
Post-operative drain use in patients undergoing decompression and fusion: incidence of complications and symptomatic hematoma
Introduction
Placement of post-operative incisional drains following spinal surgery is a controversial topic, and its utilization has varied over time (1). Periprosthetic closed drains are widely utilized in other surgical subspecialties (2-9) with objective of minimizing hematoma formation and surgical site infections (SSI). In spinal surgery, the use of closed, high or low pressure drain alternatives are believed to attenuate persistent wound drainage, infection, and hematoma formation in the post-operative setting (10-13).
Despite being widely used, the effectiveness of drains in decreasing post-operative hematoma formation and infection has been recently been called into question (14-19). A few studies have shown no difference in clinical outcomes and complications profile with and without drain use (10,14-17,20-26). Others have suggested that drain placement negatively impacts outcomes leading to significantly greater use of allogenic blood transfusions, post-hemorrhagic anemia (26) as well as prolonged length of hospital stay (LOS) (19). Given the recent shifts in intraoperative protocols toward use of other infection-control measures such as locally applied vancomycin powder (27-31), further studies into the effectiveness of subfascial drains in reducing post-operative infections and hematoma formation are warranted.
The aim of this study is to determine whether there is a difference in the rate of postoperative SSI or hematoma formation between spine deformity patients undergoing spinal decompression and fusion with and without the use of a postoperative subfascial drain.
Methods
The medical records of 139 adult patients (≥18 years old) with spinal deformity undergoing elective spinal decompression and fusion at a major academic institution were reviewed. Institutional Review Board approval was obtained prior to initiation of this study. Inclusion criteria included patients (I) with available demographics and treatment data; (II) who underwent elective decompression and fusion; and (III) had presence or absence of a drain documented on medical records. We identified 139 patients (83%) who had a post-operative drain placed and 23 (17%) who did not. The primary outcome investigated in this study was the incidence of post-operative complications, specifically SSIs and hematoma formation.
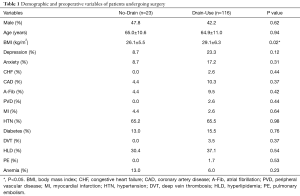
Demographic variables evaluated included patient age, gender, and body mass index (BMI). Comorbidities included depression, anxiety, congestive heart failure (CHF), coronary artery disease (CAD), atrial fibrillation (A-Fib), peripheral vascular disease (PVD), myocardial infarction (MI), hypertension (HTN), diabetes, deep vein thrombosis (DVT), hyperlipidemia (HLD), pulmonary embolism (PE), and anemia.
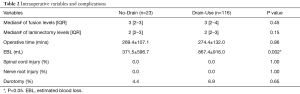
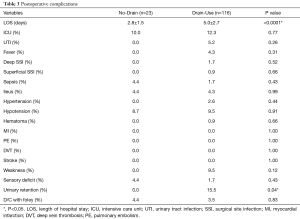
Operative variables included LOS, median fusion levels, and estimated blood loss (EBL). Intraoperative complications included incidence of spinal cord injury, nerve root injury, and durotomy. Postoperative complications included urinary tract infection (UTI), fever, deep and superficial SSI, sepsis, ileus, hematoma, MI, PE, DVT, stroke, motor weakness or sensory deficit
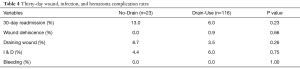
All cause re-admission within 30 days of discharge was assessed on all patients. Thirty-day complications included wound dehiscence, draining wound, incision & drainage (I & D), and bleeding.
Parametric data were expressed as means ± standard deviation (SD) and compared using the Student t-test. Nonparametric data were expressed as median (interquartile range) and compared via the Mann-Whitney U test. Nominal data were compared with the χ2 test. All tests were 2-sided and were statistically significant if the P value was less than 0.05. Statistical analysis was performed using JMP, version 13 (SAS Institute Inc., Cary, North Carolina, USA).
Results
There were no significant differences in baseline demographics between both groups. The average age and proportion of male participants were similar between both groups, P=0.94 and 0.62, respectively (Table 1). The mean BMI was significantly higher in the drain-use cohort (No-Drain: 26.1±5.5 kg/m2vs. Drain-Use: 29.1±6.3 kg/m2, P=0.02) (Table 1). There were no significant differences between both groups in prevalence of other comorbidities such as depression, anxiety, CHF, CAD, A-Fib, PVD, MI, HTN, diabetes, DVT, HLD, PE, and anemia (Table 1).
Full table
The median number of levels fused were similar between both groups {No-Drain: 3 [2–3] vs. Drain-Use: 3 [2–4], P=0.45} (Table 2). There was no significant difference in operative time between the cohorts (269.4±107.1 vs. 274.4±132.0 minutes, P=0.86) (Table 2). Compared to the No-Drain cohort, the Drain-Use cohort had significantly higher intraoperative blood loss (No-Drain: 371.5±596.7 vs. Drain-Use: 867.4±916.0 mL, P=0.002) (Table 2). Both cohorts had similar rates of incidental intraoperative durotomy (No-Drain: 4.4% vs. Drain-Use: 6.9%, P=0.65), while neither group had an incidence of spinal cord or nerve root injuries (Table 2).
Full table
Post-operative hospital stay and complication profile
Post-operative hospital stay was significantly higher for the Drain-Use cohort compared to the No-Drain cohort (No-Drain: 2.8±1.5 days vs. Drain-Use: 5.0±2.7 days, P<0.0001) (Table 3). The post-operative complication profile was similar between both cohorts, and notably, there were no significant differences in deep SSI (No-Drain: 0.0% vs. Drain-Use: 1.7%, P=0.52), superficial SSI (No-Drain: 0.0% vs. Drain-Use: 0.9%; P=0.66), and incidence of hematoma formation (No-Drain: 0.0% vs. Drain-Use: 0.9%; P=0.66), Table 3. The prevalence of post-operative complications were similar between both cohorts (No-Drain vs. Drain-Use)—ICU transfer (10.0 vs. 12.3, P=0.77), UTI (0.0 vs. 5.2, P=0.26), fever (0.0 vs. 4.3, P=0.31), sepsis (4.4 vs. 1.7, P=0.43), ileus (4.4 vs. 4.3, P=0.99), HTN (0.0 vs. 2.6, P=0.44), hypotension (8.7 vs. 9.5, P=0.91), weakness (0.0 vs. 9.5, P=0.12), or transient sensory deficit (4.4 vs. 1.7, P=0.43) (Table 3), while neither cohorts had any incidence of MI, PE, DVT, or stroke.
Full table
Thirty-day readmission rates were similar between both cohorts (No Drain: 13.0% vs. Drain-Use: 6.0%, P=0.23) (Table 4). Additionally, there were no significant differences in prevalence of 30-day wound dehiscence (No-Drain: 0.0% vs. Drain-Use: 0.9%, P=0.66), draining wound (No-Drain: 8.7% vs. Drain-Use: 3.5%; P=0.26), or I & D (No-Drain: 4.4% vs. Drain-Use: 6.0%, P=0.75) between both cohorts (Table 4).
Full table
Discussion
In this retrospective study of 139 patients who underwent elective thoracolumbar decompression with fusion, we reported similar incidence of SSI and hematoma formation with and without the use of postoperative subfascial drain.
Subfascial drains have been employed across the surgical spectrum to encourage wound healing, minimize wound discharge, and reduce the risk of infection (10,32). This practice is especially common following spinal surgery, as many associate drain placements with prevention of postoperative hematoma and its neurological sequelae (1,33). Decisions about drain placement are based mainly on surgeon preference and not guided by scientific evidence (14). In a meta-analysis of 36 studies and 5,464 patients, comparing closed suction drainage systems to no drains, Parker et al. reported that there is insufficient evidence from randomized clinical trials to support the routine use of closed suction drainage (24). Furthermore, the authors found no differences in wound infection, hematoma formation, and dehiscence rates between patients who received closed suction drains and those who did not (24). Similarly, in a meta-analysis for five studies analyzing closed suction wound drainage after lumbar spine surgery, Liu et al. demonstrated no significant reductions in the incidence rate of wound infections, hematoma formation, or reoperations associated with drain use (33). Furthermore, the authors demonstrated that drain use was associated with higher intra-operative blood loss and incidence of blood transfusions (33).
A few studies have shown no change in the incidence of post-operative SSI’s with the use of subfascial drains. In a retrospective study of 560 patients undergoing lumbar decompression, Kanayama et al. found that the risk of post-operative wound infection and hematoma formation was not influenced by use of post-operative subfascial drains (17). Walid et al. reported no difference in post-operative infection risk with the use of subfascial drains; and in fact noted an increased risk of post-operative anemia in patients with post-operative subfascial drains (26). Scuderi et al. in a study of 83 patients undergoing posterior lumbar fusion found no difference in hematoma formation between groups of patients with and without post-operative subfascial drains. Similarly, in a prospective, randomized study, Hung et al. demonstrated that duration of time from surgery to ambulation was significantly shorter in the cohort of patients who did not have a closed suction wound drain placed (34). Analogous to these aforementioned studies, our findings report no significant differences in SSI rates and rate of hematoma formation between patients who did and did not receive a closed-suction drainage system.
In contrast, a few studies that have shown benefit with use of post-operative subfascial drains. In a retrospective analysis of 126 patients that underwent posterior instrumented fusion, Ho et al. (12) found the use of subfascial drains were associated with a significantly lower risk of delayed hematoma formation (12). Blank et al., in a prospective study of 30 adolescent patients undergoing posterior spinal fusion for progressive idiopathic scoliosis, demonstrated that the use of a closed suction drainage system decreased wound complications without significantly increasing the need for blood transfusion in the postoperative setting (35). In another a study Sen et al. reported that use of closed-suction drains led to a reduction in radiographically-evident post-operative epidural fibrosis and improved patient-reported outcomes (36). Lastly, in a prospective, randomized clinical study of 50 patients undergoing lumbar disc surgery, Mirzai et al. demonstrated an incidence rate of epidural hematoma to be lower in patients with a postoperative drain than those without (36% vs. 89%) (37). Contrary to these studies, we observed no difference in post-operative complications with or without the use of indwelling drains.
Routine use of subfascial drains are associated with prolonged hospital stay, increased healthcare resource utilization and costs. In a retrospective analysis of 81 patients who underwent one and two-level cervical spinal fusion, Poorman et al. demonstrated that patients with postoperative wound drains experienced significantly longer LOS when compared to patients without a drain (38.9 vs. 31.7 hours, P=0.021) (19). In case-control study of 1,587 patients undergoing spinal fusion, Rao et al. demonstrated a directly proportional relationship between the duration of drain use and occurrence of a SSI (unit odds-ratio, 2.1; 95% CI, 1.6–3.1) (38). Similarly, in another case-control study of 5,473 adult patients undergoing spinal fusion, Walsh et al. demonstrated an increased risk of SSI’s and healthcare resource utilization in patients with post-operative indwelling drains (39).
This study has limitations with potential implications for its interpretation. Our sample size is small, thereby limiting our ability to make any firm conclusions. Though preoperative and perioperative variables were prospectively recorded at the time of surgery, these variables were retrospectively analyzed and are subject to the weaknesses of retrospective reviews. Patient comorbidities, including presence of coagulopathies or use of pre-operative anti-coagulation, which could have influenced post-operative hematoma formation were not studied and could have influenced results. Despite these limitations, we demonstrate that there are no significant differences in postoperative SSI or hematoma formation in patients undergoing lumbar decompression and fusion with and without closed suction drain placement.
Conclusions
Our study suggests that the use of postoperative subfascial drains in patients undergoing spinal decompression with fusion may not be associated with a reduction in SSIs or hematoma formation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board approval was obtained prior to initiation of this study. Informed consent was not required since this was a retrospective chart review.
References
- von Eckardstein KL, Dohmes JE, Rohde V. Use of closed suction devices and other drains in spinal surgery: results of an online, Germany-wide questionnaire. Eur Spine J 2016;25:708-15. [Crossref] [PubMed]
- McCarthy CM, Disa JJ, Pusic AL, et al. The effect of closed-suction drains on the incidence of local wound complications following tissue expander/implant reconstruction: a cohort study. Plast Reconstr Surg 2007;119:2018-22. [Crossref] [PubMed]
- Scevola S, Youssef A, Kroll SS, et al. Drains and seromas in TRAM flap breast reconstruction. Ann Plast Surg 2002;48:511-4. [Crossref] [PubMed]
- Youssef F, Jenkins MP, Dawson KJ, et al. The value of suction wound drain after carotid and femoral artery surgery: a randomised trial using duplex assessment of the volume of post-operative haematoma. Eur J Vasc Endovasc Surg 2005;29:162-6. [Crossref] [PubMed]
- Krishnamoorthy B, Al-Fagih OS, Madi MI, et al. Closed suction drainage improves clinical outcome in patients undergoing endoscopic vein harvesting for coronary artery bypass grafting. Ann Thorac Surg 2012;93:1201-5. [Crossref] [PubMed]
- Dora C, von Campe A, Mengiardi B, et al. Simplified wound care and earlier wound recovery without closed suction drainage in elective total hip arthroplasty. A prospective randomized trial in 100 operations. Arch Orthop Trauma Surg 2007;127:919-23. [Crossref] [PubMed]
- Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total hip arthroplasties. J Arthroplasty 1998;13:156-61. [Crossref] [PubMed]
- Diaz JJ Jr, Cullinane DC, Dutton WD, et al. The management of the open abdomen in trauma and emergency general surgery: part 1-damage control. J Trauma 2010;68:1425-38. [Crossref] [PubMed]
- Lawal YZ, Ogirima MO, Dahiru IL, et al. On the use of drains in orthopedic and trauma. Niger J Clin Pract 2014;17:366-9. [Crossref] [PubMed]
- Brown MD, Brookfield KF. A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine (Phila Pa 1976) 2004;29:1066-8. [Crossref] [PubMed]
- Scuderi GJ, Brusovanik GV, Fitzhenry LN, et al. Is wound drainage necessary after lumbar spinal fusion surgery? Med Sci Monit 2005;11:CR64-6. [PubMed]
- Ho C, Sucato DJ, Richards BS. Risk factors for the development of delayed infections following posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976) 2007;32:2272-7. [Crossref] [PubMed]
- Durai R, Ng PC. Surgical vacuum drains: types, uses, and complications. AORN J 2010;91:266-71. [Crossref] [PubMed]
- Andrew Glennie R, Dea N, Street JT. Dressings and drains in posterior spine surgery and their effect on wound complications. J Clin Neurosci 2015;22:1081-7. [Crossref] [PubMed]
- Zijlmans JL, Buis DR, Verbaan D, et al. Wound drains in non-complex lumbar surgery: a systematic review. Bone Joint J 2016;98-B:984-9. [Crossref] [PubMed]
- Waly F, Alzahrani MM, Abduljabbar FH, et al. The Outcome of Using Closed Suction Wound Drains in Patients Undergoing Lumbar Spine Surgery: A Systematic Review. Global Spine J 2015;5:479-85. [Crossref] [PubMed]
- Kanayama M, Oha F, Togawa D, et al. Is closed-suction drainage necessary for single-level lumbar decompression?: review of 560 cases. Clin Orthop Relat Res 2010;468:2690-4. [Crossref] [PubMed]
- Kogure K, Node Y, Tamaki T, et al. Indwelling Drains Are Not Necessary for Patients Undergoing One-level Anterior Cervical Fixation Surgery. J Nippon Med Sch 2015;82:124-9. [Crossref] [PubMed]
- Poorman CE, Passias PG, Bianco KM, et al. Effectiveness of postoperative wound drains in one- and two-level cervical spine fusions. Int J Spine Surg 2014.8. [PubMed]
- Patel SB, Griffiths-Jones W, Jones CS, et al. The current state of the evidence for the use of drains in spinal surgery: systematic review. Eur Spine J 2017;26:2729-38. [Crossref] [PubMed]
- Kou J, Fischgrund J, Biddinger A, et al. Risk factors for spinal epidural hematoma after spinal surgery. Spine (Phila Pa 1976) 2002;27:1670-3. [Crossref] [PubMed]
- Ahn DK, Kim JH, Chang BK, et al. Can We Prevent a Postoperative Spinal Epidural Hematoma by Using Larger Diameter Suction Drains? Clin Orthop Surg 2016;8:78-83. [Crossref] [PubMed]
- Uribe J, Moza K, Jimenez O, et al. Delayed postoperative spinal epidural hematomas. Spine J 2003;3:125-9. [Crossref] [PubMed]
- Parker MJ, Livingstone V, Clifton R, et al. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev 2007. [PubMed]
- Diab M, Smucny M, Dormans JP, et al. Use and outcomes of wound drain in spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2012;37:966-73. [Crossref] [PubMed]
- Walid MS, Abbara M, Tolaymat A, et al. The role of drains in lumbar spine fusion. World Neurosurg 2012;77:564-8. [Crossref] [PubMed]
- Bakhsheshian J, Dahdaleh NS, Lam SK, et al. The use of vancomycin powder in modern spine surgery: systematic review and meta-analysis of the clinical evidence. World Neurosurg 2015;83:816-23. [Crossref] [PubMed]
- Khan NR, Thompson CJ, DeCuypere M, et al. A meta-analysis of spinal surgical site infection and vancomycin powder. J Neurosurg Spine 2014;21:974-83. [Crossref] [PubMed]
- Lee GI, Bak KH, Chun HJ, et al. Effect of Using Local Intrawound Vancomycin Powder in Addition to Intravenous Antibiotics in Posterior Lumbar Surgery: Midterm Result in a Single-Center Study. Korean J Spine 2016;13:47-52. [Crossref] [PubMed]
- Sweet FA, Roh M, Sliva C. Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions: efficacy, drug levels, and patient outcomes. Spine (Phila Pa 1976) 2011;36:2084-8. [Crossref] [PubMed]
- Molinari RW, Khera OA, Molinari WJ 3rd. Prophylactic intraoperative powdered vancomycin and postoperative deep spinal wound infection: 1,512 consecutive surgical cases over a 6-year period. Eur Spine J 2012;21 Suppl 4:S476-82. [Crossref] [PubMed]
- Varley GW, Milner SA. Wound drains in proximal femoral fracture surgery: a randomized prospective trial of 177 patients. J R Soc Med 1995;88:42P-4P. [PubMed]
- Liu JM, Chen WZ, Fu BQ, et al. The Use of Closed Suction Drainage in Lumbar Spinal Surgery: Is It Really Necessary? World Neurosurg 2016;90:109-15. [Crossref] [PubMed]
- Hung PI, Chang MC, Chou PH, et al. Is a drain tube necessary for minimally invasive lumbar spine fusion surgery? Eur Spine J 2017;26:733-7. [Crossref] [PubMed]
- Blank J, Flynn JM, Bronson W, et al. The use of postoperative subcutaneous closed suction drainage after posterior spinal fusion in adolescents with idiopathic scoliosis. J Spinal Disord Tech 2003;16:508-12. [Crossref] [PubMed]
- Sen O, Kizilkilic O, Aydin MV, et al. The role of closed-suction drainage in preventing epidural fibrosis and its correlation with a new grading system of epidural fibrosis on the basis of MRI. Eur Spine J 2005;14:409-14. [Crossref] [PubMed]
- Mirzai H, Eminoglu M, Orguc S. Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech 2006;19:171-7. [Crossref] [PubMed]
- Rao SB, Vasquez G, Harrop J, et al. Risk factors for surgical site infections following spinal fusion procedures: a case-control study. Clin Infect Dis 2011;53:686-92. [Crossref] [PubMed]
- Walsh TL, Querry AM, McCool S, et al. Risk Factors for Surgical Site Infections Following Neurosurgical Spinal Fusion Operations: A Case Control Study. Infect Control Hosp Epidemiol 2017;38:340-7. [Crossref] [PubMed]


