Clinical and radiological outcomes of image guided posterior C1-C2 fixation for atlantoaxial osteoarthritis (AAOA)
Introduction
Radiological osteoarthritic degeneration (OA) of the subaxial cervical spine is ubiquitous as patients age. It is usually asymptomatic, and rarely requires intervention. Symptomatic osteoarthritis of the atlantoaxial (C1-C2) facet joint (AAOA) is rare, affecting only 4% of patients with generalised OA (1). The unique anatomy of the atlantoaxial articulation, i.e., lacking an intervertebral disc, leads to a distinct clinical syndrome resulting from the joint degeneration—unilateral suboccipital pain on the pathological side exacerbated by lateral rotation (2) (Figure 1). It leads to reduced range of movement. It can be associated with suboccipital neuralgia due to local muscle spasm irritating the suboccipital nerve. While conservative treatment should always be attempted, intractable pain often culminates in surgical intervention to fuse the C1-C2 articulation. The first report of C1-C2 fusion was in 1939 using posterior wiring (3).
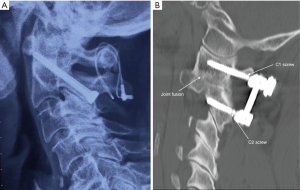
In 1987 posterior transarticular screw (TAS) fixation was reported (4) (Figure 2A) (2,5-9). Pedicle screw fixation was reported by Harms and Melcher in 2001 (10). This obviated the need for posterior cable fixation and the more direct screw insertion allowed for a less invasive surgical exposure (Figure 2B).
The objective of the surgery is stabilisation of the atlantoaxial (C1-C2) articulation to abolish the pain associated with movement of the degenerative facet joint. In our study, fusion was assessed radiographically using X-ray and CT. All patients were interviewed assessing pain using Visual Analogue Scale (VAS), need for ongoing analgesia, range of movement. Function was assessed by the Neck Disability Index (NDI). The purpose of the study was to assess the clinical and radiographic outcomes of surgical treatment for AAOA of a single surgeon (T Steel). This is the first Australian study to report the results of surgical fusion for AAOA. There has only been one previous study reporting on hybrid fixation techniques (11).
Methods
Ethics approval was obtained from St Vincent’s Hospital Human Research Ethics Committee. (SVH file number: 16/054). All patients undergoing posterior atlantoaxial surgery from 2005 to 2015 at our institution by the senior author (T Steel) of this paper were identified through hospital database and private practice records. Inclusion criteria were adult patients undergoing posterior atlantoaxial fixation surgery for AAOA. Patients who had undergone atlantoaxial fixation for other indications were excluded. Patient gender, current age, age at operation, length of hospital stay and follow-up since surgery were recorded. The presenting symptom was unilateral pain in the suboccipital region exacerbated by lateral rotation. Diagnosis was confirmed radiographically in all cases with bone window CT. Pre-operative and post-operative assessments were made. The primary outcome measure was pain assessed by VAS, patient satisfaction outcome questionnaire including the NDI score (12). Patients were asked if they would have the surgery again with the benefit of hindsight. Range of movement in flexion, extension and lateral rotation was recorded for each patient. Secondary outcome measures were the presence of fusion and periprosthetic complications assessed on CT. Joint fusion was assessed by the obliteration of the joint space with evidence of mature bone fusion across the C1-C2 joint.
Data analysis was carried out using SPSS Statistics version 23 (SPSS Inc., Chicago Ill USA). Data is presented as a mean ± standard deviation. One Sample Kolmogorov-Smirnov test was carried out to assess normality of data set, and Wilcoxson Signed-Rank test was performed to ascertain significance in measures in the pre-operative and follow-up setting. Non-parametric tests were used due to the sample size. Fisher’s exact test was used to determine the independence of the outcome variables. Statistical significance was accepted at the P<0.05 level.
Results
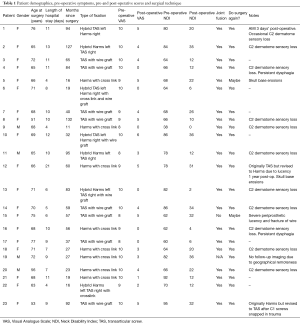
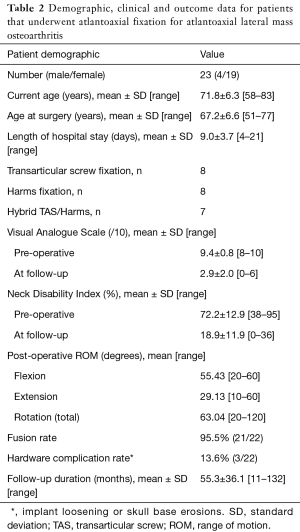
Twenty-three patients with AAOA were enrolled in the study, 19 females and 4 males (Table 1). Mean age at surgery was 67.2 years (range, 51–77 years). Mean follow-up time was 55.3 months (range, 11–132 months) (Table 2).
Full table
Full table
All patients reported severe progressive pain located to the ipsilateral suboccipital region exacerbated by lateral rotation to the affected side. Initially patients described intermittent pain brought on by rotational movement but as the disease progressed patients describe constant pain, exacerbated by any movement. Most patient at the time of the presentation to the senior surgeon (T Steel) had modified their activities to avoid any neck rotation. Flexion and extension were relatively preserved. Lateral rotation to the affected side was reduced to 30 degrees, to the unaffected side to 45 degrees. Fifteen patients reported headaches, mostly in a post-auricular (suboccipital neuralgia) distribution. Two patients reported headaches that radiated to the orbit on the pathological side. Many patients reported continual pain even without movement. Six patients reported pain radiating down to the shoulder. None had radicular pain or symptoms or signs suggestive of myelopathy. All patients had been treated with rest, immobilisation, non-steroidal anti-inflammatory drugs (NSAIDs), narcotic analgesia and facet joint injections. One patient had been on high dose morphine (>90 mg morphine equivalents a day) for 4 years prior to the surgery. Two others were on fentanyl and pethidine patches daily.
Fourteen patients reported their pre-operative range of movement as “non-existent due to the pain”. The other nine patients reported movement as “severely painful”. All patients had previously diagnosed systemic symptomatic OA, mostly in the hands, lumbar spine and subaxial cervical spine.
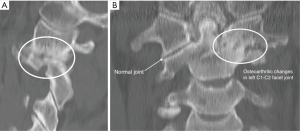
In all cases diagnosis was confirmed with pre-operative CT. Unilateral C1-C2 osteoarthritis was seen with severe joint space narrowing with osteophyte formation and subchondral sclerosis on the side of pain (Figure 1). Microcyst formation typical of severe OA was often seen.
Eight patients underwent TAS fixation with posterior wiring and bone graft. Eight patients had lateral mass pedicle screw fixation according to Harms’ method. Seven patients had hybrid fixations with one side TAS fixation and the other side a pedicle screw fixation due to anatomical variation. Choice of fixation technique was determined at the time of surgery by the senior surgeon (T Steel) on the basis of image guidance (BrainLab AG Feldkirchen, Germany). One patient’s TAS fixation was revised to a Harms fixation due to lack of fusion 14 months following initial surgery. One patient with a Harms fixation was revised to a TAS fixation due to trauma causing fracture of both C1 screws 3 years post initial surgery.
Eleven patients reported sensory disturbance in the C2 dermatome following surgery. It was the senior author’s practice early in this series to section one of the C2 nerve roots to facilitate direct exposure of the atlantoaxial joint to allow bone graft packing into the joint. The persisting sensory disturbance were discomforting to the patients, and as a result, this practice was abandoned. Two patients reported initial dysphagia following the surgery. The first case was minor however the second case was significant enough to cause tablet aspiration on two occasions. One patient, a 76-year-old female, had an acute myocardial infarct 3 days post-surgery with no significant sequelae. There were no other complications.
Primary outcome measures were identified. Data for clinical (VAS, NDI, range of movement) and radiological outcomes were found to be not normally distributed. VAS pain scores were significantly reduced immediately following surgery (Figure 3). The mean pre-operative VAS was 9.4±0.8 compared to post-operative score of 2.9±2.0 at the time of follow-up (Z=4.200, P<0.0005) (Table 2). All patients reported virtually complete abolition of pain immediately following the surgery. In some patients, mild recurrent neck pain occurred approximately 3–4 years following the surgery. Six patients reported ongoing complete abolition of pain (VAS =0). Two of these patients had TAS constructs, 2 had Harms constructs and 2 were hybrid constructs.
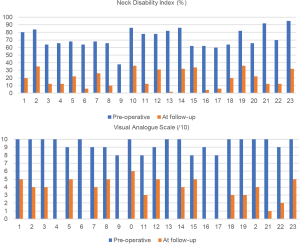
Mean NDI score prior to surgery was 72.2 which reduced to 18.9 post-operatively (Z=4.199, P<0.0005) (Table 2). This represented a statistically significant reduction in debilitation (Figure 3). All patients were classified as “completely” disabled prior to surgery compared to “mild to moderate” post-operatively (12).
Pre and post-operative range of movement measures were identical but significantly decreased compared to age and gender adjusted standards (13). The most affected being lateral rotation. Flexion-extension was relatively preserved. Post-operative mean lateral rotation was 63°±25.1° compared to the age adjusted normal of 150° (Z=4.208, P<0.0005). This is consistent with ankylosis of the C1-C2 joint which provides 50% of lateral rotation depending on age (14). Seven patients reported ongoing asymmetrical rotation in range of movement with reduction towards the pathological side post operatively.
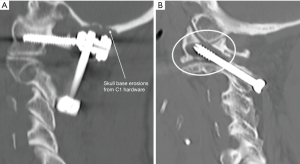
Imaging was performed on 22 patients at follow-up. One patient was unable to have imaging due to geographical remoteness. Twenty-one (95.5%) demonstrated fusion (Figure 2B). Satisfactory position of the construct was found in all 21 patients including the two patients who had undergone revision surgery. Two patients’ scans revealed skull base erosion around the head of the Harms screw (Figure 4A). One patient had a non-union. This patient was an 80-year-old female with a TAS fixation. At 5-year follow-up the patient reported recurrent pain. She had reported 4 years of complete pain relief, after which she developed progressive pain similar to pre-operative. CT scan revealed implant loosening with broken cable and resorption of the bone graft (Figure 4B).
Twenty-one of the 23 patients (91.3%) stated they would undergo the surgery again (Table 1). Two patients were unsure. One of these patients was the patient with non-union and the second was one of the patients in whom skull base erosions were seen.
Discussion
AAOA is a unique clinical syndrome with a natural history that differs from degenerative disorders elsewhere in the spine (1). First described in 1984 (15), patients report unilateral pain localised to the retromastoid, suboccipital and upper cervical region (2,8,9,11,14,16,17). Range of movement is almost always diminished (18). Grob et al. (19) reported patients needed to support their head with both hands while moving it. Some of our patients made similar comments, some needing to rest their head on the table to obtain relief. Some patients obtained relief lying down, others reported they had to sleep upright in a chair in order to tolerate the pain. Surgery was initially considered controversial in the management of AAOA, surgical intervention has now become accepted as appropriate therapy. There have however been relatively few studies reporting outcomes of cervical fusion for AAOA. The only published meta-analysis was published in 2013 of 23 studies containing 246 patients (18).
The diagnosis of AAOA is often delayed, as with many of our patients, due to the initially non-specific nature of symptoms. Many patients in clinical practice present with neck pain and it may be difficult to delineate AAOA pain from other pain generators of the cervical spine (19). The elderly nature of AAOA sufferers as in our series (mean age 67.2 years) perpetuates the difficulty in diagnosis, as all patients had OA involving subaxial facet joints. Until 2002, routine cervical spine CT scans only spanned the C3-T1 spinal segments, hence often not displaying the pathology at C1-C2. Two of our patients reported symptoms of headaches extending to the orbit, more typical of migraine. Some patients reported pain down through the trapezius and shoulder region, more consistent with C3-C4 nerve irritation or muscle spasm. This collection of symptoms, often secondary to the salient pathology, can complicate the diagnosis (1). As a result, many sufferers of AAOA have been enrolled in pain clinics in the absence of a definitive diagnosis (6). Three patients in our series had attended pain clinics and had been prescribed escalating doses of opioids to treat their neck pain. All 3 suffered side effects from the opioid medication including lethargy, nausea, social withdrawal and mental health issues.
The indication for atlantoaxial fixation surgery is the presence of severe pain that is unresponsive to conservative management. Initial management can include NSAIDs, soft collar, physiotherapy, chiropractic manipulation and targeted cortisone injections (14,18,20,21). Some patients reported in the literature have undergone C2 radiofrequency lesioning and ganglionectomy in an effort to alleviate symptoms (6,8). These techniques can be initially effective; however, they fail to address the underlying pathology and symptoms rapidly recur and relentlessly progress. The diagnosis of AAOA is confirmed on bone window CT views of the atlantoaxial joints. Scans reveal unilateral joint space narrowing, obliteration or abolishment of the articular cartilage, osteophyte formation and subchondral sclerosis of the affected joint (1,2,6,14,15,17,18,22). The unaffected joint generally appears normal. MRI scan reports can often miss the joint changes as they can be very subtle, but periarticular oedema can be seen in severe cases. Technetium bone scans generally show avid uptake in the C1-C2 joint (14). All our patients had severe pain (VAS 8 to 10). All had failed conservative treatment.
Internal fixation of the atlantoaxial segment presents a significant surgical challenge to the spine surgeon. The first method reported was posterior wiring by Gallie in 1939 (3) and subsequently Brooks and Jenkins in 1978 (23). This approach had a high rate of pseudoarthrosis with non-union rates of up to 30% (24-26). Magerl and Seemann’s technique of TAS fixation achieved more rigid fixation as did the pedicle screw fixation method pioneered by Goel and Laheri in 1995 (27) and popularised by Harms and Melcher. Both methods have demonstrated fusion rates greater than 95% (2,5-10,17,19,28-32).
Two patients in our series demonstrated skull base erosions as a result of the close proximity of the C1 screw heads to the inferior occiput (Figure 4A). One patient, a 71-year-old female who did not achieve fusion following her initial TAS fixation, underwent revision surgery one year later. The hardware was removed and replaced with lateral mass screws. One year later after initial relief of symptoms, she developed right sided neck pain. Imaging revealed stable fusion, however she had developed significant skull base erosion (Figure 4A). The C1 screws were subsequently removed with alleviation of the pain. The second patient, a 66-year-old female, developed right sided suboccipital pain 1 year following the surgery. CT scan revealed similar skull base erosions, more marked on the right side. This complication has not been previously reported in the literature.
Two patients in our series reported mild swallowing difficulties. The aetiology of the dysphagia in our patients is unclear. Dysphagia has been reported following surgery at C1 due to hypoglossal nerve dysfunction (5,33,34). Intraoperative stereotactic guidance was used in all our patients and all screws were in satisfactory position on post-operative imaging with no screws extending anterior to the C1 vertebra.
Unilateral anatomical anomalies such as a high riding vertebral artery can result in the need for hybrid surgical techniques, i.e., the use of pedicle screw instrumentation on one side with trans-articular fixation on the other (Figure 5). Only one study has previously reported this type of construct (11). The eight patients in this series who had hybrid fixations achieved identical results to those who received either solely TAS constructs or Harms constructs. The method of fixation was decided at the time of the surgery when precise screw trajectory could be best assessed via stereotactic image guidance (BrainLab).
All 23 patients reported an immediate improvement in pain scores (VAS) following surgery (mean VAS 9.4±0.8 pre-operatively to 2.9±2.0 at time of follow-up). Most patients reported complete alleviation of pain initially following surgery. Longer term follow-up time resulted in slight increase in post-operative pain scores, possibly due to symptomatic subaxial arthritic degeneration. All patients had significant degenerative changes of the subaxial cervical facet joints on the CT and it is difficult to be certain if these are symptomatic. Studies on asymptomatic adults have shown significant degenerative changes at one or more cervical levels in 70% of women and 90% of men aged 60–65 (35), similar to our patient cohort. Studies into adjacent segment disease from subaxial fusions have been extensively reported from an anterior approach (36), however, there are no published reports on adjacent segment degeneration following C1-C2 fusion. None of the patients in our series have required surgery on adjacent segments since their atlantoaxial fixation.
All 23 patients reported dramatic improvement in NDI scores. The attempt to use a quantitative scoring system such as NDI for neck disability is beneficial for analysis and external validity, however it is not ideal for atlantoaxial pathology. Some sections were invalid for our patients and left them unsure how to respond, e.g., many found difficulty driving post-operatively but this was due to lack of mobility rather than pain. Further, our patients had many comorbidities and these affected their activities of daily living more than their neck pain. Regardless, it is important to note that every patient reported a substantially decreased NDI following their surgery (72.2±13 to 18.9±12).
Negative subjective patient outcomes were generally related to the reduced range of movement. Between 30–80% of lateral rotation occurs at the C1-C2 joint and fixation leads to a reduced range of movement. Mean total rotation of the patients was 63°±25.1° which represents a 58% decrease from age adjusted normal of 150° (13). Many patients reported preferring to sit at the end of the table during communal meals in order to minimise head movement. Pre-operative and post-operative driving were by far the most affected activity. The most common concern being the lack of lateral rotation compromising their safety on the road.
Despite this, 21 (91.3%) out of the 23 patients reported they were very satisfied with the surgery and would have it performed again. Diminished range of movement was not a deterrent to the patients. Most patients had virtually no lateral rotation pre-operatively as it was limited by pain. There was no difference in range of movement between pre-operative and post-operative movement, it was a case of being restricted with pain pre-operatively, to being restricted without pain post-operatively. Grob et al. (19) similarly reported that 83% of patients (24 out of 29) in their series would undergo the procedure again. Multiple studies show the biggest factor dictating satisfaction with the surgery was the alleviation of pain (2,8,9,14,19,22,37). We compared our outcome to that of hip arthroplasty patients who are acknowledged as being amongst the most satisfied surgical cohorts of degenerative joint surgery. Dailiana et al. (38) reported on 174 total hip arthroplasty patients at one year post-operatively and 87.5% were satisfied. Mancuso et al. (39) reported satisfaction in 89% of their hip replacement cohort. Our patients report satisfaction with their surgery of greater than 90%. This indicates that posterior atlantoaxial fixation is a highly successful surgical technique for the treatment of symptomatic AAOA.
Our study has the limitation that it is not a randomised-controlled trial. All patients presenting to the senior surgeon (T Steel) presented with severe neck pain requesting intervention if possible. This patient cohort had tried many non-surgical treatments without relief and were prepared to undergo surgery after detailed discussion of the pathophysiology of symptoms and explanation of surgery. All patients were offered diagnostic and/or therapeutic CT-guided C1-C2 intra-articular injections. Some declined, and elected to proceed directly to surgery.
Conclusions
Posterior cervical fixation is a highly effective technique for the surgical treatment of neck pain secondary to atlantoaxial lateral mass osteoarthritis (AAOA) that has failed to respond to conservative measures. The surgery is safe and offers a very high rate of symptom relief. Transarticular screw and pedicle screw fusions can be used in combination with each other to adapt to anatomical and pathological variability while maintaining an extremely high surgical success rate.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Ethical Statement: Ethics approval was obtained from St Vincent’s Hospital Human Research Ethics Committee (SVH file number: 16/054).
References
- Halla JT, Hardin JG Jr. Atlantoaxial (C1-C2) facet joint osteoarthritis: a distinctive clinical syndrome. Arthritis Rheum 1987;30:577-82. [Crossref] [PubMed]
- Schaeren S, Jeanneret B. Atlantoaxial osteoarthritis: case series and review of the literature. Eur Spine J 2005;14:501-6. [Crossref] [PubMed]
- Gallie WE. Fractures and dislocations of the cervical spine. Am J Surg 1939;46:495-9. [Crossref]
- Magerl F, Seemann PS. Stable Posterior Fusion of the Atlas and Axis by Transarticular Screw Fixation. In: Kehr P, Weidner A. editors. Cervical Spine I. Springer, Vienna, 1987:322-7.
- Grob D, Jeanneret B, Aebi M, et al. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br 1991;73:972-6. [Crossref] [PubMed]
- Holly LT, Batzdorf U, Foley KT. Treatment of severe retromastoid pain secondary to C1-2 arthrosis by using cervical fusion. J Neurosurg 2000;92:162-8. [PubMed]
- Neo M, Matsushita M, Iwashita Y, et al. Atlantoaxial transarticular screw fixation for a high-riding vertebral artery. Spine 2003;28:666-70. [Crossref] [PubMed]
- Kuklo TR, Riew KD, Orchowski JR, et al. Management of recalcitrant osteoarthritis of the atlanto-axial joint. Orthopedics 2006;29:633-8. [PubMed]
- Finn M, Fassett DR, Apfelbaum RI. Surgical treatment of nonrheumatoid atlantoaxial degenerative arthritis producing pain and myelopathy. Spine 2007;32:3067-73. [Crossref] [PubMed]
- Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 2001;26:2467-71. [Crossref] [PubMed]
- Kang DG, Lehman RA Jr, Wagner SC, et al. Outcomes Following Arthrodesis for Atlanto-Axial Osteoarthritis. Spine (Phila Pa 1976) 2017;42:E294-303. [Crossref] [PubMed]
- Vernon H. The Neck Disability Index: state-of-the-art, 1991-2008. J Manipulative Physiol Ther 2008;31:491-502. [Crossref] [PubMed]
- Dvorak J, Antinnes JA, Panjabi M, et al. Age and gender related normal motion of the cervical spine. Spine (Phila Pa 1976) 1992;17:S393-8. [Crossref] [PubMed]
- Star MJ, Curd JG, Thorne RP. Atlantoaxial lateral mass osteoarthritis. A frequently overlooked cause of severe occipitocervical pain. Spine (Phila Pa 1976) 1992;17:S71-6. [Crossref] [PubMed]
- Ehni G, Benner B. Occipital neuralgia and the C1-2 arthrosis syndrome. J Neurosurg 1984;61:961-5. [Crossref] [PubMed]
- Dickman CA, Sonntag VK, Papadopoulos SM, et al. The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg 1991;74:190-8. [Crossref] [PubMed]
- Goel A, Shah A, Gupta SR. Craniovertebral instability due to degenerative osteoarthritis of the atlantoaxial joints: analysis of the management of 108 cases. J Neurosurg Spine 2010;12:592-601. [Crossref] [PubMed]
- Elliott RE, Tanweer O, Smith ML, et al. Outcomes of fusion for lateral atlantoaxial osteoarthritis: Meta-analysis and review of literature. World Neurosurg 2013;80:e337-46. [Crossref] [PubMed]
- Grob D, Bremerich FH, Dvorak J, et al. Transarticular screw fixation for osteoarthritis of the atlanto axial segment. Eur Spine J 2006;15:283-91. [Crossref] [PubMed]
- Chevrot A, Cermakova E, Vallee C, et al. C1-2 arthrography. Skeletal Radiol 1995;24:425-9. [Crossref] [PubMed]
- Yu H, Hou S, Wu W, et al. Upper cervical manipulation combined with mobilization for the treatment of atlantoaxial osteoarthritis: a report of 10 cases. J Manipulative Physiol Ther 2011;34:131-7. [Crossref] [PubMed]
- Ghanayem AJ, Leventhal M, Bohlman HH. Osteoarthrosis of the atlanto-axial joints. Long-term follow-up after treatment with arthrodesis. J Bone Joint Surg Am 1996;78:1300-7. [Crossref] [PubMed]
- Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am 1978;60:279-84. [Crossref] [PubMed]
- Dickman CA, Sonntag VK. Posterior C1-C2 transarticular screw fixation for atlantoaxial arthrodesis. Neurosurgery 1998;43:275-80; discussion 280-1. [Crossref] [PubMed]
- Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus transarticular screw fixation in C1-C2 fusion. Clin Orthop Relat Res 1999.126-35. [Crossref] [PubMed]
- Coyne TJ, Fehlings MG, Martin RJ. C1-C2 transarticular screw fixation for treatment of C1-C2 instability. J Clin Neurosci 1996;3:243-6. [Crossref] [PubMed]
- Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47-53. [Crossref] [PubMed]
- Weidner A, Wähler M, Chiu ST, et al. Modification of C1-C2 transarticular screw fixation by image-guided surgery. Spine (Phila Pa 1976) 2000;25:2668-73; discussion 2674. [Crossref] [PubMed]
- Stulik J, Vyskocil T, Sebesta P, et al. Atlantoaxial fixation using the polyaxial screw-rod system. Eur Spine J 2007;16:479-84. [Crossref] [PubMed]
- Stulík J, Barna M, Kryl J. Surgical treatment for atlantoaxial osteoarthritis (AAOA): a prospective study of twenty-seven patients. Acta Chir Orthop Traumatol Cech 2012;79:31-6. [PubMed]
- Jin KO, Kim YW, Rim DC, et al. Surgical treatment of the atlantoaxial osteoarthritis. J Korean Neurosurg Soc 2007;41:264-6. [Crossref]
- Payer M, Luzi M, Tessitore E. Posterior atlanto-axial fixation with polyaxial C1 lateral mass screws and C2 pars screws. Acta Neurochir (Wien) 2009;151:223-9; discussion 229. [Crossref] [PubMed]
- Bekelis K, Gottfried ON, Wolinsky JP, et al. Severe dysphagia secondary to posterior C1-C3 instrumentation in a patient with atlantoaxial traumatic injury: a case report and review of the literature. Dysphagia 2010;25:156-60. [Crossref] [PubMed]
- Hong JT, Lee SW, Son BC, et al. Hypoglossal nerve palsy after posterior screw placement on the C-1 lateral mass: case report. J Neurosurg Spine 2006;5:83-5. [Crossref] [PubMed]
- Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976) 1986;11:521-4. [Crossref] [PubMed]
- Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion?. Spine J 2004;4:190S-194S. [Crossref] [PubMed]
- Grob D, Luca A, Mannion AF. An observational study of patient-rated outcome after atlantoaxial fusion in patients with rheumatoid arthritis and osteoarthritis. Clin Orthop Relat Res 2011;469:702-7. [Crossref] [PubMed]
- Dailiana ZH, Papakostidou I, Varitimidis S, et al. Patient-reported quality of life after primary major joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Musculoskelet Disord 2015;16:366. [Crossref] [PubMed]
- Mancuso CA, Salvati EA, Johanson NA, et al. Patients' expectations and satisfaction with total hip arthroplasty. J Arthroplasty 1997;12:387-96. [Crossref] [PubMed]