Anterior atlantoaxial subluxation with Down syndrome and arthritis: case report
Introduction
Down syndrome (DS) occurs when an individual has a full or partial extra copy of chromosome 21 and is the most common of all malformation syndromes. On average 1 in every 700 to 900 births will present this syndrome, and it can change by various factors such as the age of conception, reaching a proportion <1:1,000 among pregnant women older than 40 years (1,2). In Colombia according to the study carried out by Julio et al. the prevalence of live births with DS during the period 1998 to 2005 was 1.7 per thousand (3). The clinical presentation mostly shows: characteristic facial features, hypotonia, mental retardation, and several malformations involving the circulatory and digestive systems (4).
Juvenile chronic arthritis (JCA) is a systemic disease of childhood affecting joints mainly. JCA is a heterogeneous group of inflammatory joint disorders with onset before the age of 16 years, comprising of seven subtype groups. The pathogenesis of JCA seen in the cervical spine is synovial inflammation, hyperemia, and pannus formation at the occipitoatlantoaxial joints resulting in characteristic craniovertebral junction (CVJ) findings (5).
Anterior atlantoaxial subluxation (AAAS) has a metric defined as an increase at the anterior atlantodental interval (AADI). The increase is representing the space between the anterior aspect of the dens and the posterior aspect of the anterior ring of the atlas. It usually is less than 5 mm on lateral cervical RX for kids under 15 years old, everything more than that is consider an instability at the CVJ (5).
Studies are reporting that for the 8% to 63% of craniocervical instability (CCI) patients, they also have a DS diagnosis. AAAS occurs in 10% to 30% of patients with DS but only 1–2% shows symptoms (6,7). The stability of CVJ primarily depends on the integrity between the ligaments and bones and can be altered by masses, trauma or iatrogenic complications like transoral odontoidectomy. It is necessary to identify relevant anatomical structures such as the opisthion, basion, tuberculum sella, posterior margin of the hard palate and the odontoid process to determine the preservation of this relationship. From them, it will measure Mcgregor’s line, Chamberlain’s line, Wackenheim’s clivus baseline, then clivus-canal angle, and the basal angle, as well as the anterior atlanto-dental space among others (8).
Case presentation
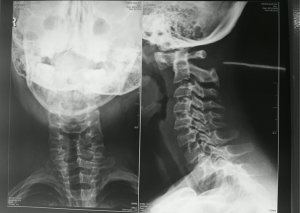
We present the case of a male patient of 10 years old with DS and juvenile arthritis who during the last two years has presented cervical pain with left predominance, managed with oral anti-inflammatory and local heat. Five days before admission to the emergency department, the patient rested in bed, and after 6 hours of rest without any management, was able to improve. That’s why during regular medical control, physician doctor requested to perform an X-ray on the lateral cervical spine channel (Figure 1). At admission to the Emergency Department of the Colombian Oftalmologica Foundation (FOSCAL) (Floridablanca-Colombia), a complete neurological examination was performed: tone, tropism and symmetric mobility of the extremities, with symmetrical paresis of arms distal to proximal (4/5) as the only positive finding.
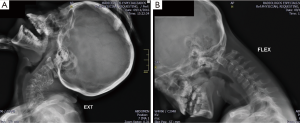
The medical team treating decide to apply dynamic cervical X-rays finding increase in the atlantoaxial space of approximately 7 mm associated with subluxation which decreases in extension and increases in flexion (Figure 2), high-resolution CT scanning cervical shows AADI of 11 mm (Figure 3), and MRI scan that evidence odontoids displaced rear and top with space preodontoide with basilar impression (Figure 3).
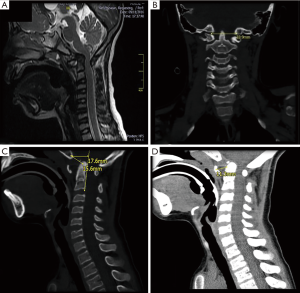
According to the three studies, this is a patient with AAAS with an approximately 11 mm, basilar impression and platybasia with severe medullary compression in 2 points, the first in the bulb by odontoides directly and the second in foramen magnum by cervical stenosis.
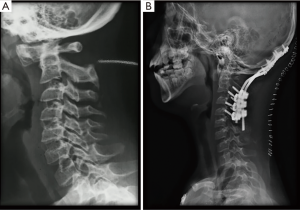
Additionally, draws typical attention to findings of juvenile arthritis on the tip of the odontoid process that was not evidenced in previous MRI scan 2 years ago (Figure 4). It is therefore highly relevant that the neurosurgery and pediatrics rheumatology departments decide that the patient will be taken to a surgical procedure for the upper cervical fusion by posterior instrumentation taking into account the findings in different images concerning the patient’s symptoms and pathological history.

The surgery was performed without complications, releasing the medullary compression at the height of foramen magnum and stabilizing the CVJ by posterior approach (Figure 5). The patient is currently without a neurological deficit, mobilizes the 4 limbs with preserved strength and without pain.
Discussion
The CVJ is a complex articulate point composed for the occiput, atlas, and axis (OC-C1-C2) and various ligaments that represents the transition between the skull base and spine. The CVJ is also the respective transition of the brainstem to the cervical spinal cord and this is the most flexible point of the entire column especially in kids under 15 years old. The basic movements in this joint are capital flexion/extension OC-C1, axial rotation, flexoextension C1-C2. All these movements can always coincide with the axial rotation ventral to the foramen magnum (9).
As stated by the Consensus Statement of the Spine Trauma Study Group the basion-dental interval (BDI) and the basion-posterior axial line interval (BAI) rules of 12 technique (a measurement greater than 12 mm is pathologic) are the most exact, sensitive, and easy to manage for detecting and classifing occipitocervical dissociation and dislocations in DS (10) (Figure 5C).
On the other hand, it is considered that when the of the tip of odontoid process project more than 5 mm to the Chamberlain’s line or 7 mm to McGregor’s this is basilar impression that refers to an abnormality that shows the vertebral column situated in an abnormally high position due to decreased height of the skull base (11,12).
Atlantoaxial instability (AAI) and less commonly occipitoatlantal instability (OAI) can be found in 70% of patients with DS (4,13,14) and can be associated to bone deformities own of this pathology, 6% of these persons who have DS also have os odontoideum. Other proposed causes for AAI in DS are: intrinsic collagen decreases causing looseness at the transverse ligament, affecting the stability of the dens with the anterior arch of C1 (6,15). For this reason, these patients should carry a radiographic control of the cervical spine from 3 years old. After that, any alteration that is evident make changes in the lifestyle that includes limitation for sports, and always keep in mind that it is quite rare that patients debut, with neurological symptomatology, associating with a spinal cord compression (15). Especially those who attend with another kind of pathologies associated with trisomy 21 as is the case that we present on this occasion.
As an uncommon pathology, experience in the surgical management is not very extended, Mummaneni et al. first proposed the use of C1–C2 transarticular screws in adults, and an alternative technique, namely C1 lateral mass screws and C2 pedicle screws (16). Since the cervical using the fusion technique or the management of this pathology is common, recent studies have proved disappointing results where up to 40% of treated patients showed serious complications especially in children (17).
Taking into account JCA, the goals for surgery may be as earliest as possible, looking for prevention of any neurological deterioration by spinal cord compression. If the patient does not shows any symptom, the indication for surgical decompression with fusion are: <14 mm space visible for the cord or cervical instability >8 mm. Patients with 5–8 mm of cervical instability plus clinical symptoms of spinal cord impingement, and those who preset neurological disrepair should undergo surgery (5).
Today, the majority of patients that request surgeries undergo posterior instrumentation and fusion. Requiring transoral decompression in cases involving fundamental irreducible ventral compression (17,18). However, the surgeon who is going to deal with these cases should be profoundly acquainted with the anatomic variations in the vasculature and bone structure of the patients with DS. The surgeons must also have the full set of images before the start of the procedure which includes 3 Rx’s lateral cervical spine X-rays, with flexion and extension views, an MRI scan is completed to measure the with of the spinal subarachnoid space and is the most effective modality for spinal cord injury and, high-resolution CT scann at C3-C4 join is mandatory for all cases of occipitocervical fusion (6).
According to the review carried out by Hankinson et al. in 2010 and his personal experience, the study had concluded that it is an essential add of the preoperative planning stereotactic navigation system to plan all screw trajectories and sizes. According to these authors the upper cervical fusion whit transarticular screw placement OC-C2 and supplementing using autograft, either from the rib or iliac crest, should be based on the age and size of the patient it is the best option (6).
Conclusions
Pediatric patients with DS represent a challenge for the spine neurosurgeons particularly by collagen defects and hypermobility. As it is the case that we present in this opportunity, the association with autoimmune diseases such as juvenile arthritis, due to the pannus located at the odontoides process, which gives a greater predisposition to articular alterations, as well as showing an increase of the perilesional edema especially during the postoperative period.
On the other hand, it is essential to keep in mind the complications associated with the surgical procedure CVJ level specially on patients with DS and that has been described since 1981 by Nordt and Stauffer et al. and this group showed two patients with DS who underwent C1-C2 fusions plus posterior wiring. Both of these cases resulted in quadriplegia after the procedure (18). Which was highly disappointing, nowadays complication rates occurred in 73% to 100% of all patients with DS and cervical spine surgery, some of them were from: local infection, wound dehiscence, incomplete joint reduction, loss of reduction (LOR), nonunion, adjacent segment instability, graft resorption, neurologic sequelae, a variety of respiratory complications, and death (19).
According to the study of Siemionow et al. a retrospective follow up of the cases with DS who had undergone cervical spine surgery between 1998–2011 (apx 24 months), they conclude that rates of perioperative complications have not significantly changed in the last 3 decades. Additionally, the study had mentioned that an anterior approach might result in a higher risk of complications than posterior cervical procedures in patients with DS (20). However this study did not include pediatric patients or with a history of arthritis which adds the presence of pannus in the odontoid process as a complication for surgery and must be a determining factor for defining the surgical approach.
We think that this case is highly relevant for medical literature, taking into account that we must considered many variables to determine the best option regarding the definitive management for patient and we would like to present the main problems that we are facing with the handling of this case.
- It’s a highly dangerous pathology in a patient with DS of 10 years old who was able to submit with minor trauma while he was in their daily activities with severe neurologic injury or even death, requires radical and definitive management.
- The association of CVJ instability with JCA that gives greater complexity in the time to define the surgical approach.
- The personal conflict that generates in the patient and his family doing a posterior fixation with fusion in a little boy.
- According to our experience, we recommend to all medical professionals that CT scan must follow any suggestive finding of odontoid pannus at least every 6 months to identify early lesions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Mentis AF. Epigenomic engineering for Down syndrome. Neurosci Biobehav Rev 2016;71:323-7. [Crossref] [PubMed]
- Sherman SL, Allen EG, Bean LH, et al. Epidemiology of Down syndrome. Ment Retard Dev Disabil Res Rev 2007;13:221-7. [Crossref] [PubMed]
- Julio NH, Lucía CO. Estudio epidemiológico global del síndrome de Down. Rev Chil Pediatr 2011;82:105-12. [Crossref]
- El-Khouri M, Mourão MA, Tobo A, et al. Prevalence of atlanto-occipital and atlantoaxial instability in adults with Down syndrome. World Neurosurg 2014;82:215-8. [Crossref] [PubMed]
- Wolfs JF, Arts MP, Peul WC. Juvenile chronic arthritis and the craniovertebral junction in the paediatric patient: review of the literature and management considerations. Adv Tech Stand Neurosurg 2014;41:143-56. [Crossref] [PubMed]
- Hankinson TC, Anderson RC. Craniovertebral junction abnormalities in Downsyndrome. Neurosurgery 2010;66:32-8. [Crossref] [PubMed]
- Herring JA. Cervical instability in Down's syndrome and juvenile rheumatoid arthritis. J Pediatr Orthop 1982;2:205-7. [Crossref] [PubMed]
- Smoker WR, Khanna G. Imaging the craniocervical junction. Childs Nerv Syst 2008;24:1123-45. [Crossref] [PubMed]
- Steinmetz MP, Mroz TE, Benzel EC. Craniovertebral junction: biomechanical considerations. Neurosurgery 2010;66:7-12. [Crossref] [PubMed]
- Bono CM, Vaccaro AR, Fehlings M, et al. Measurement techniques for upper cervical spine injuries: consensus statement of the Spine Trauma Study Group. Spine (Phila Pa 1976) 2007;32:593-600. [Crossref] [PubMed]
- Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg 1998;88:962-8. [Crossref] [PubMed]
- Dolan KD. Cervicobasilar relationships. Radiol Clin North Am 1977;15:155-66. [PubMed]
- Ali FE, Al-Bustan MA, Al-Busairi WA, et al. Cervical spine abnormalities associated with Down syndrome. Int Orthop 2006;30:284-9. [Crossref] [PubMed]
- Pizzutillo PD, Herman MJ. Cervical spine issues in Down syndrome. J Pediatr Orthop 2005;25:253-9. [Crossref] [PubMed]
- Wadhwa R, Mummaneni PV. High cervical instability in adult patients with Down syndrome. World Neurosurg 2015;83:332-3. [Crossref] [PubMed]
- Mummaneni PV, Haid RW. Atlantoaxial fixation: overview of all techniques. Neurol India 2005;53:408-15. [Crossref] [PubMed]
- Tauchi R, Imagama S, Ito Z, et al. Complications and outcomes of posterior fusion in children with atlantoaxial instability. Eur Spine J 2012;21:1346-52. [Crossref] [PubMed]
- Browd S, Healy LJ, Dobie G, et al. Morphometric and qualitative analysis of congenital occipitocervical instability in children: implications for patients with Down syndrome. J Neurosurg 2006;105:50-4. [PubMed]
- Smith MD, Phillips WA, Hensinger RN. Fusion of the upper cervical spine in children and adolescents. An analysis of 17 patients. Spine 1991;16:695-701. [Crossref] [PubMed]
- Siemionow K, Hansdorfer M, Janusz P, et al. Complications in Adult Patients with Down Syndrome Undergoing Cervical Spine Surgery Using Current Instrumentation Techniques and rhBMP-2: A Long-Term Follow-Up. J Neurol Surg A Cent Eur Neurosurg 2017;78:113-23. [Crossref] [PubMed]
(English Language Editor: Jeremy Dean Chapnick, AME Publishing Company)