
Chronic obstructive pulmonary disease is an independent predictor for 30-day readmissions following 1- to 2-level posterior lumbar fusions
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality worldwide with an annual global mortality rate estimated to be around 3 million deaths (1). COPD is expected to become the third most common cause of death worldwide by 2020 (2). As with most chronic diseases, COPD is known to be a significant economic burden on the society (3). In the United States, an estimated $50 billion in direct and indirect healthcare costs were attributed to COPD in 2010 alone (4).
Multiple factors, including tobacco use (5) and exposure to harmful gases (6) secondary to industrialization are responsible for an increase in the prevalence of COPD over time. With increasing longevity and higher prevalence of COPD, the odds of patients undergoing elective surgery requiring management of COPD as a co-morbid diagnosis is expected to rise. Furthermore, this risk is likely to affect elderly patients requiring lumbar fusion for degenerative spine disease (7). Although, few studies have identified COPD as a surgical risk factor, no study has comprehensively investigated the impact of COPD on post-operative outcomes following elective posterior lumbar fusions (PLF).
Using a multi-center, national surgical database we sought to investigate whether COPD was associated with a higher risk of 30-day complications, readmissions and re-operations after 1–2 level PLF.
Methods
Database
This was a retrospective study done using the 2015–2016 American College of Surgeons (ACS)-National Surgical Quality Improvement Program (NSQIP) database. The ACS-NSQIP database collects surgical information from more than 500 hospitals across the United States. Data are recorded for more than 150 preoperative, intra-operative and postoperative variables up to 30 days following the operation. The data are collated by trained surgical and clinical reviewers with audit reports showing an inter-reviewer disagreement rate of below 2% (8). Since the ACS-NSQIP database is a de-identified public database available to participating hospitals, it is exempt from the Institutional Review Board approval.
Study population
Current procedural terminology (CPT) codes for PLF (CPT-22612, CPT-22630 and CPT-22633) were used to retrieve records from the database. Two-level PLFs were queried using CPT codes (22614, 22632 and 22634) to identify each additional level. Only elective 1- to 2-level PLFs being done for degenerative pathologies of the spine were included in the study. Patients undergoing a >2 level fusion, fracture fixation, fusion for malignancy and deformities were excluded. In addition, patients undergoing a concurrent anterior lumbar fusion and/or a combined anterior-PLF were also removed from the study cohort. Data were filtered to remove for missing variables to reduce possibility of confounding in our analysis.
Definition of variables studied
The following baseline demographics and clinical patient variables were collected—age (categorized as 0–50, 51–65, 66–75 and >75 years of age), race (White, Black or African-American, American Indian or Alaska Native, Native Hawaiian or Pacific Islander, Asian and unknown/not reported), gender, body mass index (BMI), comorbidities, type of anesthesia used (general vs. other), admission status (inpatient vs. outpatient), American Society of Anesthesiologists (ASA) class, quarter of admission (January–March, April–June, July–September and October–December), number of levels fused (1-level vs. 2-level), use of posterior instrumentation, total operative time (minutes) and length of stay (≤3 vs. >3 days).
The ACS-NSQIP defines the presence of COPD based on review of medical records as well as the fulfillment of the following criteria: (I) functional disability due to COPD; (II) use of chronic bronchodilator therapy; (III) prior history of exacerbation requiring hospitalization; or (IV) pulmonary function test (PFT) showing a forced expiratory volume in one second (FEV1) less than 75% of the expected.
Our study population of patients undergoing 1- to 2-level PLF was divided into cohorts. The first cohort included patients with a history of COPD, and the second cohort included patients without a history of COPD. Thirty-day complications as defined by ACS-NSQIP were recorded. They included surgical site infection (SSI) whether superficial, deep and organ/space infections; wound dehiscence; myocardial infarction (MI); cardiac arrest; deep venous thrombosis (DVT); pneumonia; pulmonary embolism; urinary tract infection; postoperative ventilator use >48 hours; unplanned reintubation; bleeding requiring transfusion; acute renal failure; cerebrovascular/stroke; sepsis; septic shock; 30-day mortality; 30-day readmissions; and 30-day unplanned reoperations.
Statistical analysis
Univariate comparison of demographic, pre-operative, operative and post-operative (30-day complication) variables between patients with and without COPD was done using the Pearson-Chi square test. All post-operative variables (30-day complications) with a P value<0.05 from univariate analysis were entered into separate backward elimination logistic regression models, while adjusting for all significant (P<0.05) demographic, pre-operative and operative variables, to analyze the impact of COPD on post-operative outcomes alone while controlling for the differences present between the two groups. The impact of COPD on post-operative outcomes following adjusted analysis have been presented as odds ratio (OR) and 95% confidence interval (CI) and a P value of less than 0.05 was considered statistically significant. Statistical Analysis was carried out using SPSSv23 (IBM, Armonk, NY, USA).
Results
A total of 23,481 patients were included in the study after applying the appropriate inclusion and exclusion criteria. Out of these patients, 1,123 (4.8%) patients had a prior diagnosis of COPD at the time of the surgery. Baseline clinical characteristics are shown in Table 1. Univariate analysis showed that the groups were significantly different in terms of age, race, BMI, comorbidities, transfer status and ASA Class. Patients with COPD were generally older and had concurrent multiple co-morbidities.
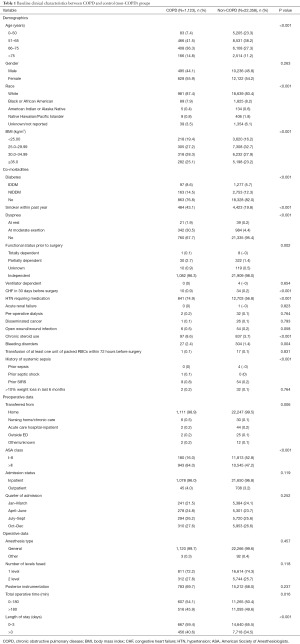
Full table
Unadjusted analysis showed that postoperatively, patients with COPD were significantly associated with a longer length of stay >3 days (P<0.001), a shorter total operative time (min) (P=0.016), risk for MI (P=0.040), cardiac arrest (P=0.041), pneumonia (P<0.001), postoperative mechanical ventilation for more than 48 hours (P=0.004), unplanned reintubation (P=0.001), 30-day readmissions (P<0.001) and discharge to skilled-care or rehabilitation facility (P<0.001) (Table 2). No significant association was seen between presence of COPD and 30-day re-operation (P=0.179) and mortality (P=0.922).
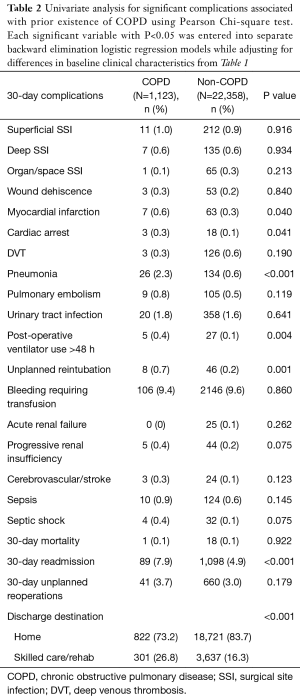
Full table
On adjusted analysis, a history of COPD was significantly associated with hospital stay longer than 3-days (OR, 1.40; 95% CI: 1.32–1.48; P=0.008), shorter operative time (OR, 0.83; 95% CI: 0.73–0.94; P=0.003), discharge to skilled-care or rehabilitation facility) (OR, 1.28; 95% CI: 1.09–1.51); P=0.002), pneumonia (OR, 2.53; 95% CI: 1.62–3.97; P<0.001) and 30-day readmission (OR, 1.31; 95% CI: 1.03–1.65; P=0.025) (Table 3).
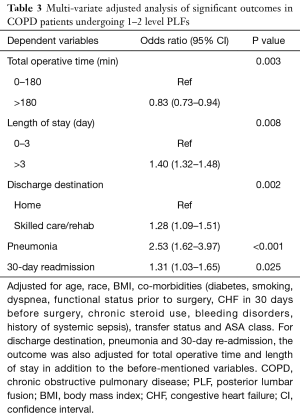
Full table
Discussion
Our analysis found that COPD is an independent risk factor associated with longer length of hospital stay, discharge to skilled-care or rehabilitation facility, post-operative pneumonia within 30 days, and 30-day readmission. Patients undergoing lumbar fusion are likely to have concomitant COPD for which a multi-disciplinary approach involving hospitalists, surgeons and critical care specialists will be required to optimize patients before surgery.
Recently there has been a shift toward value-based health-care aimed at improving quality of care while minimizing costs. Considering that each extra day in the hospital is estimated to cost around $1,000 (9), efforts to decrease length of stay following lumbar fusion will be beneficial towards increasing cost-effectiveness (10). Therefore, there is a need to prospectively identify factors that contribute to increased length of stay so that appropriate post-operative care pathways can be tailored for an early discharge. The current study’s findings of COPD contributing to an increased length of stay are in contradiction to previous spine literature. Basques et al. utilized the NSQIP database and concluded that presence of pulmonary co-morbidity was not associated with extended length of stay in elective PLFs (11). Similarly, Gruskay et al., using a cohort of 103 cases of elective PLFs, concluded that the presence of pulmonary co-morbidities did not negatively impact the length of stay (9). A possible reason for the findings in both studies could be that the authors combined numerous pulmonary co-morbidities such as pulmonary embolism, chronic bronchitis, COPD, pre-operative ventilator use or current pneumonia into one variable “pulmonary co-morbidity”. Both studies had relatively smaller sample sizes, which may impact the power of the studies. Using a large sample size, our study effectively manages to captures the impact of COPD alone on the post-operative outcomes without compromising the power.
Interestingly, we noted that COPD patients had a shorter operative time as compared to the non-COPD group. A similar finding has been reported in a previous study investigating the impact of COPD on postoperative outcomes in total hip arthroplasty (THA) (12). A plausible reason given by the authors in that study was that surgical and anesthesia teams would attempt to finish cases faster in order to prevent the occurrence of postoperative complications in patients with an already higher baseline co-morbidity burden.
Airway inflammation, narrowing and/or obliteration in COPD results in the intrinsic and extrinsic respiratory muscles being overworked to compensate for the low amount of oxygen entering the alveoli (13). Therefore, these patients might require prolonged postoperative mechanical ventilation to maintain adequate oxygen saturation levels (14). Moreover, the small airway disease can lead to trapping of bacteria and form a nidus of infection in the lung predisposing patients to developing pneumonia (15). Implementation of post-operative pneumonia prevention protocols may be an effective way of reducing the incidence of this complication. A 2010 study showed that implantation of a pneumonia-prevention program, comprising of staff education, chlorhexidine oral hygiene, incentive spirometry, ambulation and head-of-bed elevation, resulted in an 81% decrease in the incidence of post-operative pneumonia (16). Furthermore, considering that re-admissions are now an important determinant of hospital quality metrics (17), the findings of the current study stress the need for medical optimization in high-risk COPD patients to minimize the occurrence of complications and re-admissions, and improve the overall quality of care.
We found that COPD was associated with higher odds of discharge to a skilled-care or rehabilitation facility. Although this is expected given the supervision of medical care required in these high-risk patients, it may be a cause of concern given that recent literature has shown a higher rate of complications following discharge to these facilities (18).
There are several important limitations to the current study. First, the NSQIP database only captures complications occurring up to 30 days following the index procedure. It is plausible that there may be COPD-associated complications occurring beyond the specified time period. Second, as with any database study we were unable to study disease severity, radiographic findings, and patient reported outcomes. Third, we were unable to measure healthcare costs, such as costs accrued from an increased length of stay, from this database. Finally, the ACS-NSQIP database largely consists of academic medical centers and may not be representative of a true national population. Despite the limitations posed by the database, the current study utilizes a large cohort and effectively highlights the increased risk of adverse outcomes in patients with COPD undergoing PLF.
Conclusions
Following adjustment for differences in baseline clinical characteristics, COPD is independently associated with a risk of prolonged length of hospital stay, discharge to skilled-care or inpatient rehabilitation, post-operative pneumonia and readmission within 30 days after 1- and 2-level PLF. This data from a large cohort of patients may be used for pre-operative counselling to convey the risk of complications and readmissions in patients with COPD after PLF. Specific focus on optimization of patients with COPD will be beneficial in reducing the risk of postoperative complications and readmission with the aim of improving quality of care.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Since the ACS-NSQIP database is a de-identified public database available to participating hospitals, it is exempt from the Institutional Review Board approval.
References
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Crossref] [PubMed]
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997;349:1498-504. [Crossref] [PubMed]
- Guarascio AJ, Ray SM, Finch CK, et al. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res 2013;5:235-45. [PubMed]
- American Lung Association - How serious is COPD? 2011 (cited 2018 12 March). Available online: http://www.lung.org/lung-disease/copd/resources/facts-figures/COPD-Fact-Sheet.html
- Mannino DM, Higuchi K, Yu TC, et al. Economic Burden of COPD in the Presence of Comorbidities. Chest 2015;148:138-50. [Crossref] [PubMed]
- Boschetto P, Quintavalle S, Miotto D, et al. Chronic obstructive pulmonary disease (COPD) and occupational exposures. J Occup Med Toxicol 2006;1:11. [Crossref] [PubMed]
- Yoshihara H, Yoneoka D. National trends in the surgical treatment for lumbar degenerative disc disease: United States, 2000 to 2009. Spine J 2015;15:265-71. [Crossref] [PubMed]
- Iwamoto T, Suzuki T, Matsumura N, et al. Lateral Para-Olecranon Approach for the Treatment of Distal Humeral Fracture. J Hand Surg Am 2017;42:344-50. [Crossref] [PubMed]
- Gruskay JA, Fu M, Bohl DD, et al. Factors affecting length of stay after elective posterior lumbar spine surgery: a multivariate analysis. Spine J 2015;15:1188-95. [Crossref] [PubMed]
- Shields LB, Clark L, Glassman SD, et al. Decreasing hospital length of stay following lumbar fusion utilizing multidisciplinary committee meetings involving surgeons and other caretakers. Surg Neurol Int 2017;8:5. [Crossref] [PubMed]
- Basques BA, Fu MC, Buerba RA, et al. Using the ACS-NSQIP to identify factors affecting hospital length of stay after elective posterior lumbar fusion. Spine (Phila Pa 1976) 2014;39:497-502. [Crossref] [PubMed]
- Yakubek GA, Curtis GL, Sodhi N, et al. Chronic Obstructive Pulmonary Disease Is Associated With Short-Term Complications Following Total Hip Arthroplasty. J Arthroplasty 2018;33:1926-9. [Crossref] [PubMed]
- Klimathianaki M, Vaporidi K, Georgopoulos D. Respiratory muscle dysfunction in COPD: from muscles to cell. Curr Drug Targets 2011;12:478-88. [Crossref] [PubMed]
- Singh D. Small Airway Disease in Patients with Chronic Obstructive Pulmonary Disease. Tuberc Respir Dis (Seoul) 2017;80:317-24. [Crossref] [PubMed]
- Sethi S, Murphy TF. Bacterial infection in chronic obstructive pulmonary disease in 2000: a state-of-the-art review. Clin Microbiol Rev 2001;14:336-63. [Crossref] [PubMed]
- Wren SM, Martin M, Yoon JK, et al. Postoperative pneumonia-prevention program for the inpatient surgical ward. J Am Coll Surg 2010;210:491-5. [Crossref] [PubMed]
- Fischer C, Lingsma HF, Marang-van de Mheen PJ, et al. Is the readmission rate a valid quality indicator? A review of the evidence. PLoS One 2014;9. [Crossref] [PubMed]
- McLawhorn AS, Fu MC, Schairer WW, et al. Continued Inpatient Care After Primary Total Knee Arthroplasty Increases 30-Day Post-Discharge Complications: A Propensity Score-Adjusted Analysis. J Arthroplasty 2017;32:S113-8. [Crossref] [PubMed]


