A Colombian experience involving SpineJack®, a consecutive series of patients experiencing spinal fractures, percutaneous approach and anatomical restoration 2016–2017
Introduction
Spinal fractures are becoming more frequent and should be handled as a severe and endemic pathology that requires timely diagnosis and adequate treatment; however, ambulatory care of spinal injuries is more common than inpatient care. Fractures are more common in young men (trauma) and in adult women (osteoporosis). Thoracic location represents 33% of the cases compared to 46% of the lumbar; global mortality amounts to 4–5% (1).
Methods
A clinical follow-up was performed to 20 consecutive patients experiencing spinal compression fractures (SCF) who, prior informed consent, where all subject of both pain and disability measurements using a visual analog scale (VAS) for the first and the Oswestry Low Back Pain Questionnaire/Oswestry Disability Index (ODI) (2). These patients had spinal fracture reduction procedures done through percutaneous way with expander endovertebral implants, and intraosseous fixation using SpineJack® intravertebral implants plus Cohesion® cement. Within the follow-up scheme, subsequent measurements were taken after a week, a month after surgery, 3 months after the procedure and after 6 months of follow-up.
STATA® (Statistical Analysis System, version 12.1, SAS Institute Inc., Cary, NC, USA) was used for all analyzes. Group comparisons were used to see the effect in time, that is to say, the evolution between the starting value and the follow-up visits.
The Wilcoxon or Student’s t-test was used for comparisons in pairs depending on the normality of the distribution. The P value was set at 0.05 to reject the null hypothesis.
It does not require any approval of the ethics committee, since it is a study which only followed they; the patients were not intervened, by us.
Results
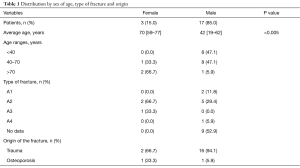
As seen in Table 1, cases were more frequent among men than women with a significant difference in the average age. This type of fractures has been more often reported in young men, secondary to trauma, and in adult women, related to osteoporosis. In general, the most frequent type of fracture on which this procedure has been used, on this series of cases, is the A2 from the AOSpine classification (3).
Full table
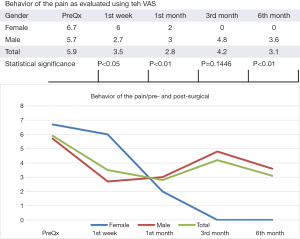
A decrease in pain was evidenced by the difference between mean values of pain scores prior to the procedures and those from 6 months afterwards: from 5.9 (95% CI, 4.76–7.09) down to 3.1 (95% CI, 1.17–4.98), P<0.01, as seen in Figure 1.
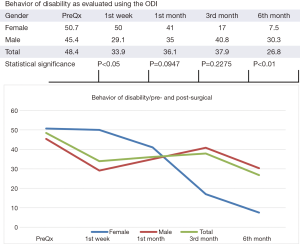
In Figure 2, It is found the behavior of the ODI-assessed disabilities: prior to surgery, the average was found at 48.4/100 (95% CI, 38.33–58.53) then, in the evaluations done 6 months after surgery, the average was 26.8/100 (95% CI, 13.31–40.23), P<0.01.
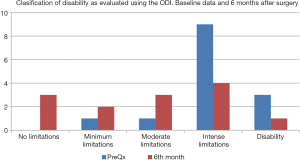
According to classifications of disability from the pre-surgical screenings, 85.7% (95% CI, 67.4–100%) of the patients had severe functional limitation or disability, representing a statistically significant difference against the 6 months evaluation results where only 38.5% (95% CI, 12–65%) presented limitation to this degree, P<0.05, as seen on Figure 3.
Discussion
Thoracolumbar compression fractures correspond to type A classification by AOSpine. This type of classification is divided in three big groups depending on specific pattern of fracture. A0 means that there is not fracture or is fracture clinically insignificant of the spinous transverse processes; A1 belongs to single endplate fracture without involvement of the posterior wall; A2 corresponds to fracture line that involves both endplates but does not involve the posterior wall; A3 injuries are fractures of a single endplate with any involvement of the posterior vertebral wall and the spinal canal; finally, A4 injuries are vertebral body fractures that involve both endplates and the posterior wall (3). Osteoporosis is the most common etiology for vertebral compression fractures, which gives patients a condition of very difficult pain control, followed by trauma. Between the classical surgical established managements is vertebroplasty or kyphoplasty, overall in refractory to conventional treatments including drugs, braces and rehabilitation (4). The first was described initially for treatment for vertebral angiomas (5), since then it has been established for the treatment of malignant vertebral condition as well as benign (6). This procedure can be realized under imaging guidance, and consist in insert a gross needle to the vertebral body affected via transpedicular for injection of methyl methacrylate (7). A 2018 Cochrane revision (8), showed that percutaneous vertebroplasty had significant improvement in pain, disability with high quality of evidence, compared with placebo.
By other side, the kyphoplasty, more specific the balloon kyphoplasty, was performed for first time in 1998 and includes the inflation of balloon to restore the vertebral height (4), by this way correcting and prevent the deformity, not only doing fixation of the fracture (9). This type of management has been demonstrated to be more effective than medical for the osteoporotic fractures (4), but in the majority of this studies don’t include compression fractures that don’t be osteoporotic. Even though, it effectiveness have been elucidated, it is not better that vertebroplasty.
Chang et al. run out and systematic review evaluating the efficacy for osteoporotic vertebral fractures between vertebroplasty and kyphoplasty, in this study (10) they raised that the two procedures are almost equally effective for the management of pain and vertebral stabilization (10), in the context of osteoporotic fractures only. Also, Hulme et al. reported that 95% of pain and vertebral dysfunction could get better with any of the two surgical procedures (11). However, being more specific, the Cobb angle was similar in the two surgical procedures; the postoperative vertebral height was significant more in favor to kyphoplasty (10).
In other hand, regard to complications, the kyphoplasty have shown that the major of its complications is an increase rate of incident fractures, overall in adjacent vertebra to he treated one (12). In vertebroplasty, the complications can go from milder like cement leakage into disc or paravertebral soft tissue without clinical consequences, to severe complications like cement leakage to paravertebral veins leading to pulmonary embolism, cardiac perforation, cerebral infarction or even death (13). Nevertheless, in general the difference regard to the rate of complications has been significantly minor in percutaneous vertebroplasty (10).
The percutaneous vertebroplasty and kyphoplasty doesn’t have too many differences in prognosis and complications. Even the kyphoplasty and vertebroplasty (14) have similar safety and effectiveness and clinical improvement with the percutaneous vertebral cement augmentation (SpineJack), this last have shown better restoration of vertebral heights and angles over time (15), confirmed by clinic and radiological images.
In this study, the majority of patients were male (85%), and none of this group had osteoporosis vertebral fracture. Following this point, the majority of studies in literature review as trauma as osteoporosis compression vertebral fracture, being the osteoporotic the most common, and, likewise, its more usual in female (16). However, the result was a significant improvement in pain in the follow-up to 6 months, in both groups (female and male), conversely, the female present a more significant improvement in pain, and this could be due to the etiology of the fracture, in this case osteoporosis.
Conclusions
Spine fracture reduction procedures done through percutaneous way with expander endovertebral implants and intraosseous fixation using SpineJack® intravertebral implants plus Cohesion® cement have proven to be effective, as well as safe under natural circumstances, for pain management and prevention of disability in both men and women. The results on this series of cases are similar to those reported in the world literature.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hu R, Mustard CA, Burns C. Epidemiology of incident spinal fracture in a complete population. Spine (Phila Pa 1976) 1996;21:492-9. [Crossref] [PubMed]
- Fairbank J. Use of Oswestry Disability Index (ODI). Spine (Phila Pa 1976) 1995;20:1535-7. [Crossref] [PubMed]
- Schnake KJ, Schroeder GD, Vaccaro AR, et al. AOSpine Classification Systems (Subaxial, Thoracolumbar). J Orthop Trauma 2017;31 Suppl 4:S14-23. [Crossref] [PubMed]
- Taylor RS, Fritzell P, Taylor RJ. Balloon kyphoplasty in the management of vertebral compression fractures: an updated systematic review and meta-analysis. Eur Spine J 2007;16:1085-100. [Crossref] [PubMed]
- Galibert P, Deramond H, Rosat P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987;33:166-8. [PubMed]
- Sadeghi-Naini M, Aarabi S, Shokraneh F, et al. Vertebroplasty and Kyphoplasty for Metastatic Spinal Lesions: A Systematic Review. Clin Spine Surg 2018;31:203-10. [Crossref] [PubMed]
- Röllinghoff M, Zarghooni K, Schlüter-Brust K, et al. Indications and contraindications for vertebroplasty and kyphoplasty. Arch Orthop Trauma Surg 2010;130:765-74. [Crossref] [PubMed]
- Buchbinder R, Johnston RV, Rischin KJ, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev 2018;4. [PubMed]
- Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 2001;26:1511-5. [Crossref] [PubMed]
- Chang X, Lv YF, Chen B, et al. Vertebroplasty versus kyphoplasty in osteoporotic vertebral compression fracture: a meta-analysis of prospective comparative studies. Int Orthop 2015;39:491-500. [Crossref] [PubMed]
- Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976) 2006;31:1983-2001. [Crossref] [PubMed]
- Fribourg D, Tang C, Sra P, et al. Incidence of subsequent vertebral fracture after kyphoplasty. Spine (Phila Pa 1976) 2004;29:2270-6; discussion 2277. [Crossref] [PubMed]
- Al-Nakshabandi NA. Percutaneous vertebroplasty complications. Ann Saudi Med 2011;31:294-7. [Crossref] [PubMed]
- Dohm M, Black CM, Dacre A, et al. A randomized trial comparing balloon kyphoplasty and vertebroplasty for vertebral compression fractures due to osteoporosis. AJNR Am J Neuroradiol 2014;35:2227-36. [Crossref] [PubMed]
- Noriega DC, Ramajo RH, Lite IS, et al. Safety and clinical performance of kyphoplasty and SpineJack(®) procedures in the treatment of osteoporotic vertebral compression fractures: a pilot, monocentric, investigator-initiated study. Osteoporos Int 2016;27:2047-55. [Crossref] [PubMed]
- Parreira PC, Maher CG, Megale RZ, et al. An overview of clinical guidelines for the management of vertebral compression fracture: a systematic review. Spine J 2017;17:1932-8. [Crossref] [PubMed]