
The use of subfascial drains after multi-level anterior cervical discectomy and fusion: does the data support its use?
Introduction
Subfascial drains are routinely used after multi-level anterior cervical discectomy and fusion (ACDF) procedures. The use of these kinds of drains following multi-level ACDFs is motivated by a desire to reduce postoperative complications such as surgical site infections (SSIs) and the development of life-threatening hematomas that may cause airway obstruction, despite the lack of evidence to support its use. In lumbar decompression, other studies have reported no association between SSIs and hematoma formation with placement of a subfascial drain; in fact, several studies have found associations between the use of drains and an increased need for postoperative blood transfusion, postoperative fever, and SSI following instrumented fusion (1-10). There is also evidence from several studies concerning surgeries of the neck, esophagectomy, thyroidectomy, parathyroidectomy, demonstrating an increased incidence of SSI and prolonged length of hospital stay with the use of subfascial drains (11-14).
To this end, this study aims to determine whether the use of subfascial drains after multi-level ACDFs are associated with a decreased incidence of hematoma formation and SSIs.
Methods
This is a retrospective study of 321 consecutive adult patients (18 years and older) with degenerative cervical stenosis that underwent an index multi-level ACDF procedure. Institutional review board approval was obtained before study initiation. Only patients that underwent multilevel ACDF’s were included in the study. Patients were separated into one of two groups depending on whether a subfascial drain was placed during surgery (Drain cohort: n=58; No Drain cohort: n=263). The decision to place a drain was based on surgeon preference. Baseline characteristics, operative and postoperative details, as well as rates of hematoma formation and SSI’s were gathered by direct medical record review.
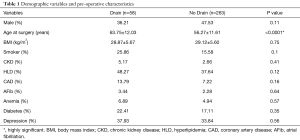
Demographic variables evaluated included patient’ age, sex, and body mass index (BMI). Comorbidities included diabetes, coronary artery disease (CAD), hyperlipidemia (HLD), atrial fibrillation (A-Fib), anemia, depression, chronic kidney disease (CKD), and smoking status.
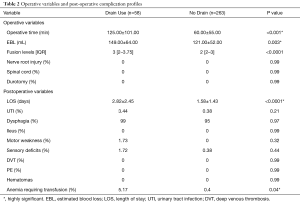
Operative variables included operative time, estimated blood loss (EBL), median number of fusion levels [interquartile range (IQR)], nerve root injury, spinal cord injury, and incidental durotomy. Postoperative variables included length of stay (LOS), incidence of urinary tract infection (UTI), dysphagia, ileus, motor weakness, sensory deficits, deep vein thrombosis, pulmonary embolism, and anemia requiring transfusion.
Parametric data were expressed as means ± standard deviation (SD) and compared via the Student t-test. Nonparametric data were expressed as median (IQR) and compared via the Mann-Whitney U test. Nominal data were compared with the χ2 test. All tests were two-sided and were statistically significant if the P value was <0.05. Statistical analysis was performed using JMP®, Version 12. SAS Institute Inc., Cary, NC, USA, 1989–2007.
Results
Three hundred and twenty-one patients (146 male and 175 female) were studied. The average age at the time of surgery ranged from 20 to 88 years (mean 57.63±12.02 years, median 58 years). Fifty-eight (18%) patients had subfascial drains placed at the time of surgery, and 263 (82%) did not have a subfascial drain placed at the time of surgery. On average, patients with subfascial drains placed at the time of surgery were older (“Drain Cohort”: 63.75±12.03 years vs. “No Drain Cohort”: 56.27±11.61 years, P<0.0001). There were no significant differences between cohorts in baseline demographic or other comorbidity characteristics including male gender (drain: 36.21% vs. no drain: 47.53%, P=0.11), BMI (drain: 28.87±5.67 kg/m2vs. no drain: 29.12±5.60 kg/m2, P=0.75), smoking status (drain: 25.86% vs. no drain:15.58%, P=0.1), CKD (drain: 5.17% vs. no drain: 2.66%, P=0.41), HLD (drain: 48.27% vs. no drain: 37.64%, P=0.12), CAD (drain: 13.79% vs. no drain: 7.22%, P=0.16), A-Fib (drain: 3.44% vs. no drain: 2.28%, P=0.64), anemia (drain: 6.89% vs. no drain: 4.94%, P=0.57), diabetes (drain: 22.41% vs. no drain: 17.11%, P=0.35), and depression (drain: 37.93% vs. no drain: 33.84%, P=0.56) (Table 1).
Full table
Operative variables
The median (IQR) number of fusion levels were higher for patients in which drains were placed compared to those who did not have a drain placed at the time of surgery {“Drain Cohort”: 3 [2–3.75] vs. “No Drain Cohort” 2 [2–3], P<0.0001}. Patients with subfascial drains placed at the time of surgery underwent longer surgeries (125.00±101.00 minutes) as compared to the patients who did not have drains placed at the time of surgery (121.00±52.00 minutes). On average the EBL was higher in the cohort of patients with drains placed at the time of surgery, 149.00±64.00 vs. 121.00±52.00 mL respectively (P=0.003), than those who did not have drains placed at the time of surgery. No patients from either group had an incidental durotomy, or experienced nerve root or spinal cord injury.
Postoperative variables
No patients developed a postoperative hematoma or SSIs (P=0.99). The need for post-operative allogenic blood transfusions were 14-fold higher in the cohort of patients with subfascial drains (“Drain Use”: 5.17% vs. “No drain”: 0.4%, P=0.04) (Table 2). The use of drains postoperatively was independently predictive of the likelihood that a patient would require an allogenic blood transfusion (OR =14.17, P=0.04). Age, BMI, number of levels, smoking status, preoperative anemia, or diabetes mellitus were not found to be independently predictive of a patient requiring post-operative allogenic blood transfusion (Table 3). Compared to patients with no drains, patients with subfascial drains placed at the time of surgery had a significantly longer length of hospital stay 2.82±2.45 vs. 1.58±1.43 days, respectively (P<0.0001).
Full table

Full table
Discussion
In this retrospective study of patients undergoing multi-level ACDFs with and without the use of subfascial drains, we observed no difference in the incidence of SSIs or hematoma formation. Furthermore, patients with subfascial drains were more likely to require a post-operative blood transfusion and have a longer duration of in-hospital stay.
Subfascial drains are routinely used after multi-level ACDFs. The use of these kinds of drains following multi-level ACDFs are motivated by a desire to reduce postoperative complications such as SSI’s and the development of life-threatening hematomas in the neck that may cause airway obstruction, both of which are associated with significant morbidity, health care utilization and costs. However, drain placement is not a trivial consideration, as drains can be associated with pain in the area of insertion, increased patient anxiety during its withdrawal, and the potential for hematoma development during removal. In rare instances, patients may develop a SSI at the drain insertion site. To date, few studies have demonstrated a clinical utility to using these drains, most of which have been very small case series.
The utility of subfascial drains in reducing postoperative hematoma volume has been supported by studies which have found statistically significant benefits in the use of drains following spine surgery (9,10). In a prospective randomized control trial that employed MRI to measure postoperative hematoma volume by Mirzai et al., a significant reduction in the incidence of symptomatic and asymptomatic postoperative hematoma formation was found in patients with subfascial drains as compared to those without drains (10). Furthermore, a retrospective study of patients undergoing elective ACDFs by Basques et al. identified advancing age (≥50 years), increasing number of levels, and a history of smoking as independent predictors of increased drain output, suggesting that patients with these factors may benefit most from surgical drain placement after ACDF (9). In the present study, no patients in either cohort developed a postoperative hematoma or SSIs (P=0.99).
The effectiveness of subfascial drains in the reduction of postoperative SSIs and hematoma formation has been called into question for a wide array of surgical procedures (10-23). In the context of spine surgery, studies including a prospective randomized study by Brown et al. which studied the utility of subfascial drains in 83 patients (42 patients with drains, and 41 patients without drains) following extensive lumbar spine surgeries, found no difference in the incidence of postoperative SSIs or hematoma formation between patients with and without subfascial drains placed at the time of surgery (3). Similarly, another prospective randomized study Payne et al. comparing 103 drained and 97 undrained patients following a single-level lumbar laminectomy found no statically significant difference between the incidence of SSIs or hematoma formation in patients with and without subfascial drains placed at the time of surgery (4). A retrospective analysis by Kanayama et al. that compared 298 drained and 262 undrained patients following single-level lumbar decompression surgeries also found that the risk of SSIs and hematomas was not influenced by the use of a drain (1). Walid et al.’s case-control study compared 285 drained and 117 undrained patients following posterior lumbar interbody fusion, finding no significant reduction in incidence of postoperative SSI or hematoma formation when utilizing drains postoperatively (8). Lastly, a multicenter retrospective study by Diab et al. compared 324 drained and 176 undrained adolescent patients found no difference in the rate of postoperative SSIs between patients with and without subfascial drains placed at the time of surgery (7). Analogously, other surgeries involving the neck failed to demonstrate any recovery benefit or reduction of postoperative SSI or hematoma risk in patients with subfascial drains, and rather found an increased incidence of SSI and prolonged hospital stay in patients with these kinds of drains (11-14). Although our study did not find an increase in SSI with the utilization of subfascial drains, there was no advantage found in the utilization of these kinds of drains in patients undergoing multi-level ACDFs. In fact, no patients experienced an SSI or hematoma in our study in either group.
The use of subfascial drains has also been associated with an increase in length of hospital stay and the need for transfusion in patients undergoing fusion procedures. In a retrospective cohort study, Walid et al. found the rate of allogenic blood transfusion to be significantly greater in patients with sub-fascial drains (8). No other study assessed the association between the use of subfascial drains and the need for allogeneic blood transfusions in spine fusion surgery. Our study demonstrated that patients who had a subfascial drain placed at the time of a multi-level ACDF procedure required a statistically significant greater number of postoperative allogenic blood transfusion (P=0.04), and that drain use was the sole independent predictor of a patient needing an allogenic blood transfusion postoperatively. Likewise, our study found that patients with subfascial drains placed at the time of surgery had a statistically significant longer LOS as compared to patients with no drains (P<0.0001).
This study has limitations, which has implications for its interpretation. First, our small sample size of patients with a documented SSI limits our ability to make any firm conclusions. Second, it was not known whether the decision to transfuse was mainly driven by the patients’ clinical picture or provider preferences. Our study was performed a single institution and the utilization of the different approaches as well as the surgical technique are subject to the bias of individual surgeons. Although pre- and perioperative variables were prospectively recorded into the study registry at the time of surgery, these variables were retrospectively analyzed for the purposes of this study and as such are subject to the pitfalls associated with all retrospective reviews. Despite these limitations, this study demonstrates that the use of subfascial drains following multi-level ACDFs did not significantly impact the incidence of SSIs or hematoma, but rather increased the length of hospital stay, and the need for transfusion.
Conclusions
The use of subfascial drains after multi-level ACDF procedures were not associated with a decreased incidence of hematoma formation or SSI’s. In fact, patients in which a subfascial drain was used were 14 times more likely to require a post-operative blood transfusion and with an almost 2-fold increase in the duration of in-hospital stay.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional review board approval was obtained before study initiation (Rush Medical Center IRB 17021801-IRB01-AM04).
References
- Kanayama M, Oha F, Togawa D, et al. Is closed-suction drainage necessary for single-level lumbar decompression?: review of 560 cases. Clin Orthop Relat Res 2010;468:2690-4. [Crossref] [PubMed]
- Scuderi GJ, Brusovanik GV, Fitzhenry LN, et al. Is wound drainage necessary after lumbar spinal fusion surgery? Med Sci Monit 2005;11:CR64-6. [PubMed]
- Brown MD, Brookfield KF. A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine (Phila Pa 1976) 2004;29:1066-8. [Crossref] [PubMed]
- Payne DH, Fischgrund JS, Herkowitz HN, et al. Efficacy of closed wound suction drainage after single-level lumbar laminectomy. J Spinal Disord 1996;9:401-3. [Crossref] [PubMed]
- Blank J, Flynn JM, Bronson W, et al. The use of postoperative subcutaneous closed suction drainage after posterior spinal fusion in adolescents with idiopathic scoliosis. J Spinal Disord Tech 2003;16:508-12. [Crossref] [PubMed]
- Rao SB, Vasquez G, Harrop J, et al. Risk factors for surgical site infections following spinal fusion procedures: a case-control study. Clin Infect Dis 2011;53:686-92. [Crossref] [PubMed]
- Diab M, Smucny M, Dormans JP, et al. Use and outcomes of wound drain in spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012;37:966-73. [Crossref] [PubMed]
- Walid MS, Abbara M, Tolaymat A, et al. The role of drains in lumbar spine fusion. World Neurosurg 2012;77:564-8. [Crossref] [PubMed]
- Basques BA, Bohl DD, Golinvaux NS, et al. Factors predictive of increased surgical drain output after anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2014;39:728-35. [Crossref] [PubMed]
- Mirzai H, Eminoglu M, Orguc S. Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech 2006;19:171-7. [Crossref] [PubMed]
- Samraj K, Gurusamy KS. Wound drains following thyroid surgery. Cochrane Database Syst Rev 2007. [PubMed]
- Tabaqchali MA, Hanson JM, Proud G. Drains for thyroidectomy/parathyroidectomy: fact or fiction? Ann R Coll Surg Engl 1999;81:302-5. [PubMed]
- Shandilya M, Kieran S, Walshe P, et al. Cervical haematoma after thyroid surgery: management and prevention. Ir Med J 2006;99:266-8. [PubMed]
- Choi HK, Law S, Chu KM, et al. The value of neck drain in esophageal surgery: a randomized trial. Dis Esophagus 1998;11:40-2. [Crossref] [PubMed]
- Parker MJ, Livingstone V, Clifton R, et al. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev 2007. [PubMed]
- Zhou XD, Li J, Xiong Y, et al. Do we really need closed-suction drainage in total hip arthroplasty? A meta-analysis. Int Orthop 2013;37:2109-18. [Crossref] [PubMed]
- Ritter MA, Keating EM, Faris PM. Closed wound drainage in total hip or total knee replacement. A prospective, randomized study. J Bone Joint Surg Am 1994;76:35-8. [Crossref] [PubMed]
- Beer KJ, Lombardi AV Jr, Mallory TH, et al. The efficacy of suction drains after routine total joint arthroplasty. J Bone Joint Surg Am 1991;73:584-7. Erratum in: J Bone Joint Surg Am 1991;73:791. [Crossref] [PubMed]
- Hadden WA, McFarlane AG. A comparative study of closed-wound suction drainage vs. no drainage in total hip arthroplasty. J Arthroplasty 1990;5 Suppl:S21-4. [Crossref] [PubMed]
- Reilly TJ, Gradisar IA Jr, Pakan W, et al. The use of postoperative suction drainage in total knee arthroplasty. Clin Orthop Relat Res 1986.238-42. [PubMed]
- Cobb JP. Why use drains? J Bone Joint Surg Br 1990;72:993-5. [Crossref] [PubMed]
- Lang GJ, Richardson M, Bosse MJ, et al. Efficacy of surgical wound drainage in orthopaedic trauma patients: a randomized prospective trial. J Orthop Trauma 1998;12:348-50. [Crossref] [PubMed]
- Waly F, Alzahrani MM, Abduljabbar FH, et al. The Outcome of Using Closed Suction Wound Drains in Patients Undergoing Lumbar Spine Surgery: A Systematic Review. Global Spine J 2015;5:479-85. [Crossref] [PubMed]


