoperative infection, and mortality.
Unadjusted univariate analysis was performed to determine mean differences between categorical variables utilizing either Chi-squared or Fisher’s exact testing. A P value of <0.05 was considered statistically significant. Data was analyzed using SPSS Statistics v24.0 (IBM Corp., Armonk, NY, USA).
Results
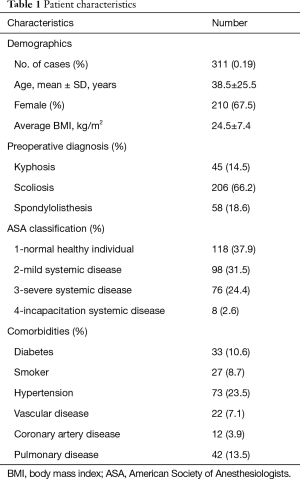
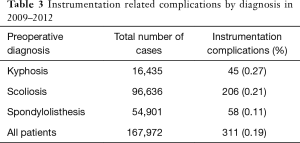
A total of 167,972 patients were identified, including 96,636 patients with a diagnosis of scoliosis, 54,901 with spondylolisthesis, and 16,435 with kyphosis. Instrumentation-related complications occurred in 311 patients with an overall rate of 0.19%, or 18.5 per 10,000 patients (Table 1). There were 206 patients with scoliosis (66.2%), 58 patients with spondylolisthesis (18.6%), and 45 patients with kyphosis (14.5%) that experienced instrumentation complications. The mean age of patients was 38.5±25.5 years with a female predominance (67.5%) and mean BMI of 24.5±7.4. There were 73 patients with hypertension (23.5%), 42 with pulmonary disease (13.5%), 33 with diabetes (10.6%), 27 with active smoking history (8.7%), 22 with vascular disease (7.1%), and 12 with coronary artery disease (3.9%). The majority of patients were classified as American Society of Anesthesiologists (ASA) score I or II (Table 1).
Full table
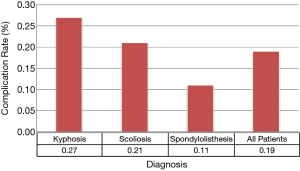
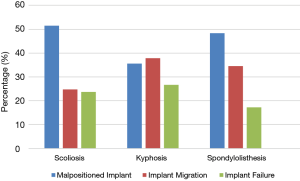
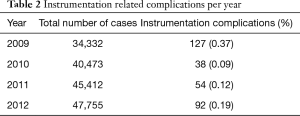
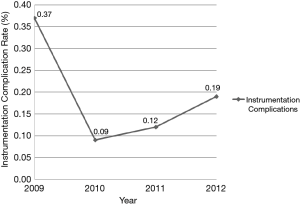
Instrumentation complication rates decreased significantly from 2009 to 2012 (0.37% vs. 0.19%, P<0.001) (Table 2, Figure 1). There was a dramatic decrease from 2009 to 2010, and then a gradual increase from 2010 to 2011 and to 2012. The overall difference between 2009 and 2012 was still a statistically significant decreased. When compared to patients with a diagnosis of spondylolisthesis, patients with kyphosis (0.27% vs. 0.11%, P<0.001) and patients with scoliosis (0.21% vs. 0.11%, P<0.001), experienced significantly more instrumentation complications (Table 3, Figure 2).
Full table
Full table
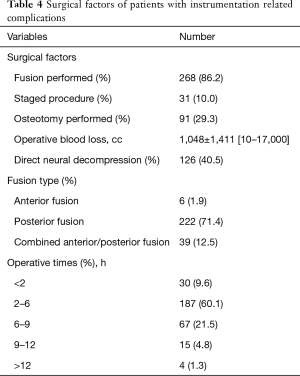
Spinal fusion was performed in 268 patients (86.2%) with 31 (10.0%) of those being staged procedures (Table 4). The majority of patients underwent a posterior only fusion (71.4%). Posterior column osteotomies were performed in 91 patients (29.3%). Other surgical factors including operative times, blood loss, number of patients that underwent decompressions and implants used are listed in Table 4.
Full table
When classified by type of instrumentation complication, malpositioned implants (48.6%) occurred most commonly, followed by implant migration (28.3%), and implant failure (23.3%). The different types of IRC per diagnosis are shown in Figure 3, and there was no significant difference in the rates of each type of complication. Among the complications associated with IRC, development of a new perioperative neurologic deficit occurred most commonly and was reported in 146 patients (46.9%). Eighty-four patients (27%) required implant removal secondary to the development of an intraoperative neurologic deficit. Additionally, postoperative infections occurred in 22 patients (7.1%) that had IRC.
Discussion
The current study found a total of 311 patients with IRC from 2009–2012 with an average rate of 0.19% per year and an incidence of 18.5 per 10,000 deformity cases. The rate has significantly decreased from 2009 to 2012 (0.37% vs. 0.19%, P<0.001) and was significantly lower in patients with a diagnosis of spondylolisthesis compared to those with kyphosis or scoliosis. The potentially avoidable malpositioning of implants represents 48.6% of these complications. A new perioperative neurologic deficit occurred in 46.9% of patients with an instrumentation complication, 57.5% of which occurred intraoperatively and required implant removal.
In 2006, Coe and colleagues analyzed 363 of 6,334 AIS patients from the SRS M&M data from 2001–2003 and found IRC rates of 0.6% for posterior instrumentation and fusion, 1.4% for anterior instrumentation and fusion, and 1.0% for combined anterior and posterior fusion procedures (1). Additionally, in a 5-year prospective series of 99 AIS patients, 3% of patients required revision surgery for malpositioned posterior instrumentation (2). Li et al. analyzed more than 1,000 thoracic 106 screws placed in 208 deformity patients and found an overall complication rate attributed 107 to pedicle screws of 7.2%. They found 1.7% of the screws were malpositioned on CT, occurring most commonly in severe curves >90º and on the concavity of the curves. Three screws required removal for loosening, and there were 3.8% infections and 1 neurological complication related to the malpositioned screws (14). In a more recent study involving 82 adult spinal deformity patients, Smith and colleagues reported an instrumentation complication rate of 40.2% in patients that underwent three-column osteotomies (15). Rod breakage was the most common complication occurring in 31% of cases and resulting in 17% reoperation. In a 2014 prospective multicenter study by Smith et al. (15), rod fracture occurred in 18 cases (9.0%) at a mean of 14.7 months (range, 3–27 months). Our study found an average instrumentation complication rate of 0.19% from 2009–2012 with an overall rate of 0.1% secondary to screw malpositioning. Of the patients with IRC, 27% required implant removal secondary to intraoperative neurologic changes.
There is an increased interest in using navigation or robotic guidance to decrease the rates of IRC. Our study shows an overall very low IRC rate. One strategy to improve these already low rates of IRC includes paying close attention to the bony anatomy, particularly in fellowship training institutions. Additionally, the use of navigation and robotics has been shown to improve pedicle screw accuracy in many instances, and could be considered in more difficult or complex spinal deformity surgeries (16,17).
The limitations of the current study are primarily inherent to analyses of large patient databases with unclear accuracy and completeness of submitted data. No quality assurance measures are utilized to verify the voluntarily submitted data. Similar to other databases, the SRS M&M database is subject to recall bias as members may input all data once a year before the deadline, which may skew the data toward complications occurring within proximity to the deadline. Moreover, complications may be underreported by members as higher complication rates are found in other retrospective studies (1,18). Alternatively, the lower incidence of complications in the SRS M&M database may be indicative of a change in both operative technique and an increased emphasis on medical perioperative management. Prior efforts aimed at validating the SRS database ultimately concluded that differences would remain across several databases secondary to the methods of data collection. Despite this limitation, conclusions drawn from the SRS database have previously shown good concordance with other large databases with respect to complication data (9). The size of this patient cohort allows this data to be generalizable as it represents complication data from modern, fellowship-trained surgeons operating within the most up-to-date standard of care. Long term follow-up of IRC and their impact on hospital costs and health-related quality of life are necessary to continually improve treatment of patients undergoing spinal deformity surgery.
Conclusions
The current analysis of 167,972 spinal deformity cases within the SRS M&M database showed an average rate of 0.19% per year and an incidence of 18.5 per 10,000 deformity patients. The highest risk of IRC occurred in patients with a preoperative diagnosis of kyphosis. Nearly 50% of IRC were due to the potentially avoidable malpositioning implants. Closer attention to posterior bony anatomy, improved intraoperative imaging, and utilization of navigation or robotic guidance may potentially decrease these instrumentation complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was not applicable as the data was from a de-identified SRS database.
References
- Coe JD, Arlet V, Donaldson W, et al. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2006;31:345-9. [Crossref] [PubMed]
- Hwang SW, Samdani AF, Marks M, et al. Five-year clinical and radiographic outcomes using pedicle screw only constructs in the treatment of adolescent idiopathic scoliosis. Eur Spine J 2013;22:1292-9. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Klineberg E, et al. Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 2017;27:444-57. [Crossref] [PubMed]
- Gum JL, Lenke LG, Bumpass D, et al. Does Planned Staging for Posterior-Only Vertebral Column Resections in Spinal Deformity Surgery Increase Perioperative Complications? Spine Deform 2016;4:131-7. [Crossref] [PubMed]
- Papadopoulos EC, Boachie-Adjei O, Hess WF, et al. Early outcomes and complications of posterior vertebral column resection. Spine J 2015;15:983-91. [Crossref] [PubMed]
- Ayvaz M, Olgun ZD, Demirkiran HG, et al. Posterior all-pedicle screw instrumentation combined with multiple chevron and concave rib osteotomies in the treatment of adolescent congenital kyphoscoliosis. Spine J 2014;14:11-9. [Crossref] [PubMed]
- Ghayem Hassankhani E, Omidi-Kashani F, Moradkhani S, et al. Comparison of Clinical and Radiologic Outcome of Adolescent Idiopathic Scoliosis Treated with Hybrid Hook-Screw Instrumentation versus Universal Clamp System. Adv Med 2016;2016:7639727. [Crossref] [PubMed]
- Shaffrey E, Smith JS, Lenke LG, et al. Defining rates and causes of mortality associated with spine surgery: comparison of 2 data collection approaches through the Scoliosis Research Society. Spine (Phila Pa 1976) 2014;39:579-86. [Crossref] [PubMed]
- Webb ML, Lukasiewicz AM, Samuel AM, et al. Overall Similar Infection Rates Reported in the Physician-reported Scoliosis Research Society Database and the Chart-abstracted American College of Surgeons National Surgical Quality Improvement Program Database. Spine (Phila Pa 1976) 2015;40:1431-5. [Crossref] [PubMed]
- Hamilton DK, Smith JS, Sansur CA, et al. Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: a report of the scoliosis research society morbidity and mortality committee. Spine (Phila Pa 1976) 2011;36:1218-28. [Crossref] [PubMed]
- Sansur CA, Smith JS, Coe JD, et al. Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine (Phila Pa 1976) 2011;36:E593-7. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Sansur CA, et al. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2011;36:556-63. [Crossref] [PubMed]
- MacEwen GD, Bunnell WP, Sriram K. Acute neurological complications in the treatment of scoliosis. A report of the Scoliosis Research Society. J Bone Joint Surg Am 1975;57:404-8. [Crossref] [PubMed]
- Li G, Lv G, Passias P, et al. Complications associated with thoracic pedicle screws in spinal deformity. Eur Spine J 2010;19:1576-84. [Crossref] [PubMed]
- Smith JS, Shaffrey E, Klineberg E, et al. Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine 2014;21:994-1003. [Crossref] [PubMed]
- Overley SC, Cho SK, Mehta AI, et al. Navigation and Robotics in Spinal Surgery: Where Are We Now?. Neurosurgery 2017;80:S86-99. [Crossref] [PubMed]
- Staartjes VE, Klukowska AM, Schröder ML. Pedicle Screw Revision in Robot-Guided, Navigated, and Freehand Thoracolumbar Instrumentation: A Systematic Review and Meta-Analysis. World Neurosurg 2018;116:433-43.e8. [Crossref] [PubMed]
- Sharma S, Wu C, Andersen T, et al. Prevalence of complications in neuromuscular scoliosis surgery: a literature meta-analysis from the past 15 years. Eur Spine J 2013;22:1230-49. [Crossref] [PubMed]