
Surgical management of spinal fractures in ankylosing spondylitis
Introduction
Ankylosing spondylitis (AS) is an inflammatory rheumatologic condition that predominantly affects the axial skeleton (1). It has a prevalence of 0.1% to 1.4% and is twice more common in males than females (2). The widespread inflammation leads to structural changes and formation of syndesmophytes, which fuse vertebral segments (3,4). The resulting spinal immobility of the ankylosed spine, along with the low bone mineral density associated with the disease, renders the spine susceptible to fractures (5,6).
Most reported vertebral fractures in AS patients occur in the subaxial cervical spine and the thoracolumbar spine (7-9). Treatment for vertebral fractures in AS patients has shifted towards surgical intervention with the advent of modern spinal instrumentation. However, surgical intervention can still be controversial in certain cases. Since patients with AS have an increased risk for pulmonary complications and cardiac conduction disturbances (10-12), they present with a higher predisposition to perioperative morbidity and mortality. Non-operative treatment, which includes bed rest, traction, and immobilization/bracing, used to be the standard treatment (13). However, nonoperative management of these vertebral fractures in AS patients can often lead to poor fracture healing, resulting in pseudarthrosis (14). Recent studies report that patients undergoing surgical treatment have better clinical outcomes (7,15).
Spinal fusion approaches for vertebral fractures in AS patients depend on the location of the fracture and can include posterior spinal fusion (PSF), anterior-posterior spinal fusion (APSF), and anterior spinal fusion (ASF). With the advent of new instrumentation and techniques, trends in the use of these approaches have changed. To our knowledge, no study has examined the national trends in the use of spinal fusion surgery for vertebral fractures in AS patients. The objective of this study is to evaluate trends in the surgical treatment of AS patients with cervical and thoracolumbar spine fractures between 2003 and 2014.
Methods
Data source
We queried the NIS database for the years 2003 to 2014. The NIS is the largest publicly available database in the United States. It contains an approximate 20% sample of hospital inpatient admissions. Data for each hospitalization includes diagnoses and procedures, patient demographics, institutional characteristics, lengths of stay, charges, and outcomes (16). In addition to these data, sampling weights are also supplied by the NIS which allows for calculation of national estimates. This study is exempt from institutional review board approval because the NIS database is publicly available.
Patient population
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9) diagnostic and procedure codes were used to identify the patient population of interest. We identified all patients from 2003 to 2014 with a diagnosis of AS (ICD-9 72.00). The records of these patients were then queried for cervical fractures using ICD-9 diagnostic codes 805.00 to 805.08 and 806.00 to 806.09; patients with thoracolumbar fractures were identified using ICD-9 diagnostic codes 805.2, 805.4, 806.2, 806.20 to 806.29, and 80.64. These patients’ records were then queried for cervical, thoracolumbar, and lumbosacral fusion. Patients who underwent PSF were identified using the ICD-9 procedural codes 81.03, 81.05, 81.07, and 81.08; patients who underwent ASF were identified using the ASF codes 81.02, 81.04, and 81.06; and patients who underwent APSF were identified using at least one of each of the PSF and ASF codes.
We identified 961 patients with a diagnosis of AS who received spinal fusion surgeries for cervical or thoracolumbar vertebral fractures during the study period. After utilizing the NIS discharge weights, 4,683 admissions were estimated. The database was then used to query for patient demographics, hospital location (urban/rural), geographic region (Northeast/Midwest/South/West), length of stay, and total hospitalization costs.
Outcome measures
Operative characteristics that were evaluated included surgical approach (PSF, APSF, and ASF). Major in-hospital complications, defined as those requiring a return to the operating room or having potentially long-term sequelae, included: neurological, cervical-spine related, pulmonary, cardiac, thromboembolic, renal, infectious, implant-related, and incidental durotomies. We also evaluated in-patient mortality rates and the use of blood transfusions (ICD-9 99.04).
Statistical methods
The associations between surgical approach and complications, patient sex, patient, race, and hospital characterizations were analyzed using Pearson chi-squared tests. Analysis of variance model was used in the comparison of age, length of stay, and total hospitalization costs between the three surgical approaches. Significance was set at P<0.05. All calculations were performed using Stata 13.1 (StataCorp., College Station, TX, USA).
Results
Population demographics
The patient population’s mean age was 67.4 (SD, 13.5) with all of the patients older than 18 years of age. Females accounted for 12.3% of all patients. Within the patient population, 80.3% were white, 5.2% were black, 7.0% were Hispanic, 3.6% were Asian or Pacific Islander, 1% were Native American, and 3% were unclassified.
Trends in spinal fusion
The number of spinal fusion surgeries performed in AS patients who experienced fractures increased significantly (P<0.01) over the study period (Figure 1).

The proportion of cervical fractures receiving fusions stayed consistent (Figure 2). However, there was a shift in the surgical approaches for cervical fractures. The number of PSF surgeries in cervical fractures increased 4.0-fold and the number of ASF surgeries increased 3.8-fold. While APSF was most popular in 2003 (55.6%), it was least popular in 2014 (21.7%) (Figure 3).
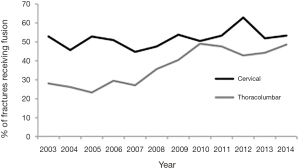
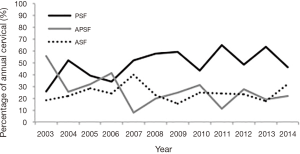
The proportion of thoracolumbar fractures receiving fusions increased significantly (P<0.01) from 2003 to 2014 (Figure 2). Moreover, the percentage of PSF surgeries with thoracolumbar fractures increased significantly (P=0.01), with PSF accounting for 84.6% of the surgeries in 2003 and 95.7% in 2014 (Figure 4).

Institutional characteristics and approach
For the cervical group, there was a significant association between hospital location and approach (P=0.03); 1.8% of PSF, 1.1% of APSF, 7.8% of ASF surgeries were performed in rural hospitals.
In the cervical group, all three approaches were more popular in hospitals located in the South: 41.7% of PSF, 41.2% of APSF, and 46.8% of ASF surgeries. In the thoracolumbar group, most of the PSF (35.8%) and APSF (57.1%) surgeries were performed in the South while most (42.9%) of the ASF surgeries were performed in the Midwest.
Total hospitalization costs, length of stay, and approach
In the cervical group, there was a significant association between surgical approach and total charges (P<0.01): $202,199 for PSF, $245,044 for APSF, and $138,811 for ASF surgery. There was also a significant difference in length of stay by approach (P<0.01): 12.2 days for PSF, 17 days for APSF, and 10.3 days for ASF.
For the thoracolumbar group, there was no significant association between approach and total charges. However, there was a significant difference in length of stay by approach (P<0.01): 11.4 days for PSF, 16.8 days for APSF, and 13.9 days for ASF.
Complications, transfusions, and approach
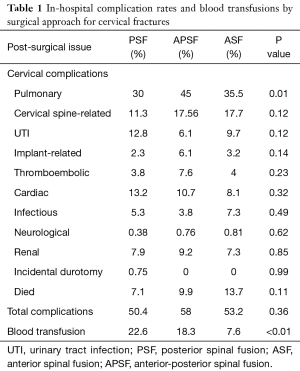
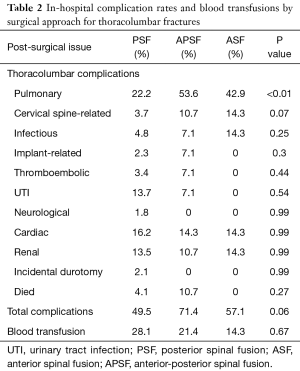
There was a significant association between pulmonary complications (respiratory failure, pneumonia, iatrogenic pneumothorax) and surgical approach in both the cervical (P=0.01) and thoracolumbar (P<0.01) groups (Tables 1,2).
Full table
Full table
Blood transfusions were more common in PSF (22.6%) and APSF (18.3%) than in ASF (7.6%) in the cervical group (P<0.01).
The in-patient mortality rates were higher in patients with cervical fractures (7.1% in PSF, 9.9% in APSF, 13.7% in ASF) than with thoracolumbar fractures (4.1% in PSF, 10.7% in APSF, 0% in ASF); however, there was no statistically significant difference between the surgical approaches (Tables 1,2).
Discussion
While the difference between operative and non-operative management of vertebral fractures in AS patients has been well-studied, differences in surgical approaches within operative treatment have not. In this study, we analyzed national trends in the use of spinal fusion surgery for the surgical treatment of AS from 2003 to 2014. Our results show that operative treatment is being increasingly used for thoracolumbar fractures but staying consistent for cervical fractures.
Several studies have been published on the management of spinal fractures in patients with AS (7,17-19). Spinal fractures in AS patients are associated with higher rates of neurologic damage in contrast to those in patients with non-ankylosed spinal fractures (20-22). Non-operative treatment includes bed rest, roto-rest bed, and immobilization with a brace or halo vest and surgical treatment includes posterior fixation, anterior fixation, or anterior-posterior fixation (7). Though treatment recommendations have been shifting over the years, prior studies (23) and more recent studies (24) agree that if progressive neurologic deficits are observed, surgery is indicated. Minimally invasive techniques in combination with or without decompression are also being increasingly used (25-28).
In AS patients, cervical fractures are observed more frequently than thoracolumbar fractures. In an analysis of published case series, Westerveld et al. note that 77.5% of fractures were located in the subaxial cervical spine (7). In a more recent NIS database study spanning 2005 to 2011, Lukasiewicz et al. (29) reported 53% of fractures to be in the cervical spine, 41.9% in the thoracic spine, 18.2% in the lumbar spine, and 1.5% in the sacrum. Our data is consistent with the latter study with 47.4% of fractures in the cervical spine, 37.5% in the thoracic spine, 13.7% in the lumbar spine, and 1.4% in the sacrum.
Historically, the standard protocol for cervical fractures in AS patients used to be non-operative treatment (13,23). However, treatment with traction and immobilization is fraught with difficulty due to the underlying kyphotic deformity often observed in these patients. It has even been proposed that patients be immobilized in the kyphotic position to avoid harmful extension which could result in the progression of neurologic deficits (30). In a 1981 study, Murray et al. reported a mortality rate of 45% for surgically treated patients and 29% for non-operatively managed patients. Not only did these numbers shift over the years, but also the prevalence of surgical approaches changed. In a 1996 study of 31 patients, Olerud et al. recommended APSF for cervical fractures in AS (9). In a more recent study, Kouyoumdjian et al. proposed that ASF alone is sufficient for cervical spine fractures in AS patients (31). ASF has the added benefit of shorter operating time which can improve intra- and post-operative complications. However, operative treatment for cervical fractures is associated with a high risk of mortality. In a recent retrospective study, Schoenfeld et al. reported that AS patients with cervical spine fractures had a significantly increased risk of mortality compared with age- and sex-matched controls at 3 months and at 1 and 2 years after the fracture (32).
Nonoperative treatment was also the standard approach for treating thoracolumbar fractures in AS (17). However, more recent studies recommend early surgical treatment as it results in more favorable outcomes with lower rates of pseudarthrosis and neurologic deficits (7,14,15). In a recent retrospective study of 28 AS patients being treated for thoracolumbar spine fractures, Lu et al. (33) reported that surgically treated patients provided solid fusion and neurological improvement in contrast to non-operatively treated patients who often presented with pseudarthrosis and progressive neurologic deficits. For thoracolumbar fractures, PSF of at least three levels above and below the fracture are recommended by several authors (15,34). In treating 13 thoracolumbar fractures in AS patients, Sapkas et al. exclusively used PSF and solid fusion was achieved in all of them (22). The authors note that this approach is preferred to reduce the possibility of complications, as these patients already have cardiovascular and pulmonary disorders due to their underlying AS.
Minimally invasive approaches are also being utilized more frequently in the treatment of spinal fractures in AS. Minimally invasive stabilization is an alternative to open reduction given the older age, higher rate of comorbidities, and greater surgical risk of AS patients. In the first case series of ankylosing spinal disorder patients with either AS or diffuse idiopathic skeletal hyperostosis (DISH) being treated with minimally invasive techniques, Krüger et al. (26) reported improved patient outcomes with closed reduction and percutaneous dorsal instrumentation. The authors argue that the benefits of the percutaneous approach, including reduced intraoperative complications and operating times, are very advantageous considering the patient cohort. In a similar case series of 11 ankylosing spinal disorder patients, 9 with AS and 2 with DISH, Nayak et al. (28) employed minimally invasive surgeries to stabilize hyperextension thoracolumbar injuries in a cohort of patients with an average age of 77 and multiple comorbidities. The authors reported no instrumentation failures or nonunions that required revision surgeries. They concluded that percutaneous dorsal instrumentation for these fractures are associated with limited disability and higher health utility according to the patients’ postoperative Oswestry Disability Index and EuroQol-5D scores.
In this study, we have shown a significant increase in the total number of spinal fusions for the treatment of vertebral fractures in AS patients from 2003 to 2014. We have also demonstrated that the percentage of thoracolumbar fractures being treated surgically has increased significantly from 28.3% to 48.4%. The increased popularity of surgical treatment for thoracolumbar fractures is most likely due to improvement in surgical implants and techniques which allow a safer alternative to non-operative treatment options. Posterior long segments with pedicle screw constructs are preferred and provide favorable outcomes (33). This is in agreement with our results, which demonstrate a significant increase (84.6% in 2003 and 95.7% in 2014) in the use of PSF for thoracolumbar fractures (Figure 4). Moreover, newer minimally invasive pedicle screw instrumentation allows higher risk patients to undergo surgery without concerns of large soft tissue dissection.
Fractures in the cervical spine have greater variability with respect to surgical approach. The treatment is also rendered more controversial due to the higher mortality rate associated with these injuries. This is in part due to the presence of preexisting deformities such as kyphosis. Thus, for the cervical spine, the location and presence of deformity need to be carefully considered when choosing a treatment option. Werner et al. (34) recommend that PSF or APSF should be used because ASF is associated with higher failure rates. However, our results indicate that ASF is still relatively popular. While APSF (55.6%) was most frequently used in 2003, PSF (46.7%) and ASF (31.7%) were more popular in 2014. These numbers corroborate the notion that treating the cervical fractures is more individualistic, depending on the location and underlying deformity. In the senior author’s practice, there have been instances in which AS patients with cervical spine fractures were unable to tolerate prone positioning due to cardiac or pulmonary comorbidities. In such cases, an anterior cervical fusion can be performed with concurrent cervical collar and bed rest with bathroom privileges.
With regard to differences among the three surgical approaches, we found significant differences in both the cervical and thoracolumbar groups. There was a significant association between hospital location and approach in the cervical group. There was also a significant association between total charges and length of stay in the cervical group with APSF having higher total costs and hospitalization lengths. In the thoracolumbar group, APSF had significantly higher hospitalization length but not total costs. This finding is in agreement with the intrinsic difference between APSF and the other approaches, in that APSF is a more extensive multi-operation procedure.
A higher prevalence of pulmonary disease is often seen in AS patients due to restrictive ankylosis of the thoracic cage (10,11). Extra-articular involvement of the lungs can be seen even in asymptomatic patients (35). Our complications results confirm this pulmonary component of AS. In addition, we found a significant association between surgical approach and pulmonary complications in both cervical and thoracolumbar fractures in which the highest rate of pulmonary complications is seen in APSF. This is a significant finding that may assist surgeons in choosing a treatment approach for AS patients with spinal fractures who may have preexisting lung disease.
Our study has several limitations inherent to large database studies. First, the quality of the data has an influence on the power of our study. Therefore, incorrect or inconsistent coding of ICD-9 codes are potential sources of error. Moreover, complication data are acquired from inpatient hospitalizations and do not factor in a patient’s long-term complications. Second, the NIS database does not provide specific details about a patient’s hospitalization. This is important because underlying deformities, radiographic data, and time elapsed since fracture onset is instrumental factors to consider when making a treatment decision. We also do not have information on the neurological status of the patient following the fracture. Lastly, minimally invasive instrumentation is increasingly being used to treat fractures in AS, and the database does not have the level of detail to differentiate between open versus minimally invasive instrumentation.
Conclusions
We found that surgical treatment has been growing in popularity for thoracolumbar fractures but staying consistent for cervical fractures in AS patients. Surgical approach has shifted for cervical fractures with APSF transitioning from the most popular to the least popular approach from 2003 to 2014. For thoracolumbar fractures, PSF has remained the preferred approach. Patients undergoing APSF had significantly higher pulmonary complication rates in both cervical and thoracolumbar fractures. This finding can help surgeons in treating fractures in AS patients with underlying pulmonary disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Because the NIS database is publicly available, our study was exempt from institutional review board (IRB) approval.
References
- Braun J, Sieper J. Ankylosing spondylitis. Lancet 2007;369:1379-90. [Crossref] [PubMed]
- Feldtkeller E, Khan M, Van Der Heijde D, et al. Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis. Rheumatol Int 2003;23:61-6. [PubMed]
- Wanders A, Landewe R, Dougados M, et al. Association between radiographic damage of the spine and spinal mobility for individual patients with ankylosing spondylitis: can assessment of spinal mobility be a proxy for radiographic evaluation? Ann Rheum Dis 2005;64:988-94. [Crossref] [PubMed]
- De Vlam K, Mielants H, Veys E. Involvement of the zygapophyseal joint in ankylosing spondylitis: relation to the bridging syndesmophyte. J Rheumatol 1999;26:1738-45. [PubMed]
- Davey-Ranasinghe N, Deodhar A. Osteoporosis and vertebral fractures in ankylosing spondylitis. Curr Opin Rheumatol 2013;25:509-16. [Crossref] [PubMed]
- Karberg K, Zochling J, Sieper J, et al. Bone loss is detected more frequently in patients with ankylosing spondylitis with syndesmophytes. J Rheumatol 2005;32:1290-8. [PubMed]
- Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;18:145-56. [Crossref] [PubMed]
- Thorngren K-G, Liedberg E, Aspelin P. Fractures of the thoracic and lumbar spine in ankylosing spondylitis. Arch Orthop Trauma Surg 1981;98:101-7. [Crossref] [PubMed]
- Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J 1996;5:51-5. [Crossref] [PubMed]
- Kanathur N, Lee-Chiong T. Pulmonary manifestations of ankylosing spondylitis. Clin Chest Med 2010;31:547-54. [Crossref] [PubMed]
- Davies D. Lung fibrosis in ankylosing spondylitis. Thorax 1972;27:262. [Crossref] [PubMed]
- Kaźmierczak J, Peregud-Pogorzelska M, Biernawska J, et al. Cardiac arrhythmias and conduction disturbances in patients with ankylosing spondylitis. Angiology 2007 Dec-2008 Jan;58:751-6. [Crossref] [PubMed]
- Osgood C, Martin LG, Ackerman E. Fracture-dislocation of the cervical spine with ankylosing spondylitis: Report of two cases. J Neurosurg 1973;39:764-9. [Crossref] [PubMed]
- Fox MW, Onofrio BM, Kilgore JE. Neurological complications of ankylosing spondylitis. J Neurosurg 1993;78:871-8. [Crossref] [PubMed]
- Caron T, Bransford R, Nguyen Q, et al. Spine fractures in patients with ankylosing spinal disorders. Spine 2010;35:E458-E64. [Crossref] [PubMed]
- Agency for Healthcare Research and Quality. Introduction to the HCUP National Inpatient Sample (NIS) 2014. Available online: https://hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2014.jsp
- El Tecle NE, Abode-Iyamah KO, Hitchon PW, et al. Management of spinal fractures in patients with ankylosing spondylitis. Clin Neurol Neurosurg 2015;139:177-82. [Crossref] [PubMed]
- Ma J, Wang C, Zhou X, et al. Surgical Therapy of Cervical Spine Fracture in Patients With Ankylosing Spondylitis. Medicine (Baltimore) 2015;94. [PubMed]
- Chaudhary SB, Hullinger H, Vives MJ. Management of acute spinal fractures in ankylosing spondylitis. ISRN Rheumatol 2011;2011. [Crossref] [PubMed]
- Rogers WA. Fractures and dislocations of the cervical spine: an end-result study. J Bone Joint Surg Am 1957;39-A:341-76. [Crossref] [PubMed]
- Janda W, Kelly P, Rhoton Jr A, et al., editors. Fracture-dislocation of the cervical part of the spinal column in patients with ankylosing spondylitis. Mayo Clinic Proceedings, 1968.
- Sapkas G, Kateros K, Papadakis SA, et al. Surgical outcome after spinal fractures in patients with ankylosing spondylitis. BMC Musculoskelet Disord 2009;10:96. [Crossref] [PubMed]
- Murray GC, Persellin RH. Cervical fracture complicating ankylosing spondylitis: a report of eight cases and review of the literature. Am J Med 1981;70:1033-41. [Crossref] [PubMed]
- Kanter AS, Wang MY, Mummaneni PV. A treatment algorithm for the management of cervical spine fractures and deformity in patients with ankylosing spondylitis. Neurosurg Focus 2008;24. [Crossref] [PubMed]
- Sedney CL, Daffner SD, Obafemi-Afolabi A, et al. A Comparison of Open and Percutaneous Techniques in the Operative Fixation of Spinal Fractures Associated with Ankylosing Spinal Disorders. Int J Spine Surg 2016;10:23. [Crossref] [PubMed]
- Krüger A, Frink M, Oberkircher L, et al. Percutaneous dorsal instrumentation for thoracolumbar extension-distraction fractures in patients with ankylosing spinal disorders: a case series. Spine J 2014;14:2897-904. [Crossref] [PubMed]
- Yeoh D, Moffatt T, Karmani S. Good outcomes of percutaneous fixation of spinal fractures in ankylosing spinal disorders. Injury 2014;45:1534-8. [Crossref] [PubMed]
- Nayak NR, Pisapia JM, Abdullah KG, et al. Minimally invasive surgery for traumatic fractures in ankylosing spinal diseases. Global Spine J 2015;5:266-73. [Crossref] [PubMed]
- Lukasiewicz AM, Bohl DD, Varthi AG, et al. Spinal fracture in patients with ankylosing spondylitis: cohort definition, distribution of injuries, and hospital outcomes. Spine 2016;41:191-6. [Crossref] [PubMed]
- Broom MJ, Raycroft JF. Complications of fractures of the cervical spine in ankylosing spondylitis. Spine 1988;13:763-6. [Crossref] [PubMed]
- Kouyoumdjian P, Guerin P, Schaelderle C, et al. Fracture of the lower cervical spine in patients with ankylosing spondylitis: retrospective study of 19 cases. Orthop Traumatol Surg Res 2012;98:543-51. [Crossref] [PubMed]
- Schoenfeld AJ, Harris MB, McGuire KJ, et al. Mortality in elderly patients with hyperostotic disease of the cervical spine after fracture: an age-and sex-matched study. Spine J 2011;11:257-64. [Crossref] [PubMed]
- Lu ML, Tsai TT, Lai PL, et al. A retrospective study of treating thoracolumbar spine fractures in ankylosing spondylitis. Eur J Orthop Surg Traumatol 2014;24 Suppl 1:S117-23. [Crossref] [PubMed]
- Werner BC, Samartzis D, Shen FH. Spinal Fractures in Patients With Ankylosing Spondylitis: Etiology, Diagnosis, and Management. J Am Acad Orthop Surg 2016;24:241-9. [Crossref] [PubMed]
- Yuksekkaya R, Almus F, Celıkyay F, et al. Pulmonary involvement in ankylosing spondylitis assessed by multidetector computed tomography. Pol J Radiol 2014;79:156. [Crossref] [PubMed]


