
Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation
Introduction
Lateral access surgery has seen an increase in popularity among spine surgeons since its initial introduction (1-3). The transpsoas approach provides access to the lumbar spine with relatively predictable anatomy and obviates the need for an access surgeon (4,5). Lateral access surgery is performed in the lateral decubitus position and the discectomy, endplate preparation, and interbody insertion are all performed while the patient remains in the lateral position. Once the interbody has been inserted, traditionally, the wounds are closed and the patient is repositioned prone for pedicle screw fixation (1). The repositioning requires completing a second round of prepping, draping, and room positioning, which may add significant time to the case and increase the risk of contamination.
The lateral position tends to be better tolerated by the patient compared to prone surgery and avoids many of the major concerns that exist with prone positioning including but not limited to: postoperative vision loss, cardiovascular complications, hypovolemia, reduced pulmonary compliance, and cardiac arrest (6-8). Concern exists regarding theoretical disadvantages of completing the entire surgery in the lateral position, namely inadequate correction of lumbar lordosis as well as difficulty with placing bilateral pedicle screws. To date, correction of lordosis has not been compared between lateral only and lateral-then-prone approaches.
This study investigates the short-term (two-year) outcomes of two cohorts: one that underwent single position surgery for the interbody and posterior pedicle screw placement (SP) and a second cohort that underwent the more traditional approach of dual positioning (DP), first being placed in the lateral position for the interbody and then being turned prone for pedicle screw fixation. Our goal was to determine whether there were differences in perioperative and radiographic outcomes between SP and DP surgery.
Methods
This retrospective chart review was approved by the Stanford University institutional review board #7935. All consecutive lumbar interbody fusions performed via lateral access (SP or DP) from a single surgeon (IC) from January 2012 to December 2015 were eligible for study inclusion. Nearly all SP patients were consecutive surgeries.
Patient population and data collection
Inclusion criteria were patients over the age of 18 undergoing extreme lateral interbody fusion for any degenerative lumbar pathology. Exclusion criteria included patients with a history of retroperitoneal surgery, those with inadequate preoperative imaging available for review, and patients undergoing combined procedures including direct posterior decompression, trans-foraminal lumbar interbody fusion, posterior lumbar interbody fusion, or anterior lumbar interbody fusion. Of note, patients who had previously undergone a spinal fusion above or below the level of interest were not excluded.
In total, 56 SP and 50 DP were identified. Fourteen SP and 26 DP patients were excluded due to additional procedures or incomplete imaging. The final cohort consisted of 42 patients in the SP group and 24 in the DP group. Patient demographics [age, sex, and body mass index (BMI)] and surgical details (previous lumbar spine surgeries, indications for surgery, and number of operative spinal levels) were recorded. Imaging consisted of preoperative and postoperative anteroposterior (AP) and lateral lumbar films with measurement of overall and segmental lordosis. A senior orthopaedic resident who remained independent of the surgeries measured the radiographs and was blinded to the differences in positioning. Surgical characteristics investigated included estimated blood loss, operating room time, unilateral versus bilateral pedicle screw fixation, the pre- to post-operative change in overall and segmental lordosis, length of stay, and the presence of postoperative complications (both medical and surgical within 90 days).
Surgical technique
Patients were all placed in the lateral decubitus position for the lateral approach, discectomy, interbody sizing, and placement. The SP group then remained in the lateral decubitus position for percutaneous pedicle screw fixation. The DP group was turned to the prone position and then re-prepped and draped. Percutaneous pedicle screw fixation was then performed in the prone position.
Statistical methods
Data distributions were evaluated with histograms and quantile-quantile plots. Univariate differences between SP and DP were assessed with independent samples t-tests or Mann-Whitney U tests (if non-normally distributed) for continuous variables and chi-squared or Fisher’s exact tests for categorical variables. Segmental lordosis was tested by segment with a Mann-Whitney U test, and additionally all operated segments were considered together and differences were assessed with a repeated measures generalized estimating equation (GEE). A GEE analysis was also used to investigate differences in OR time between groups after adjustment for other factors. Candidates for this model included any factors with P<0.20 in univariate tests for the differences between groups. All analyses were performed in SAS version 9.4 (Cary, NC, USA) with a two-sided level of significance of α=0.05.
Results
The final cohort included 66 patients (42 SP, 24 DP) with a mean age of 67.6±11.3 years and a mean BMI of 27.3±5.2. In total, 59.1% of the patients were female. Most individuals never had a previous lumbar spine surgery (65.2%), and those who did had either a laminectomy (10.6%), partial laminectomy (7.6%), anterior fusion (7.6%), or posterior fusion (3.0%). The remaining 6.0% of patients each had either a hemilaminectomy, microdiscectomy, combination of a posterior fusion with a laminectomy, or combination of a partial laminectomy and microdiscectomy. The most common indications for lumbar interbody fusion surgery in this study included degenerative spondylolisthesis (65.2%), degenerative scoliosis (21.2%), and both degenerative spondylolisthesis and degenerative scoliosis (7.6%). Other indications included junctional disc herniation, degenerative disk with angular instability, adjacent segment disease, and fixed sagittal imbalance, with only one patient diagnosed with each respective condition.
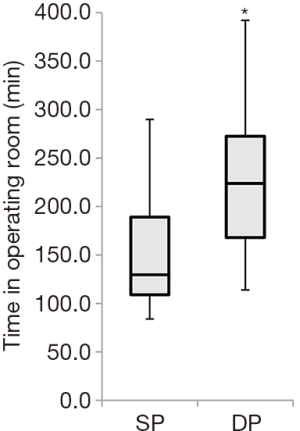
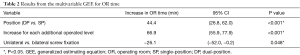
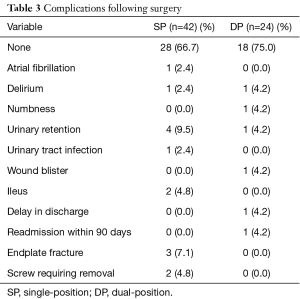
There were no differences observed between SP and DP for age, sex, BMI, estimated blood loss, length of stay, or number of operative spinal levels in univariate tests (Table 1). However, OR time was longer for DP (226.1±74.9 minutes) than SP (149.2±53.2 minutes, P<0.001) (Figure 1, Table 1). Multivariable analysis controlling for number of levels operated identified an operative time difference of 44 minutes (P<0.05) (Table 2). Over two-thirds of patients had no complications, and there was no difference in the overall rate of complications between groups (33.3% SP, 25.0% DP, P=0.479) (Table 1). Complications included atrial fibrillation, delirium, numbness, urinary retention, urinary tract infection, wound blister, ileus, delay in discharge, readmission with 90 days, endplate fracture, and suboptimal screw placement requiring removal (Table 3). The statistical power was too small to compare individual complications. No significant differences were observed in pre- or post-operative overall lordosis or the change in overall lordosis (P>0.200 for each) (Figure 2, Table 1). Similarly, there were no significant differences in segmental lordosis, either when tested by individual operated level, or when considering all operative levels together (P>0.600 for each) (Figure 3, Table 1).
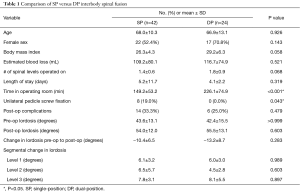
Full table
Full table
Full table


There was a greater percentage of individuals in the SP group that had unilateral pedicle screw placement (19.0%) compared to 0.0% in the DP group (P=0.043) (Table 1). These patients were early in the collection period and there was noted to be a high rate of subsidence so unilateral pedicle screw placement was not continued during subsequent surgeries. Individuals with unilateral pedicle screw placement versus bilateral placement were more likely to be female (88% versus 44%, P=0.047), had less operative time (102.6±22.6 versus 160.2±52.5 min, P=0.001), had a smaller pre- to post-operative change in lordosis (−5.2±4.2 versus −11.6±6.4 degrees, P=0.005), and had fewer operative levels (1.0±0.7 versus 1.5±0.0 levels, P=0.042). All other outcomes did not differ significantly between unilateral and bilateral screw placement, and excluding the unilateral screw patients from the univariate SP versus DP comparisons did not change the study findings.
In multivariable models, OR time remained different between groups (P<0.001), even after adjusting for the number of levels operated (P<0.001) and unilateral versus bilateral screw placement (P=0.048) (Table 2). OR time remained 44.4 (95% CI: 26.8–62.0) minutes longer for DP than SP after this adjustment. OR time was 66.9 (95% CI: 55.9–77.9) minutes longer for each additional level operated, but was 26.1 (95% CI: 0.2–52.0) minutes shorter for unilateral versus bilateral screw placement.
Discussion
The prone position is typically utilized for spine surgeries requiring a posterior approach to the spinal column. Despite its convenience in terms of ease of access, the prone position carries with it significant and well-documented risks that can result in permanent disability (6-8). Coupled with the trend towards value based healthcare, considerations of alternative forms of surgical techniques that decrease operative times without compromising patient safety and surgical outcomes deserve investigation (9,10). This study builds on the previous work of Blizzard and Thomas, which was a case series on SP surgery (11). We found no differences in primary endpoints including estimated blood loss, complication rate, and lumbar lordosis correction.
The primary finding of this study relates to operative time. Operative time for DP was on average 44 minutes longer than for SP after adjusting for other factors. The majority of this time is very likely due to the need to reposition, re-prep, and re-drape the patient when transitioning from a lateral to prone position. A time saving of 44 minutes for SP surgery after controlling for the number of levels operated on and unilateral versus bilateral screw placement is substantial. Case duration has been shown to correlate with delay to extubation (7). Kim et al. looked specifically at the effect of operative time on complication rate in a multicenter retrospective cohort review and found a step-wise increased risk for overall complications, medical complications, surgical complications, superficial surgical site infections, and postoperative transfusions particularly related to single level lumbar fusion surgery (12). Similar findings in other studies support this conclusion (13-15). We therefore suggest that surgeons who frequently perform lateral surgery, especially those at high volume centers, may want to consider implementation of SP surgery.
Interestingly, post-operative lordosis did not differ between groups, nor did the pre- to post-operative change in lordosis. This suggests that adequate restoration of lordosis can be obtained in the lateral decubitus position primarily through the interbody work. Proponents of DP surgery often argue that optimum restoration of lordosis can only be achieved in the prone position due to accentuated lumbar lordosis from the operative table (16,17)). These cited works would argue that placing the patient prone on the table allows for more lordosis to be gained at the time of posterior instrumentation due in large part to Jackson frame. This study, while limited in size, would suggest that adequate lordosis can be achieved entirely in the lateral position with no additional advantage of repositioning for posterior fixation.
Complications related to prone positioning can be profound. Perhaps the most devastating complication is postoperative visual loss (POVL), first described in the 1950’s (18). The incidence of POVL is approximately 3.00/10,000 (0.03%) after spinal fusion (19). While the etiology is somewhat debated and remains unclear, prone positioning has been implicated as a major risk for the development of posterior ischemic optic neuropathy (PION) and prevention is crucial as there exists a lack of validated treatment options (20-22). Central retinal artery occlusion, cortical blindness, and subconjunctival hemorrhage have all been implicated in prone positioning complications (20,23). While overall risk of developing POVL is extremely low and did not occur in any of the patients in this study, the benefits of single position surgery are that increased intraocular pressure can be minimized. Prone positioning during surgery is also associated with reduced stroke volume and cardiac index, raised central venous pressures, and low blood pressure (6). Hypovolemia in the setting of a major spine surgery, coupled with hypovolemia related to prone positioning, can be problematic. For this and the aforementioned reasons, procedures that can be carried out in the lateral decubitus position, alone, certainly warrant investigation.
Additional concerns regarding placement of pedicle screws and increased potential for pedicle breach in the lateral position have been discussed in the literature (11). Blizzard and Thomas evaluated SP surgery for pedicle screw accuracy and found results in their cohort that were consistent with published rates of breach for prone surgery, further strengthening the role of SP surgery for the appropriate patient. Blizzard and Thomas did not have a comparison cohort of prone positioned patients and did not comment on degree of lordosis achieved, or other perioperative outcome measures, which are included in the current study (11).
Two patients in the SP cohort required eventual return to the operating room for removal of symptomatic pedicle screws. It should be stated that there is certainly a learning curve to pedicle screw insertion in the lateral position. Orthogonal triangulation of start sites and screw trajectory can be challenging initially but alleviated with the assistance of intraoperative fluoroscopy. The senior author began performing single position surgery in 2012. The patients that required screw removal were number 28 and 32 in the series of SP surgery. One patient had symptoms from a downside screw, and the other from the upside.
Complication rates did not differ widely between the two groups. Of note, this study was underpowered to detect differences in complications, particularly when considered individually. Four patients in the SP group had postoperative urinary retention requiring Foley insertion. While some risk factors may be unavoidable, namely retroperitoneal dissection with the transpsoas approach, judicious use of intravenous fluids, avoidance of epidural analgesia, and shorter surgery obviate the need for Foley catheter placement and may lower the rate of retention (24). Endplate breach and early subsidence was noted in three of the single position patients. While not requiring revision surgery, this is concerning. All three occurred in women and one patient had unilateral pedicle screw fixation. Bone quality is a contributing factor to endplate stability. While biomechanical studies have demonstrated an effect on range of motion and potential compromise of decompression, the clinical relevance is poorly defined (25). None of the three patients with breach required reoperation and all had good relief of symptoms with follow up imaging consistent with fusion.
Retrospective cohort studies have limitations. Selection bias applies to our two cohorts given a single surgeon was indicating them for surgery. Additionally all surgeries were performed at a single center by a single surgeon. While there could be some bias due to the experience and patient population of the single surgeon, we feel that the single surgeon cohort creates a more uniform cohort for study, especially given the fact that data was collected from a consecutive series of cases. Having all surgeries performed by the same surgeon provides a uniform sampling of operative time, technique and experience, and while not applicable to surgeons not performing lateral access surgery, this data suggests that close to one hour of operative time can be eliminated without influencing blood loss or length of stay. An additional limitation is the inclusion of patients who underwent unilateral pedicle crew fixation. This could potentially lower operative time and skew results. This was adjusted for in multivariable models and unilateral screw placement was on average 26 minutes shorter compared to bilateral placement. A further limitation of this study is the lack of evaluation of screw trajectory and position. CT scans were not routinely obtained postoperatively to assess fusion or screw position. It should be noted that two patients in the SP group required revision of a single pedicle screw each due to persistent post-operative radiculopathy but this remain consistent with previously published rates of suboptimal screw placement (26).
Conclusions
We compared a single surgeon’s perioperative characteristics for single position and dual position lateral lumbar fusions. In the single position the entire lumbar procedure including approach, discectomy, interbody placement, and percutaneous screw fixation is performed in the lateral decubitus position. Most notably, single position surgery decreased the mean operative time by 44 minutes after adjusting for other factors with no differences in blood loss, length of stay, lordosis correction or overall rate of complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: Cheng—Nuvasive, Royalties, consulting; Globus Medical, Royalties; Stryker Spine, Consulting; Spine Wave, Royalties; SpineCraft, Consulting; Cytonics, Stock; Spine Innovations, Stock; SpinalCyte, Stock. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Stanford University institutional review board (#7935).
References
- Ozgur BM, Aryan HE, Pimenta L, et al. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 2006;6:435-43. [Crossref] [PubMed]
- Berjano P, Balsano M, Buric J, et al. Direct lateral access lumbar and thoracolumbar fusion: preliminary results. Eur Spine J 2012;21 Suppl 1:S37-42. [Crossref] [PubMed]
- Formica M, Berjano P, Cavagnaro L, et al. Extreme lateral approach to the spine in degenerative and post traumatic lumbar diseases: selection process, results and complications. Eur Spine J 2014;23 Suppl 6:684-92. [Crossref] [PubMed]
- Hu WK, He SS, Zhang SC, et al. An MRI study of psoas major and abdominal large vessels with respect to the X/DLIF approach. Eur Spine J 2011;20:557-62. [Crossref] [PubMed]
- Kepler CK, Bogner EA, Herzog RJ, et al. Anatomy of the psoas muscle and lumbar plexus with respect to the surgical approach for lateral transpsoas interbody fusion. Eur Spine J 2011;20:550-6. [Crossref] [PubMed]
- Kwee MM, Ho YH, Rozen WM. The prone position during surgery and its complications: a systematic review and evidence-based guidelines. Int Surg 2015;100:292-303. [Crossref] [PubMed]
- Anastasian ZH, Gaudet JG, Levitt LC, et al. Factors that correlate with the decision to delay extubation after multilevel prone spine surgery. J Neurosurg Anesthesiol 2014;26:167-71. [Crossref] [PubMed]
- DePasse JM, Palumbo MA, Haque M, et al. Complications associated with prone positioning in elective spinal surgery. World J Orthop 2015;6:351-9. [Crossref] [PubMed]
- Macario A. What does one minute of operating room time cost? J Clin Anesth 2010;22:233-6. [Crossref] [PubMed]
- Tan JM, Macario A. How to evaluate whether a new technology in the operating room is cost-effective from society's viewpoint. Anesthesiol Clin 2008;26:745-64. viii. [Crossref] [PubMed]
- Blizzard DJ, Thomas JA. MIS Single-position Lateral and Oblique Lateral Lumbar Interbody Fusion and Bilateral Pedicle Screw Fixation: Feasibility and Perioperative Results. Spine (Phila Pa 1976) 2018;43:440-6. [PubMed]
- Kim BD, Hsu WK, De Oliveira GS Jr, et al. Operative duration as an independent risk factor for postoperative complications in single-level lumbar fusion: an analysis of 4588 surgical cases. Spine (Phila Pa 1976) 2014;39:510-20. [Crossref] [PubMed]
- Peersman G, Laskin R, Davis J, et al. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J 2006;2:70-2. [Crossref] [PubMed]
- Ball CG, Pitt HA, Kilbane ME, et al. Peri-operative blood transfusion and operative time are quality indicators for pancreatoduodenectomy. HPB (Oxford) 2010;12:465-71. [Crossref] [PubMed]
- Cheng H, Chen BP, Soleas IM, et al. Prolonged Operative Duration Increases Risk of Surgical Site Infections: A Systematic Review. Surg Infect (Larchmt) 2017;18:722-35. [Crossref] [PubMed]
- Yson SC, Sembrano JN, Santos ER, et al. Does prone repositioning before posterior fixation produce greater lordosis in lateral lumbar interbody fusion (LLIF)? J Spinal Disord Tech 2014;27:364-9. [Crossref] [PubMed]
- Harimaya K, Lenke LG, Mishiro T, et al. Increasing lumbar lordosis of adult spinal deformity patients via intraoperative prone positioning. Spine (Phila Pa 1976) 2009;34:2406-12. [Crossref] [PubMed]
- Hollenhorst RW, Svien HJ, Benoit CF. Unilateral blindness occurring during anesthesia for neurosurgical operations. AMA Arch Ophthalmol 1954;52:819-30. [Crossref] [PubMed]
- Shen Y, Drum M, Roth S. The prevalence of perioperative visual loss in the United States: a 10-year study from 1996 to 2005 of spinal, orthopedic, cardiac, and general surgery. Anesth Analg 2009;109:1534-45. [Crossref] [PubMed]
- Nandyala SV, Marquez-Lara A, Fineberg SJ, et al. Incidence and risk factors for perioperative visual loss after spinal fusion. Spine J 2014;14:1866-72. [Crossref] [PubMed]
- Stambough JL, Dolan D, Werner R, et al. Ophthalmologic complications associated with prone positioning in spine surgery. J Am Acad Orthop Surg 2007;15:156-65. [Crossref] [PubMed]
- Li A, Swinney C, Veeravagu A, et al. Postoperative Visual Loss Following Lumbar Spine Surgery: A Review of Risk Factors by Diagnosis. World Neurosurg 2015;84:2010-21. [Crossref] [PubMed]
- Akhaddar A, Boucetta M. Subconjunctival hemorrhage as a complication of intraoperative positioning for lumbar spinal surgery. Spine J 2012;12:274. [Crossref] [PubMed]
- Darrah DM, Griebling TL, Silverstein JH. Postoperative urinary retention. Anesthesiol Clin 2009;27:465-84. table of contents. [Crossref] [PubMed]
- Santoni BG, Alexander GE 3rd, Nayak A, et al. Effects on inadvertent endplate fracture following lateral cage placement on range of motion and indirect spine decompression in lumbar spine fusion constructs: A cadaveric study. Int J Spine Surg 2013;7:e101-8. [Crossref] [PubMed]
- Rivkin MA, Yocom SS. Thoracolumbar instrumentation with CT-guided navigation (O-arm) in 270 consecutive patients: accuracy rates and lessons learned. Neurosurg Focus 2014;36:E7. [Crossref] [PubMed]


