
The Morel-Lavallée lesion in thoracolumbar spine trauma—two index cases
Introduction
The Morel-Lavallée lesion (MLL) is a closed degloving injury caused by traumatic separation of the subcutaneous tissue from the underlying fascia, without a break in the overlying skin. It was initially reported in 1853 by the French surgeon Victor-Auguste-François Morel-Lavallée (1,2). It is most commonly associated with pelvic injuries. We have reviewed the literature on lumbar MLLs and present a previously unreported association of thoracolumbar fractures and MLL.
Case presentation
Case 1
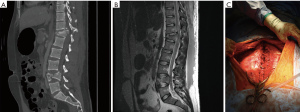
A 21-year-old male rear seat passenger was ejected from the car in a high-speed motor vehicle accident. He was transferred from a rural hospital to our Level 1 trauma centre. A trauma CT scan demonstrated the following injuries: undisplaced C2 arch fracture; T12 AO type C injury; L4 AO type A4 injury; transverse process fractures of T10, T11, L1 and L3; multiple bilateral rib fractures; grade 2 splenic injury; left-sided retroperitoneal haematoma; right distal radius fracture; right scapula fracture; and a lumbar MLL (Figure 1). The patient had an ASIA A spinal cord injury. A posterior T12 vertebrectomy with cage reconstruction and a T10–L5 pedicle screw fixation was undertaken.
A week later the patient developed discharge from his wound and he was taken to theatre for washout, debridement and application of a negative pressure wound therapy device (NPWT). He underwent three further washouts and NPWT changes, followed by closure with a split skin graft. Enterobacter cloacae was grown, requiring 4 weeks of meropenem treatment, followed by 6 months of oral ciprofloxacin.
Case 2
A 21-year-old male was found by bystanders in a rural area after a car versus tree motor vehicle accident. He was transferred to our Level 1 trauma centre after stabilisation. A trauma CT scan and an MRI spine revealed the following images: multiple rib fractures, pulmonary contusion, right kidney laceration, an L1 AO type B2 injury, L2 spinous process fracture, bilateral acetabular fractures, right inferior pubic ramus fracture, right sacroiliac diastasis, and a lumbar MLL (Figure 2). The MLL was not noted on the trauma CT scan.
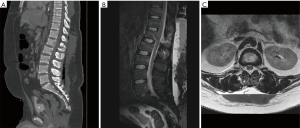
The patient proceeded to theatre the following day for a T11 to L3 pedicle screw fixation and fusion. It was noted that there were abrasions over the lumbar region, and after a midline incision a large cavity of blood was encountered between the muscle and fascial layers. Two drains were placed. The patient underwent percutaneous fixation of the right sacroiliac joint on the same day. Intravenous (IV) antibiotics were given whilst drains remained in. They were removed on post-operative day 3.
Signs of wound infection developed 2 days later and IV antibiotics were recommenced. The wound dehisced on day 7 post-op and the patient was taken back to theatre where a large infected haemoserous collection was encountered. A NPWT dressing was applied and the patient underwent regular washouts and NPWT changes over the following 2 months. Enterobacter cloacae was grown from the MLL requiring IV meropenem. Debridement and closure was undertaken 2 months from admission. On follow-up at 3 months there were no signs of infection with good wound closure.
Discussion
The MLL is a closed degloving injury caused by traumatic separation of the subcutaneous tissue from the underlying fascia, without a break in the overlying skin. In his initial paper, Morel-Lavallée described 12 cases of “traumatic serous effusions”, of which 10 involved pelvic or extremity trauma (1). He published a second review of the topic a decade later in which he revised his description of the lesion to a traumatic separation of the layers below the skin, with the serous effusion a secondary phenomenon (3). He provided 30 further cases in this paper, and postulated an “oblique or tangential pressure” as the proposed mechanism, which would cause the hypodermis to separate from the underlying fascia (3). This shear force disrupts vasculature and lymphatics which fills this potential space with lymph, blood and necrotic fat (4,5).
The MLL is most commonly seen in the trochanteric region; and has been associated with pelvic trauma, including spinopelvic dissociation (6,7). The initial case series by Morel-Lavallée included two cases of lumbar MLL after blunt trauma without fracture. There have since been a small number of cases of MLL in the lumbar region after blunt trauma in the literature (4,6,8,9). Similarly, none of these have been associated with lumbar fractures. We present a previously unreported association of the MLL with thoracolumbar spinal fractures.
The MLL occurs more frequently than is reported. Further, it is often missed on imaging as its significance may not be apparent, or it may be overlooked in the context of multitrauma (5,6,10,11). It may also be difficult to identify the lesion if there are no visible signs of injury. Suzuki and colleagues (12) reviewed 19 patients with vertically unstable sacral fractures treated with operative fixation where clinical evidence of an MLL was an exclusion criterion; five patients were found to have an MLL intra-operatively. In both of our cases, the MLL was overlooked on the initial trauma CT scan. We think it is important to consider the possibility of an MLL in cases of spinal trauma where the imaging focus may be on the spinal cord and vertebral column.
If not identified or treated appropriately MLLs may become infected, cause tissue necrosis, or develop a pseudocapsule (4,6). Various treatment options have been described including conservative management, percutaneous drainage, or incision and debridement. The MLL has a significant risk of infection. Dodwad and colleagues reported infection in three of their four cases (6). In the Suzuki series of 19 patients there were two wound infections, both in patients with MLL; the authors concluded that posterior plate fixation should be used with great caution in these patients due to concerns over infection (12). In a review of the literature, Shen and colleagues reported an infection rate of 19% (29 of 153 cases) (13). The high risk of infection has prompted recommendations for early diagnosis and management of MLLs (4-7,10). Both of our cases developed infected collections with resistant gram-negative bacteria. This resulted in prolonged admission with multiple operations. Lumbar MLL may be at higher risk of infection due to the large area of tissue damage and the location of the lesion.
Unlike cases of pelvic injury in which open surgical correction may be delayed or avoided by the use of percutaneous pelvic fixation, lumbar fractures often require more urgent decompression and fixation. Preoperative recognition of this unique injury is essential so that strategies to mitigate the risk of wound dehiscence and infection can be employed. We are of the opinion that such strategies should include debridement and washout; prolonged drainage with consideration of negative pressure wound therapy; appropriate antibiotic use; meticulous wound care; and early involvement of plastic surgery services.
Conclusions
We report a previously unrecognised association of the MLL with thoracolumbar spine fractures in two cases. Awareness of this injury should allow tailored strategies to decrease the high risk of wound complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Morel-Lavallée VAF. Épanchements traumatiques de sérosité. Arch Gén de Méd 1853.
- Hirsch A. Biographisches lexikon der hervorragenden aerzte aller zeiten und völker. Vienna and Leipzig: Urban and Schwarzenberg, 1886.
- Morel-Lavallée VAF. Décollements traumatiques de a peau et des couches sous-jacentes. Arch Gén de Méd 1863;1.
- Sawkar AA, Swischuk LE, Jadhav SP. Morel-Lavallee seroma: a review of two cases in the lumbar region in the adolescent. Emerg Radiol 2011;18:495-8. [Crossref] [PubMed]
- Dawre S, Lamba S, Sreekar H, et al. The Morel-Lavallee lesion: a review and a proposed algorithmic approach. Eur J Plast Surg 2012;35:489-94. [Crossref]
- Dodwad SN, Niedermeier SR, Yu E, et al. The Morel-Lavallée lesion revisited: management in spinopelvic dissociation. Spine J 2015;15:e45-51. [Crossref] [PubMed]
- Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallée lesion. J Trauma 1997;42:1046-51. [Crossref] [PubMed]
- Efrimescu CI, McAndrew J, Bitzidis A. Acute lumbar Morel-Lavallee haematoma in a 14-year-old boy. Emerg Med J 2012;29:433. [Crossref] [PubMed]
- Moran DE, Napier NA, Kavanagh EC. Lumbar Morel-Lavallée effusion. Spine J 2012;12:1165-6. [Crossref] [PubMed]
- Takahara S, Oe K, Fujita H, et al. Missed massive morel-lavallee lesion. Case Rep Orthop 2014;2014. [Crossref] [PubMed]
- Kottmeier SA, Wilson SC, Born CT, et al. Surgical management of soft tissue lesions associated with pelvic ring injury. Clin Orthop Relat Res 1996.46-53. [Crossref] [PubMed]
- Suzuki T, Hak DJ, Ziran BH, et al. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury 2009;40:405-9. [Crossref] [PubMed]
- Shen C, Peng JP, Chen XD. Efficacy of treatment in peri-pelvic Morel-Lavallee lesion: a systematic review of the literature. Arch Orthop Trauma Surg 2013;133:635-40. [Crossref] [PubMed]


